Abstracts
BACKGROUND: Psychological factors such as stress and depression have already been established as risk factors for cardiovascular disease. More recently, the impact of anxiety has been addressed. OBJECTIVE: To identify psychiatric disorders and assess health- and cardiac-related anxiety in coronary artery disease patients attending a supervised exercise program. METHODS: Forty-two male cardiac patients were interviewed using the Mini International Neuropsychiatric Interview (MINI) version 5.0 and instructed to complete the Anxiety Sensitivity Index, the Agoraphobic Cognitions Questionnaire, the Body Sensations Scale, and the Cardiac Anxiety Questionnaire. RESULTS: Thirty-eight percent of the participants presented with one or more psychiatric disorders (PDs) but only 19% presented with multiple PDs. Psychiatric disorders were associated with higher health- and cardiac-related anxiety scores (p < 0.05). No relationship was found between these anxiety scores and the severity of cardiovascular disease (p > 0.05). DISCUSSION: Health-related anxiety seems to be more strongly associated with the presence of psychiatric comorbidities in cardiac patients than with the severity of cardiovascular disease. Screening of all cardiac patients for past and present psychiatric symptoms should be implemented. Interventional strategies, including exercise and counseling, warrant further research.
Anxiety; psychiatric disorders; cardiac anxiety; coronary artery disease; rehabilitation
CONTEXTO: Aspectos psicológicos como estresse e depressão já são reconhecidos como fatores de risco cardiovascular. Mais recentemente, o impacto da ansiedade passou a ser objeto de estudo. OBJETIVO: Identificar a prevalência de transtornos psiquiátricos e a presença de ansiedade relacionada à saúde e de ansiedade cardíaca em coronariopatas participantes de um programa de exercício supervisionado. MÉTODOS: Quarenta e dois homens coronariopatas foram entrevistados com o Mini International Neuropsychiatric Interview (MINI), versão 5.0, e solicitados a preencher a Escala de Sensibilidade à Ansiedade, o Questionário de Cognições Agorafóbicas, a Escala de Sensações Corporais e o Questionário de Ansiedade Cardíaca. RESULTADOS: Dentre os participantes, 38% apresentaram um ou mais diagnósticos psiquiátricos pelo MINI, mas apenas 19% apresentaram múltiplas comorbidades. A presença de transtornos psiquiátricos encontra-se associada a escores mais altos de ansiedade relacionada à saúde e à ansiedade cardíaca (p < 0,05). Não foi encontrada relação entre os escores de ansiedade e a gravidade da doença cardiovascular (p > 0,05). CONCLUSÕES: Ansiedade relacionada à saúde parece estar mais fortemente associada à presença de comorbidades psiquiátricas do que à gravidade do quadro cardiovascular. Recomenda-se a triagem regular de pacientes coronariopatas para transtornos psiquiátricos. Estratégias terapêuticas complementares como exercício físico e psicoterapia podem ser alternativas terapêuticas complementares.
Ansiedade; transtornos psiquiátricos; ansiedade cardíaca; doença arterial coronariana; reabilitação
ORIGINAL ARTICLE
IClinical Psychologist. Laboratory of Panic and Respiration Institute of Psychiatry - Federal University of Rio de Janeiro (UFRJ)
IIGraduate Program in Physical Education from Gama Filho University
IIIAdjunct professor of the Universidade Federal Fluminense (UFF)
IVAssociate professor of Medical School, Psychiatry Institute (IPUB)/UFRJ
Address correspondence to
ABSTRACT
BACKGROUND: Psychological factors such as stress and depression have already been established as risk factors for cardiovascular disease. More recently, the impact of anxiety has been addressed.
OBJECTIVE: To identify psychiatric disorders and assess health- and cardiac-related anxiety in coronary artery disease patients attending a supervised exercise program.
METHODS: Forty-two male cardiac patients were interviewed using the Mini International Neuropsychiatric Interview (MINI) version 5.0 and instructed to complete the Anxiety Sensitivity Index, the Agoraphobic Cognitions Questionnaire, the Body Sensations Scale, and the Cardiac Anxiety Questionnaire.
RESULTS: Thirty-eight percent of the participants presented with one or more psychiatric disorders (PDs) but only 19% presented with multiple PDs. Psychiatric disorders were associated with higher health- and cardiac-related anxiety scores (p < 0.05). No relationship was found between these anxiety scores and the severity of cardiovascular disease (p > 0.05).
DISCUSSION: Health-related anxiety seems to be more strongly associated with the presence of psychiatric comorbidities in cardiac patients than with the severity of cardiovascular disease. Screening of all cardiac patients for past and present psychiatric symptoms should be implemented. Interventional strategies, including exercise and counseling, warrant further research.
Keywords: Anxiety, psychiatric disorders, cardiac anxiety, coronary artery disease, rehabilitation.
Introduction
Psychiatric conditions have long been studied in cardiac patients1. Depression is currently considered to not only be an associated condition but also an independent risk factor for the development of coronary artery disease (CAD)2. More recently, studies have pointed out the concurrence of anxiety disorders3, notably panic disorder4 and health-related anxiety5, in CAD patients. These studies suggest that panic attacks can lead to a poorer clinical prognosis and myocardial perfusion deficits even in clinically stable patients6.
Not only may psychiatric disorders (PD) such as depression and anxiety contribute to impaired functioning7 for patients with CAD, but they may also represent an additional risk. Additionally, depression and anxiety have been shown to be predictive factors for cardiac rehabilitation drop-out8 and lower adherence to pharmacological treatment9. The actual prevalence of these psychiatric comorbidities has not been determined in CAD patients participating in exercise programs, which can be considered a subset of CAD patients with very particular characteristics. The present study aimed to identify PDs and assess health-related anxiety (HRA) and cardiac-related anxiety (CA) in CAD patients regularly attending a supervised exercise program.
Methods
Forty-two male CAD patients attending a medically-supervised cardiac rehabilitation exercise program were interviewed to identify PDs and to assess HRA and CA in a cross-sectional observation. The program was hosted at a private clinic where patients were referred by their cardiologists for cardiac rehabilitation. Typical exercise sessions consisted of 20-30 minutes of aerobic exercise on treadmills and upper and lower limb cyclergometers followed by 20-30 minutes of resistance training and stretching exercises.
Participants were attendees with a formal diagnosis of CAD documented by history of myocardial infarction or coronary artery revascularization procedures or by the presence of significant obstructive coronary lesions evidenced by angiography. Inclusion criteria were agreement to participate, regular compliance with the supervised exercise program (attendance at a minimum of 75% of the sessions), and a well-established diagnosis of CAD as the primary medical condition. Exclusion criteria were refusal to participate and the presence of any other major medical condition, such as cancer, neurological problems, or psychotic disorders. Individual medical data were obtained by review of medical files.
After volunteering to participate and reading and signing an informed consent document, patients went through a structured interview designed to explore each of the necessary criteria for the main DSM-IV Axis I diagnoses [the Mini International Neuropsychiatric Interview (MINI) version 5.0]10. Data collection occurred for each participant individually, either before or immediately after the exercise session in a separate room in the clinic. All data collection was performed by the same trained researcher (A.S.).
Subjects were later requested to fill in the following self-report instruments in order to investigate HRA and CA: the Anxiety Sensitivity Index (ASI)11, the Agoraphobic Cognitions Questionnaire (ACQ)12, the Body Sensations Scale (BSS)12, and the Cardiac Anxiety Questionnaire (CAQ)13. The ASI is a 36-item inventory that evaluates the extent to which a person believes that anxiety-related sensations can be catastrophic. The ACQ has 14 items regarding thoughts that occur when the person experiences anxiety. The BBS has 17 items and describes body sensations that can potentially elicit anxiety. Finally, the CAQ is an 18-item instrument designed to evaluate how threatening the subject considers the experienced cardiac symptoms. All measures were Likert-type self report instruments, and Brazilian Portuguese validated versions were used14-17.
Psychiatric disorders were assessed in terms of present and lifetime prevalence and described in terms of frequency. To assess differences in the scores of HRA and CA, patients were later divided into subgroups relative to the presence/absence of a PD and a history of acute myocardial infarction (AMI). Inferential analysis of the mean differences between the standardized scores of the questionnaires was carried out by t-tests and ANOVAs, followed by Bonferroni post-hoc analysis as needed. A significance level of .05 was established. All statistical analyses were carried out by GraphPad Prism version 5.0. The present study was approved by the Rio de Janeiro Federal University Research Ethics Committee.
Results
Demographic and clinical data
Participants were 42 men (Tolerable Error = 0.08; 95% confidence interval) aged from 46 to 89 years (69 ± 9.7; mean ± SD). All subjects had a minimum of eight years of education and belonged to upper socioeconomic strata. According to their medical records, 35 (83%) patients attended the supervised exercise program three times a week, while 7 (17%) participated four to six times a week. Average time of participation in the program was 19.5 months (SD = 11.1).
Fifty percent (n = 21) of the patients had at least one AMI, while 45% (n = 19) had received coronary artery bypass grafts, and 60% (n = 25) had undergone at least one percutaneous transluminal coronary angioplasty. In addition, 69% (n = 29) of the patients had a diagnosis of arterial hypertension, 64% (n = 27) had dyslipidemia, and 7% (n = 3) currently smoked. Other clinical comorbidities reported included asthma (n = 1), hypotiroidism (n = 1), history of stroke (n = 2), atrial fibrillation (n = 2), mitral insufficiency (n = 1), abdominal aortic endoprotesis (n = 2) and carotid endarterectomy (n = 2). Data on current medication use were not reliably available on the medical files.
Prevalence of psychiatric disorders
Sixteen participants (38%) met the criteria for at least one PD as assessed by the MINI (Table 1). Eight patients (19%) presented with multiple PDs. In these patients, a past depression episode was found to be the most commonly identified disorder (n = 7; 17%) followed by agoraphobia (n = 6; 14%) and social phobia (n = 6; 14%).
From the entire sample, only three patients (7%) were currently seeing a psychiatrist for outpatient clinical treatment. In spite of that, 26% (n = 11) reported taking benzodiazepines whenever anxious, stressed, or having sleep difficulties. Patients reported that the benzodiazepines had been prescribed by their attending cardiologist or clinician in the past, to be taken whenever necessary. Only one patient claimed to currently being treated for anxiety by the cardiologist.
Concerning anxiety manifestations, 24% (n = 10) reported at least one anxiety disorder. Although no recent panic attacks were reported, four (10%) participants reported a history of panic attacks in the past. The most prevalent disorder identified was agoraphobia without current panic attacks (14%, n = 6). Social phobia was present in 14% (n = 6) of the subjects while generalized anxiety disorder was found in 2% (n = 1) of the patients, and specific phobias were reported by 5% (n = 2). Obsessive-compulsive disorder was not identified in this sample.
Lifetime prevalence of depressive episodes was 17% (n = 7) while only 5% (n = 2) met the criteria for a current major depressive episode. One patient had experienced a manic episode previously (2%), and another (2%) reported a hypomanic episode in the past. No dysthymia was found. The relative frequencies of each diagnostic criteria established by the MINI can be seen in table 1.
Health related anxiety and cardiac related anxiety
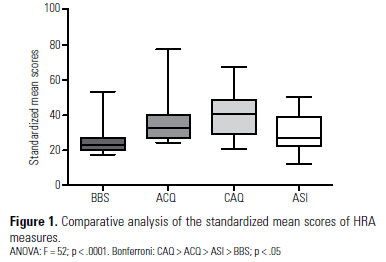
Analysis of variance (ANOVA) followed by Bonferroni post-hoc comparisons from standardized mean scores of the self-report instruments showed differences among indicators, with significantly higher scores in the CAQ followed by the ASI, the ACQ, and the BBS (Figure 1).
When patients were further divided into those with and without history of AMI, there were no significant differences in the mean scores of the HRA and CA questionnaires (Figure 2).
Mean scores of the health and CA questionnaires were significantly higher when CAD patients were separated according to the presence of psychiatric disorders. Significant differences were found between these two subgroups with all measures, as shown in figure 3.
Discussion
The high prevalence of current single or multiple PDs (38%) found in this particular subset of CAD patients confirms similar data from the literature1 and highlights the importance of considering the effects of psychiatric disorders among patients suffering from cardiac problems. As would be expected, CA was significantly more common than HRA, suggesting that patients with CAD tend to feel more anxious about cardiac symptoms as compared to other body sensations.
Despite the high psychiatric morbidity found in our study, patients were largely undertreated regarding these conditions with only three patients (7%) currently under psychiatric attention. Even those 26% that at some point had benzodiazepines prescribed by their attending cardiologist or clinician may not be receiving adequate psychiatric care. These results corroborate the importance of a more careful psychiatric screening of outpatients presenting with cardiac diseases. Psychiatric disorders, such as anxiety and depression, may be frequent and widely misdiagnosed in outpatient clinics. Likely, an early identification of these conditions could decrease the use of benzodiazepines in cardiac patients without any precise psychiatric diagnosis and lead to better treatment, health improvement, increased quality of life, and a decrease in the higher morbidity and mortality risk attributed to the association of cardiac disease and psychiatric illness2-5.
Although the prevalence described here was similar to that reported by others, the relatively low prevalence of multiple PDs (19%) is a discrepant outcome when compared to the rest of the literature. For instance, Bankier et al.1 found that most cardiac outpatients with a psychiatric diagnosis present with more than one psychiatric disorder. Other interesting results from the present study include the absence of participants with current panic attacks and the finding that the prevalence of current depressive episode and GAD in this study was far below that which is usually reported with self-report measures in patients with CAD2-4.
The low occurrence of present depressive episodes and the absence of panic attacks can be explained in two ways. It is intuitive to assume that severely depressed or anxious patients are less likely to regularly attend a cardiac rehabilitation program, which is a clear selection bias that limits any causality assumption to be derived from the present observation. On the other hand, there is abounding evidence regarding the ability of the serotonin-system to improve mood in depressed and healthy subjects who engage in regular exercise18. This protective and therapeutic effect of exercise on psychiatric conditions could explain the lower prevalence of multiple PDs, which is associated with a less severe presentation of psychiatric impairment and a better prognosis for these patients1. Another important factor is that the relatively low prevalence of depression may be influenced by the absence of women in the sample, as depression is far more prevalent in women after an AMI or coronary artery bypass surgery than in men in similar conditions19.
Concerning panic attacks, one could imagine that a person experiencing frequent panic attacks would probably develop an intense avoidance behavior that could interfere with adherence to an exercise-based rehabilitation program. Specifically, an exercise program can induce autonomic manifestations that are similar to anxiety symptoms experienced in the attacks and thus physical exercise would be specifically avoided20. Notwithstanding, it is also likely that regular exercise works as interoceptive exposure, promoting gradual desensitization to the feared autonomic symptoms and therefore reducing the frequency and intensity of panic attacks and even having a secondary impact on avoidance behavior. As a matter of fact, it has been demonstrated that regular exercise can reduce the likelihood of experiencing a panic attack21. Additionally, patients under treatment to PD present worse quality of life scores, compared to healthy controls, especially those with high levels of anxiety and agoraphobia22 and regular exercising could have a positively impact quality of life.
A very surprising result was the lack of a significant difference in HRA and CA between patients with AMI history when compared to those without previous AMI, as post-MI patients have been the main focus of attention in studies on PDs in cardiac patients5,9. This result suggests that all CAD patients, not only those that have experienced an acute event such as a myocardial infarction, would benefit from being regularly checked for PDs, HRA, and CA in order to reduce the potential harmful effects of persisting PDs, particularly anxiety.
Assessment of HRA and CA can be very important in the sense that persisting anxiety can impair functioning5, decrease quality of life8, and negatively impact cardiac disease prognosis2-5. Data in the current literature point to the relevance of the negative cardiac impact of PDs such as panic attacks6, depression, and anxiety2-7. Also, chronic HRA and CA can induce a sense of vulnerability and impaired management skills that can contribute to the onset of psychiatric conditions9. In patients with HFA, it is not enough to be assured by the clinician that the disease is under control. In these cases, the absence of adequate screening for psychiatric disorders such as panic or HFA symptoms may lead to increased health system utilization, for additional unnecessary medical examinations, due to anxiety23. It is also known that psychological problems secondary to a cardiac disease onset/event can negatively impact one's motivation to seek appropriate treatment and to adhere to treatment guidelines5. More specifically, behavioral compliance in cardiac rehabilitation programs can be affected and can be considered a significant cause of treatment drop-out24.
Even more interesting was the finding that HRA and CA were more strongly associated with the presence of any PD than with the severity of the cardiovascular condition. This has relevant clinical implications in that the high prevalence of PDs among cardiac patients and not the severity of the cardiac condition may be the actual factor associated with the high HRA and CA found in this population. The finding that any PD, not only depression (n = 4) or panic, that is associated with higher anxiety is also clinically relevant, as this may contribute, directly or indirectly, to impaired functioning, poor adherence to treatment, and more negative outcomes.
Some limitations present in this study shall be highlighted. The main limitations are that there was no comparison group to allow for investigation into the possibility of selection bias and that there was a relatively small number of participants. Further studies need to be held comparing subsets of CAD patients attending or not attending exercise programs in order to precisely determine the effect size of this type of regular exercise on the prevalence of PDs. Due to the limitations of this observational study, a firm conclusion cannot be drawn; however, the data presented here can add to the growing body of evidence corroborating the linkage between mental health and regular exercise.
Another point that deserves to be highlighted is the non-representativeness of the studied sample related to the cardiac patient population in Brazil, especially considering the socioeconomic and educational level of the participants. On the other hand, this sample can be considered representative of the cardiac individuals in Brazil that would actually have access to a private exercise-based cardiac rehabilitation program. Although there are some exercise based-rehabilitation programs offered in public hospitals, most of them are held in private institutions and therefore only available to upper economic level subjects. In this sense, the present sample can be considered to adequately represent the target population of cardiac rehabilitation participants.
Lastly, different clinical conditions were grouped as CAD and described in terms of frequency, but there were not enough subjects available to perform a reasonable multiple regression statistical analysis in order to isolate the individual contribution of each different disease. Most studies published previously reported psychiatric disorders in specific cardiovascular conditions, and the present study yielded similar outcomes in terms of general prevalence among subjects with different clinical diagnoses and severity. Adding to this observation is the finding that the severity of heart disease, here operationally defined as history of AMI, does not have a significant effect on HRA and CA. The results of this work point to the importance of psychiatric screening in all types of cardiac disorders.
Conclusion
The outcomes of this research show that PDs are still highly prevalent in cardiac patients who attend an elective supervising exercise program, although less severe in terms of impairment in functioning and regarding the presence of multiple comorbidities. It can be hypothesized that regular exercise has an impact on the onset of PDs after a cardiac event, due to its effect on mood and anxiety, especially HRA and CA. Another possibility is that physical activity can directly mediate the prevalence of some psychiatric conditions, such as panic attacks or depressive episodes.
Psychiatric comorbidities among CAD patients and after an acute coronary event continue to be an issue of great importance. Controlled interventional studies are needed to fully understand the nature of this problem, the pathophysiology by which it arises, its prognostic significance, the best method of treatment for both alleviation of symptoms and improvement in event-free survival, and a better estimate of the effect of regular attendance at supervised exercise programs on the prevalence of PDs in CAD patients.
References
- 1. Bankier B, Januzzi JL, Littman AB. The high prevalence of multiple psychiatric disorders in stable outpatients with coronary heart disease. Psychosom Med. 2004;66(5):645-50.
- 2. Frasure-Smith N, Lesperance F. Recent evidence linking coronary heart disease and depression. Can J Psychiatry. 2006;51(12):730-7.
- 3. Frasure-Smith N, Lesperance F. Depression and anxiety as predictors of 2-year cardiac events in patients with stable coronary artery disease. Arch Gen Psychiatry. 2008;65(1):62-71.
- 4. Katerndahl D. Panic & plaques: panic disorder & coronary artery disease in patients with chest pain. J Am Board Fam Pract. 2004;17(2):114-26.
- 5. Furze G, Lewin RJP, Murberg T, Bull P, Thompson DR. Does it matter what patients think? The relationship between changes in patients' beliefs about angina and their psychological and functional status. J Psychosom Res. 2005;59(5):323-9.
- 6. Fleet R, Lespérance F, Arsenault A, Gregoire J, Lavoie K, Laurin C, et al. Myocardial perfusion study of panic attacks in patients with coronary artery disease. Am J Cardiol. 2005;96(8):1064-8.
- 7. Jiang W, Kuchibhatla M, Cuffe MS, Christopher EJ, Alexander JD, Clary GL, et al. Prognostic value of anxiety and depression in patients with chronic heart failure. Circulation. 2004;110(22):3452-6.
- 8. Komorovsky R, Desideri A, Rozbowsky P, Sabbadin D, Celegon L, Gregori D. Quality of life and behavioral compliance in cardiac rehabilitation patients: a longitudinal survey. Int J Nurs Stud. 2008;45(7):979-85.
- 9. Johansson I, Swahn E, Strömberg A. Manageability, vulnerability and interaction: a qualitative analysis of acute myocardial infarction patients' conceptions of the event. Eur J Cardiovasc Nurs. 2007;6(3):184-91.
- 10. Sheehan D, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):34-57.
- 11. Taylor S, Cox BJ. An expanded anxiety sensitivity index: evidence for a hierarchic structure in a clinical sample. J Anxiety Dis. 1998;12(5);463-83.
- 12. Chambless DL, Caputo C, Bright P, Gallagher R. Assessment of fear in agoraphobics: the Body Sensations Questionnaire and the Agoraphobic Cognitions Questionnaire. J Consult Clin Psychol. 1984;52(6):1090-7.
- 13. Eifert GH, Thompson RN, Zvolensky MJ, Edwards K, Frazer NL, Haddad JW, et al. The Cardiac Anxiety Questionnaire: development and preliminary validity. Behav Res Ther. 2000;38(10):1039-53.
- 14. Amorim P. Mini International Neuropsychiatric Interview (MINI): validação de entrevista breve para diagnóstico de transtornos mentais. Rev Bras Psiquiatr. 2000;22(3):106-15.
- 15. Escocard MRPG. Propriedades psicométricas da Escala de Sensibilidade à Ansiedade Revisada. Psicol Clin. 2008;20(1):217.
- 16. Ito LM, Ramos RT. Escalas de avaliação clínica: transtorno de pânico. Rev Psiq Clín. 1998;25:294-302.
- 17. Sardinha A, Nardi AE, Eifert GH. Translation and cross-cultural adaptation of the Brazilian version of the Cardiac Anxiety Questionnaire. Rev Psiquiatr Rio Gd Sul. 2008:30(2):139-49.
- 18. Peluso MAM, Guerra de Andrade LH. Physical activity and mental health: the association between exercise and mood. Clinics. 2005;60(1):61-70.
- 19. Smoller JW, Pollack MH, Wassertheil-Smoller S, Jackson RD, Oberman A, Wong N, et al. Panic attacks and risk of incident cardiovascular events among postmenopausal women in the Women's Health Initiative Observational Study. Arch Gen Psychiatry. 2007;64(10):1153-60.
- 20. King ALS, Valença AM, Melo-Neto VL, Nardi AE. A importância do foco da terapia cognitivo-comportamental direcionado às sensações corporais no transtorno do pânico: relato de caso. Rev Psiq Clín. 2007;34(4):191-5.
- 21. Broocks A, Bandelow B, Pekrun G, George A, Meyer T, Bartmann U, et al. Comparison of aerobic exercise, clomipramine, and placebo in the treatment of panic disorder. Am J Psychiatry. 1998;155(5):603-9.
- 22. Melo-Neto VL, Valença AM, Nascimento I, Lopes FL, Nardi AE. Quality of life assessment by WHOQOL-BREF in panic disorder patients during treatment. Rev Psiq Clín. 2008;35(2):49-54.
- 23. Soares-Filho GLF, Valença AM, Nardi AE. Dor torácica no transtorno de pânico: sintoma somático ou manifestação de doença arterial coronariana? Rev Psiq Clín. 2007;34(2):97-101.
- 24. Yohannes AM, Yalfani A, Doherty P, Bundy C. Predictors of drop-out from an outpatient cardiac rehabilitation programme. Clin Rehabil. 2007;21(3):222-9.
Prevalence of psychiatric disorders and health-related anxiety in cardiac patients
Publication Dates
-
Publication in this collection
18 May 2011 -
Date of issue
2011
History
-
Received
26 Apr 2010 -
Accepted
26 July 2010