Abstract
Paper aims
This article aims to evaluate the impact of Lean Production (LP) practices implementation on the supply chain of a public hospital.
Originality
Most implementations fall short of their goals because they are done in a fragmented way and not from a system-wide perspective. Our approach allows to anticipate errors of misguided LP implementations in healthcare organizations.
Research method
The implementation of a set of LP practices in the hospital`s supply chain was assessed by computational simulation modelling, focusing on one of the most financially important product families.
Main findings
Since the simulation model considers the variability of suppliers and customers as inputs, it allows the verification of the proposed inventory policies effectiveness, in order to avoid affecting the service level.
Implications for theory and practice
The proposition of a method that integrates value stream mapping into computational simulation modelling brings a differentiated approach to analyze lean implementation in a healthcare supply chain. The simulation model supports a more assertive decision-making process on lean implementation, allowing the organization to ensure that the quality and efficiency of healthcare is not affected.
Keywords:
Lean production; Lean supply chain; Lean healthcare; Simulation model
1. Introduction
Healthcare organizations are an important part of the service industry given not only the criticality of quality and safety in patient care but also due to the high associated investment (Dobrzykowski et al., 2014Dobrzykowski, D., Deilami, V., Hong, P., & Kim, S. (2014). A structured analysis of operations and supply chain management research in healthcare (1982–2011). International Journal of Production Economics, 147, 514-530. http://dx.doi.org/10.1016/j.ijpe.2013.04.055.
http://dx.doi.org/10.1016/j.ijpe.2013.04...
). Aherne & Whelton (2010)Aherne, J., & Whelton, J. (Eds.). (2010). Applying lean in healthcare: a collection of international case studies. Boca Raton: CRC Press. http://dx.doi.org/10.1201/EBK1439827390.
http://dx.doi.org/10.1201/EBK1439827390...
and Waring & Bishop (2010)Waring, J., & Bishop, S. (2010). Lean healthcare: rhetoric, ritual and resistance. Social Science & Medicine, 71(7), 1332-1340. http://dx.doi.org/10.1016/j.socscimed.2010.06.028. PMid:20702013.
http://dx.doi.org/10.1016/j.socscimed.20...
comment that these organizations are under constant pressure to reduce costs, waiting times, errors, while improving service quality and patient safety. The challenging context of healthcare organizations has been denoted in 2008 by the Institute for Healthcare Improvement (IHI) as the Triple Aim, which simultaneously looks for improving the individual experience of care, improving the health of populations, and reducing the per capita costs of care for population (Whittington et al., 2015Whittington, J. W., Nolan, K., Lewis, N., & Torres, T. (2015). Pursuing the triple aim: the first 7 years. The Milbank Quarterly, 93(2), 263-300. http://dx.doi.org/10.1111/1468-0009.12122. PMid:26044630.
http://dx.doi.org/10.1111/1468-0009.1212...
). The essence of Triple Aim can also be associated with the underlying complexity of healthcare organizations, aggravating the difficulties for an effective healthcare management (Plsek & Greenhalgh, 2001Plsek, P. E., & Greenhalgh, T. (2001). The challenge of complexity in health care: an introduction. BMJ, 323(7314), 625-628. http://dx.doi.org/10.1136/bmj.323.7313.625. PMid:11557716.
http://dx.doi.org/10.1136/bmj.323.7313.6...
; Sheikh et al., 2015Sheikh, A., Sood, H., & Bates, D. (2015). Leveraging health information technology to achieve the “triple aim” of healthcare reform. Journal of the American Medical Informatics Association, 22(4), 849-856. http://dx.doi.org/10.1093/jamia/ocv022. PMid:25882032.
http://dx.doi.org/10.1093/jamia/ocv022...
). Dooner (2014)Dooner, R. (2014). How supply chain management can help to control health-care costs. CSCMP’s Supply Chain Quarterly, 8(3), 50-53. indicated that the lack of standardized processes increases waste in healthcare organizations.
Regarding the processes of a healthcare organization, those related to material and information flows are the most expensive ones, corresponding from 30 to 40% of the total expenditures (Aronsson et al., 2011Aronsson, H., Abrahamsson, M., & Spens, K. (2011). Developing lean and agile health care supply chains. Supply Chain Management, 16(3), 176-183. http://dx.doi.org/10.1108/13598541111127164.
http://dx.doi.org/10.1108/13598541111127...
). In this sense, the management of hospital’s supply chain presents great opportunities for improvement in healthcare systems, both in terms of cost reduction and increased quality of care (Schwarting et al., 2011Schwarting, D., Bitar, J., Arya, Y., & Pfeiffer, T. (2011). The transformative hospital supply chain: balancing costs with quality. USA: Booz & Company.). Among the existing improvement approaches, the adaptation of manufacturing concepts, such as Lean Production (LP), has been widely accepted (Womack et al., 2005Womack, J., Byrne, A., Fiume, O., Kaplan, G., & Toussaint, J. (2005). Going lean in health care. Cambridge: Institute for Healthcare Improvement.; Brandão de Souza, 2009Brandão de Souza, L. (2009). Trends and approaches in lean healthcare. Leadership in Health Services, 22(2), 121-139. http://dx.doi.org/10.1108/17511870910953788.
http://dx.doi.org/10.1108/17511870910953...
). However, Hasle et al. (2016)Hasle, P., Nielsen, A., & Edwards, K. (2016). Application of lean manufacturing in hospitals: the need to consider maturity, complexity, and the value concept. Human Factors and Ergonomics in Manufacturing & Service Industries, 26(4), 430-442. http://dx.doi.org/10.1002/hfm.20668.
http://dx.doi.org/10.1002/hfm.20668...
emphasize that such adoption in healthcare, denoted as Lean Healthcare (LH), requires an adequate adjustment to the complexity inherent to health care processes in order to enable better performance. Healthcare supply chain management may be focused on the whole chain, including suppliers and distributors, or may be restricted to one or more value stream (comprising one or more sectors of the organization) (Shah et al., 2008Shah, R., Goldstein, S., Unger, B., & Henry, T. (2008). Explaining anomalous high performance in a health care supply chain. Decision Sciences, 39(4), 759-789. http://dx.doi.org/10.1111/j.1540-5915.2008.00211.x.
http://dx.doi.org/10.1111/j.1540-5915.20...
). To understand the various levels of complexity frequently associated to healthcare supply chains, one must clearly define the problem and comprehend the flows across organizational interfaces, including materials, information and patients (Böhme et al., 2013Böhme, T., Williams, S. J., Childerhouse, P., Deakins, E., & Towill, D. (2013). Methodology challenges associated with benchmarking healthcare supply chains. Production Planning and Control, 24(10-11), 1002-1014. http://dx.doi.org/10.1080/09537287.2012.666918.
http://dx.doi.org/10.1080/09537287.2012....
).
Given the importance of healthcare organizations, it is prudent to assess their impacts to ensure that the service level will not be affected when implementing lean practices in hospital’s supply chain. According to Chung (2013)Chung, C. (Ed.). (2013). Simulation modeling handbook: a practical approach. London: CRC Press., testing new concepts or systems before implementation and obtaining information without disrupting the current system are some of the purposes of modeling and simulation analysis. In addition, simulation modeling has specific benefits, which include: compressed-time experimentation, reduced analytical requirements and easily demonstrable models, prior quantification of the improvements, supporting the reduction of change resistance, cost reduction and lead time, greater customer relationship and greater understanding of the processes among its stakeholders (Haddad et al., 2016Haddad, M., Zouein, P., Salem, J., & Otayek, R. (2016). Case study of lean in hospital admissions to inspire culture change. Engineering Management Journal, 28(4), 209-223. http://dx.doi.org/10.1080/10429247.2016.1234896.
http://dx.doi.org/10.1080/10429247.2016....
). In this sense, based upon the aforementioned arguments, we raise the the following research question: “what is the impact of lean practices implementation in the healthcare supply chain?”.
To answer this question, this article aims to evaluate the impact of lean practices implementation in the healthcare supply chain context aided by computer simulation modelling. To achieve that, a case study was carried out involving a Brazilian public-university hospital, whose focus was on the value stream improvement of the product family called OPSM (Orthoses, Prostheses and Special Materials), which is relevant both in terms of cost and operational aspects. The data related to this value stream were collected identifying the main sources of uncertainty and their variability, in order to allow its subsequently computational modeling verification. Results of this analysis were evaluated based on two performance indicators: (i) delivery service level and (ii) lead time. It is also noteworthy that this research expands upon Borges et al. (2018)Borges, G., Tortorella, G., Frazzon, E., & Martinez, F. (2018, June). Simulation-based analysis of lean implementation in healthcare. In Proceedings from 25th International Annual EurOMA Conference. Brussels: European Operations Management Association. , which has only envisioned some relationships but has not properly evidenced them.
The rest of this article is structured as follows. Section 2 presents a brief literature review on healthcare supply chain, lean practices in healthcare supply chain and computational simulation modelling applied to supply chain. Section 3 describes the proposed research method, whose results are presented in Section 4. Finally, Section 5 closes the article presenting findings and future research opportunities.
2. Literature review
2.1. Healthcare supply chain
The concept of supply chain management is concerned with the management of a supply chain, which can be defined as a set of three or more entities (organizations or individuals) directly involved in the upstream and downstream flows of products, services, finances, and/or information from a source to a customer and back (Mentzer et al., 2001Mentzer, J., Dewitt, W., Keebler, J., Min, S., Nix, N., Smith, C., & Zacharia, Z. (2001). Defining supply chain management. Journal of Business Logistics, 22(2), 1-25. http://dx.doi.org/10.1002/j.2158-1592.2001.tb00001.x.
http://dx.doi.org/10.1002/j.2158-1592.20...
). According to Nelson et al. (2001)Nelson, D., Moody, P., & Stegner, J. (2001). The purchasing machine. New York; The Free Press., for supply chain management to be successful, there is a need for top leadership support and comprehension about the importance of its management, benchmarking to assess and guide processes, shared knowledge and common understanding among all members, and institutionalization of continuous improvement initiatives. Interest in the concept of supply chain management has increased since the 1980s, when the concept first emerged and companies began to understand the benefits of collaborative relationships inside and outside their own organization (Lummus & Vokurka, 1999Lummus, R., & Vokurka, R. (1999). Defining supply chain management: a historical perspective and practical guidelines. Industrial Management & Data Systems, 99(1), 11-17. http://dx.doi.org/10.1108/02635579910243851.
http://dx.doi.org/10.1108/02635579910243...
; Chen & Paulraj, 2004Chen, I., & Paulraj, A. (2004). Towards a theory of supply chain management: the constructs and measurements. Journal of Operations Management, 22(2), 119-150. http://dx.doi.org/10.1016/j.jom.2003.12.007.
http://dx.doi.org/10.1016/j.jom.2003.12....
). However, despite the fact that in recent decades the scope of supply chain management has expanded considerably, there are still limitations on its approach in healthcare value chain (McKone‐Sweet et al., 2005McKone‐Sweet, K., Hamilton, P., & Willis, S. (2005). The ailing healthcare supply chain: a prescription for change. The Journal of Supply Chain Management, 41(1), 4-17. http://dx.doi.org/10.1111/j.1745-493X.2005.tb00180.x.
http://dx.doi.org/10.1111/j.1745-493X.20...
).
Healthcare organizations are institutions where the customer (i.e. patient), when seeking the service, is a part of the whole process until its end (Aronsson et al., 2011Aronsson, H., Abrahamsson, M., & Spens, K. (2011). Developing lean and agile health care supply chains. Supply Chain Management, 16(3), 176-183. http://dx.doi.org/10.1108/13598541111127164.
http://dx.doi.org/10.1108/13598541111127...
). In this sense, the healthcare supply chain management must integrate the sequences of actions defined for the generation of products and services, considering that each procedure requires a specific combination that varies between different organizations, types of patients and healthcare professionals (Jahre et al., 2012Jahre, M., Dumoulin, L., Greenhalgh, L., Hudspeth, C., Limlim, P., & Spindler, A. (2012). Improving health in developing countries: reducing complexity of drug supply chains. Journal of Humanitarian Logistics and Supply Chain Management, 2(1), 54-84. http://dx.doi.org/10.1108/20426741211226000.
http://dx.doi.org/10.1108/20426741211226...
). There is consensus within academia that healthcare supply chains are more complex than the other sectors, are surrounded with issues and very challenging to improve (Böhme et al., 2013Böhme, T., Williams, S. J., Childerhouse, P., Deakins, E., & Towill, D. (2013). Methodology challenges associated with benchmarking healthcare supply chains. Production Planning and Control, 24(10-11), 1002-1014. http://dx.doi.org/10.1080/09537287.2012.666918.
http://dx.doi.org/10.1080/09537287.2012....
). The complexities and politically oriented elements are expected to pose challenges to direct application of supply chain management techniques and concepts (Dobrzykowski et al., 2014Dobrzykowski, D., Deilami, V., Hong, P., & Kim, S. (2014). A structured analysis of operations and supply chain management research in healthcare (1982–2011). International Journal of Production Economics, 147, 514-530. http://dx.doi.org/10.1016/j.ijpe.2013.04.055.
http://dx.doi.org/10.1016/j.ijpe.2013.04...
). For instance, healthcare organizations generally face a diverse set of stakeholders with varied and conflicting interests. This mix of standardized and contingent services leads to hospitals being ‘relatively inefficient’ due to the expense of equipping and operating such multiactivity supply chain (Habidin et al., 2014Habidin, N. F., Shazali, N. A., Ali, N., Khaidir, N. A., & Jamaludin, N. H. (2014). Exploring lean healthcare practice and supply chain innovation for Malaysian healthcare industry. International Journal of Business Excellence, 7(3), 394-410. http://dx.doi.org/10.1504/IJBEX.2014.060782.
http://dx.doi.org/10.1504/IJBEX.2014.060...
).
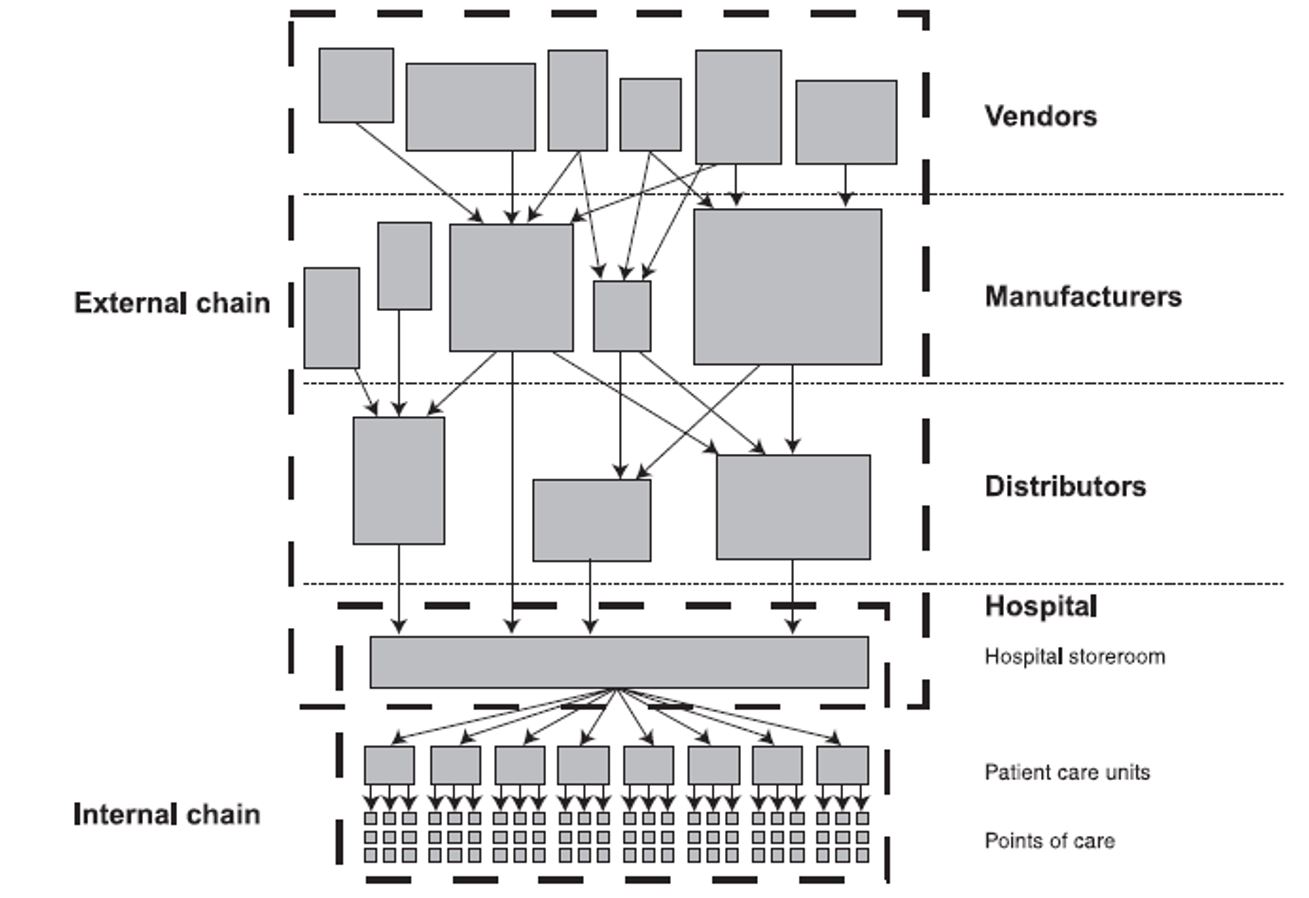
Because of such complexity, one of the main characteristics of healthcare supply chain is its division into two approaches: internal and external supply chain (see Figure 1). The external supply chain includes suppliers-related processes such as negotiation and purchase, biddings (in the case of public healthcare organizations), technical assistance and maintenance, supply logistics, etc. The internal supply chain comprises management of processes within the boundaries of the hospital that will support material, information and patients flows across hospital’s departments, units or sectors (Andersen & Co., 1990 apudRivard-Royer et al., 2002Rivard-Royer, H., Landry, S., & Beaulieu, M. (2002). Hybrid stockless: a case study. Lessons for health-care supply chain integration. International Journal of Operations & Production Management, 22(4), 412-424. http://dx.doi.org/10.1108/01443570210420412.
http://dx.doi.org/10.1108/01443570210420...
). In particular, literature shows that most of the works focus on the internal supply chain and most of these studies (e.g. Kumar et al., 2009Kumar, S., Swanson, E., & Tran, T. (2009). RFID in the healthcare supply chain: usage and application. International Journal of Health Care Quality Assurance, 22(1), 67-81. http://dx.doi.org/10.1108/09526860910927961. PMid:19284172.
http://dx.doi.org/10.1108/09526860910927...
; Jahre et al., 2012Jahre, M., Dumoulin, L., Greenhalgh, L., Hudspeth, C., Limlim, P., & Spindler, A. (2012). Improving health in developing countries: reducing complexity of drug supply chains. Journal of Humanitarian Logistics and Supply Chain Management, 2(1), 54-84. http://dx.doi.org/10.1108/20426741211226000.
http://dx.doi.org/10.1108/20426741211226...
; Teichgräber & De Bucourt, 2012Teichgräber, U., & De Bucourt, M. (2012). Applying value stream mapping techniques to eliminate non-value-added waste for the procurement of endovascular stents. European Journal of Radiology, 81(1), e47-e52. http://dx.doi.org/10.1016/j.ejrad.2010.12.045. PMid:21316173.
http://dx.doi.org/10.1016/j.ejrad.2010.1...
; Machado et al., 2013Machado, C., Carvalho, J. C., & Maia, A. (2013). Vendor managed inventory (VMI): evidences from lean deployment in healthcare. Strategic Outsourcing, 6(1), 8-24. http://dx.doi.org/10.1108/17538291311316045.
http://dx.doi.org/10.1108/17538291311316...
; Roberts et al., 2017Roberts, R., Wilson, A., & Quezado, Z. (2017). Using Lean Six Sigma methodology to improve quality of the anesthesia supply chain in a pediatric hospital. Anesthesia and Analgesia, 124(3), 922-924. http://dx.doi.org/10.1213/ANE.0000000000001621. PMid:27749347.
http://dx.doi.org/10.1213/ANE.0000000000...
) approach only a specific echelon of the internal supply chain within a department.
Hospital’s internal and external supply chains. Source: Adapted from Andersen & Co. (1990 apud Rivard-Royer et al., 2002Rivard-Royer, H., Landry, S., & Beaulieu, M. (2002). Hybrid stockless: a case study. Lessons for health-care supply chain integration. International Journal of Operations & Production Management, 22(4), 412-424. http://dx.doi.org/10.1108/01443570210420412.
http://dx.doi.org/10.1108/01443570210420... ).
2.2. Lean practices in healthcare supply chain
LH implementation promotes a new way of thinking and acting, demanding changes and participation of all members of an organization (Graban, 2016Graban, M. (2016). Lean hospitals: improving quality, patient safety, and employee engagement. New York: CRC Press. http://dx.doi.org/10.1201/b11740.
http://dx.doi.org/10.1201/b11740...
). LH implies the understanding of patient needs by specifying what is value from their perspective, removing waste and reducing processing times (Womack et al., 2005Womack, J., Byrne, A., Fiume, O., Kaplan, G., & Toussaint, J. (2005). Going lean in health care. Cambridge: Institute for Healthcare Improvement.). In addition, LH practices lead to better performance in terms of patient safety, quality, waiting time, cost, workplace environment, employees’ satisfaction and interdepartmental communication (Waring & Bishop, 2010Waring, J., & Bishop, S. (2010). Lean healthcare: rhetoric, ritual and resistance. Social Science & Medicine, 71(7), 1332-1340. http://dx.doi.org/10.1016/j.socscimed.2010.06.028. PMid:20702013.
http://dx.doi.org/10.1016/j.socscimed.20...
; Radnor et al. 2012Radnor, Z., Holweg, M., & Waring, J. (2012). Lean in healthcare: the unfilled promise? Social Science & Medicine, 74(3), 364-371. http://dx.doi.org/10.1016/j.socscimed.2011.02.011. PMid:21414703.
http://dx.doi.org/10.1016/j.socscimed.20...
).
In the context of the manufacturing industry, Tortorella et al. (2017a)Tortorella, G., Miorando, R., & Tlapa, D. (2017a). Implementation of lean supply chain: an empirical research on the effect of context. The TQM Journal, 29(4), 610-623. http://dx.doi.org/10.1108/TQM-11-2016-0102.
http://dx.doi.org/10.1108/TQM-11-2016-01...
identified 27 most commonly implemented lean practices in supply chains. However, when considering healthcare organizations, these lean practices may suffer significant adaptations (Fillingham, 2007Fillingham, D. (2007). Can lean save lives? Leadership in Health Services, 20(4), 231-241. http://dx.doi.org/10.1108/17511870710829346. PMid:20698096.
http://dx.doi.org/10.1108/17511870710829...
). Moreover, Adebanjo et al. (2016)Adebanjo, D., Laosirihongthong, T., & Samaranayake, P. (2016). Prioritizing lean supply chain management initiatives in healthcare service operations: a fuzzy AHP approach. Production Planning and Control, 27(12), 953-966. http://dx.doi.org/10.1080/09537287.2016.1164909.
http://dx.doi.org/10.1080/09537287.2016....
indicated that the number of lean practices implemented in the healthcare supply chain is likely to be much lower. In fact, they suggest that the lack of homogeneity related to the implementation of lean practices in healthcare supply chain deserves a careful consideration by healthcare organizations. Among the lean practices most frequently adopted in healthcare organizations are value stream analysis or value stream mapping (Kimsey, 2010Kimsey, D. (2010). Lean methodology in health care. AORN Journal, 92(1), 53-60. http://dx.doi.org/10.1016/j.aorn.2010.01.015. PMid:20619772.
http://dx.doi.org/10.1016/j.aorn.2010.01...
; Setijono et al., 2010Setijono, D., Mohajeri Naraghi, A., & Pavan Ravipati, U. (2010). Decision support system and the adoption of lean in a swedish emergency ward: balancing supply and demand towards improved value stream. International Journal of Lean Six Sigma, 1(3), 234-248. http://dx.doi.org/10.1108/20401461011075026.
http://dx.doi.org/10.1108/20401461011075...
; Chiarini, 2013Chiarini, A. (2013). Waste savings in patient transportation inside large hospitals using lean thinking tools and logistic solutions. Leadership in Health Services, 26(4), 356-367. http://dx.doi.org/10.1108/LHS-05-2012-0013.
http://dx.doi.org/10.1108/LHS-05-2012-00...
; Farrokhi et al., 2013Farrokhi, F. R., Gunther, M., Williams, B., & Blackmore, C. C. (2013). Application of lean methodology for improved quality and efficiency in operating room instrument availability. Journal for Healthcare Quality, 37(5), 277-286 PMid:; Narayanamurthy & Gurumurthy, 2018Narayanamurthy, G., & Gurumurthy, A. (2018). Is the hospital lean? A mathematical model for assessing the implementation of lean thinking in healthcare institutions. Operations Research for Health Care, 18, 84-98. http://dx.doi.org/10.1016/j.orhc.2017.05.002.
http://dx.doi.org/10.1016/j.orhc.2017.05...
) and standardized work procedures (Shah et al., 2008Shah, R., Goldstein, S., Unger, B., & Henry, T. (2008). Explaining anomalous high performance in a health care supply chain. Decision Sciences, 39(4), 759-789. http://dx.doi.org/10.1111/j.1540-5915.2008.00211.x.
http://dx.doi.org/10.1111/j.1540-5915.20...
; Hasle et al., 2016Hasle, P., Nielsen, A., & Edwards, K. (2016). Application of lean manufacturing in hospitals: the need to consider maturity, complexity, and the value concept. Human Factors and Ergonomics in Manufacturing & Service Industries, 26(4), 430-442. http://dx.doi.org/10.1002/hfm.20668.
http://dx.doi.org/10.1002/hfm.20668...
; Costa et al., 2017Costa, L. B. M., Godinho Filho, M., Rentes, A. F., Bertani, T. M., & Mardegan, R. (2017). Lean healthcare in developing countries: evidence from Brazilian hospitals. The International Journal of Health Planning and Management, 32(1), e99-e120. http://dx.doi.org/10.1002/hpm.2331. PMid:26681656.
http://dx.doi.org/10.1002/hpm.2331...
), since they are usually considered forerunners to other practices. Furthermore, kanban is another practice often implemented, as evidenced by Kumar et al. (2008)Kumar, A., Ozdamar, L., & Ning Zhang, C. (2008). Supply chain redesign in the healthcare industry of Singapore. Supply Chain Management, 13(2), 95-103. http://dx.doi.org/10.1108/13598540810860930.
http://dx.doi.org/10.1108/13598540810860...
, Bendavid et al. (2010)Bendavid, Y., Boeck, H., & Philippe, R. (2010). Redesigning the replenishment process of medical supplies in hospitals with RFID. Business Process Management Journal, 16(6), 991-1013. http://dx.doi.org/10.1108/14637151011093035.
http://dx.doi.org/10.1108/14637151011093...
, Kates (2014)Kates, S. (2014). Lean business model and implementation of a geriatric fracture center. Clinics in Geriatric Medicine, 30(2), 191-205. http://dx.doi.org/10.1016/j.cger.2014.01.002. PMid:24721360.
http://dx.doi.org/10.1016/j.cger.2014.01...
, Papalexi et al. (2016)Papalexi, M., Bamford, D., & Dehe, B. (2016). A case study of kanban implementation within the pharmaceutical supply chain. International Journal of Logistics Research and Applications, 19(4), 239-255. http://dx.doi.org/10.1080/13675567.2015.1075478.
http://dx.doi.org/10.1080/13675567.2015....
. In turn, practices, such as visual management (Jin et al., 2008Jin, M., Switzer, M., & Agirbas, G. (2008). Six Sigma and Lean in healthcare logistics centre design and operation: a case at North Mississippi Health Services. International Journal of Six Sigma and Competitive Advantage, 4(3), 270-288. http://dx.doi.org/10.1504/IJSSCA.2008.021840.
http://dx.doi.org/10.1504/IJSSCA.2008.02...
; Liu et al., 2016Liu, T., Shen, A., Hu, X., Tong, G., Gu, W., & Yang, S. (2016). SPD-based logistics management model of medical consumables in hospitals. Iranian Journal of Public Health, 45(10), 1288-1299. PMid:27957435.), inventory policies (Jahre et al., 2012Jahre, M., Dumoulin, L., Greenhalgh, L., Hudspeth, C., Limlim, P., & Spindler, A. (2012). Improving health in developing countries: reducing complexity of drug supply chains. Journal of Humanitarian Logistics and Supply Chain Management, 2(1), 54-84. http://dx.doi.org/10.1108/20426741211226000.
http://dx.doi.org/10.1108/20426741211226...
; Liu et al., 2015Liu, M., Zhang, L., & Zhang, Z. (2015). Optimal scheduling of logistical support for medical resources order and shipment in community health service centers. Journal of Industrial Engineering and Management, 8(5), 1362. http://dx.doi.org/10.3926/jiem.1463.
http://dx.doi.org/10.3926/jiem.1463...
; Lim et al., 2017Lim, J., Norman, B., & Rajgopal, J. (2017). Process redesign and simplified policies for more effective vaccine inventory management. Engineering Management Journal, 29(1), 17-25. http://dx.doi.org/10.1080/10429247.2016.1277446.
http://dx.doi.org/10.1080/10429247.2016....
), consignment stock, are much less frequently reported in the literature. More research is therefore required to more holistically understand the implementation of lean practices in healthcare supply chains (Bhasin, 2011Bhasin, S. (2011). Performance of organizations treating lean as an ideology. Business Process Management Journal, 17(6), 986-1011. http://dx.doi.org/10.1108/14637151111182729.
http://dx.doi.org/10.1108/14637151111182...
).
One reason for such theoretical gap can be associated with the differences in lean maturity and complexity levels between manufacturing and healthcare contexts (Shah et al., 2008Shah, R., Goldstein, S., Unger, B., & Henry, T. (2008). Explaining anomalous high performance in a health care supply chain. Decision Sciences, 39(4), 759-789. http://dx.doi.org/10.1111/j.1540-5915.2008.00211.x.
http://dx.doi.org/10.1111/j.1540-5915.20...
). Wijewardana & Rupasinghe (2013)Wijewardana, R., & Rupasinghe, T. (2013). Applicability of Lean Healthcare in Sri Lankan Healthcare Supply Chains. International Journal of Supply Chain Management, 2(4), 42-49. add that, although it has been proven that lean can be adopted in healthcare, it remains a challenge to practically implement with the rigid healthcare supply chain structure. Khorasani et al. (2015)Khorasani, S., Maghazei, O., & Cross, J. (2015). A structured review of lean supply chain management in health care. In Proceedings of the International Annual Conference of the American Society for Engineering Management (p. 1). Huntsville: ASEM. argued that the lack of supply chain education within healthcare organizations is a critical barrier for lean implementation. Healthcare organizations are usually organized in functional silos and need well-established processes to meet patient demands on availability of services, short lead-times, high efficiency and quality of care (D’Andreamatteo et al., 2015D’Andreamatteo, A., Ianni, L., Lega, F., & Sargiacomo, M. (2015). Lean in healthcare: a comprehensive review. Health Policy, 119(9), 1197-1209. http://dx.doi.org/10.1016/j.healthpol.2015.02.002. PMid:25737260.
http://dx.doi.org/10.1016/j.healthpol.20...
). Patient process frequently involves a large number of functions in need of coordination both in space and time, which undermines an effective design of the supply chain (Aronsson et al., 2011Aronsson, H., Abrahamsson, M., & Spens, K. (2011). Developing lean and agile health care supply chains. Supply Chain Management, 16(3), 176-183. http://dx.doi.org/10.1108/13598541111127164.
http://dx.doi.org/10.1108/13598541111127...
). To guide lean implementation in healthcare supply chain, Machado et al. (2014)Machado, C., Scavarda, A., & Vaccaro, G. (2014). Lean healthcare supply chain management: minimizing waste and costs. Independent Journal of Management & Production, 5(4), 1071-1088. http://dx.doi.org/10.14807/ijmp.v5i4.245.
http://dx.doi.org/10.14807/ijmp.v5i4.245...
proposed a conceptual model to assist hospitals to identify what is important in view of the customer (patient) through changing organizational culture, being the main vehicle teamwork (doctors, nurses).
2.3. Computational simulation modelling applied to supply chain
Simulation-based techniques can be used to develop or evaluate complex systems (Frazzon et al., 2017Frazzon, E., Tortorella, G., Dávalos, R., Holtz, T., & Coelho, L. (2017). Simulation-based analysis of a supplier-manufacturer relationship in lean supply chains. International Journal of Lean Six Sigma, 8(3), 262-274. http://dx.doi.org/10.1108/IJLSS-03-2016-0009.
http://dx.doi.org/10.1108/IJLSS-03-2016-...
) allowing for a better understanding of processes and supporting managers in the decision-making process (Sakurada & Miyake, 2009Sakurada, N., & Miyake, D. (2009). Aplicação de simuladores de eventos discretos no processo de modelagem de sistemas de operações de serviços. Gestão & Produção, 16(1), 25-43. http://dx.doi.org/10.1590/S0104-530X2009000100004.
http://dx.doi.org/10.1590/S0104-530X2009...
). Simulation models can be used as tools to analyze a system’s response under different scenarios without necessarily disturbing it (Sharma et al., 2007Sharma, V., Abel, J., Al‐Hussein, M., Lennerts, K., & Pfründer, U. (2007). Simulation application for resource allocation in facility management processes in hospitals. Facilities, 25(13/14), 493-506. http://dx.doi.org/10.1108/02632770710822599.
http://dx.doi.org/10.1108/02632770710822...
; Setijono et al., 2010Setijono, D., Mohajeri Naraghi, A., & Pavan Ravipati, U. (2010). Decision support system and the adoption of lean in a swedish emergency ward: balancing supply and demand towards improved value stream. International Journal of Lean Six Sigma, 1(3), 234-248. http://dx.doi.org/10.1108/20401461011075026.
http://dx.doi.org/10.1108/20401461011075...
). In general, the use of simulation modelling for supply chain analysis has some advantages, such as: possibility of dealing with high-variability situations; usually lower investments compared to changes implemented directly on real systems; possibility of controlling the conditions under which the simulations are performed; and visualizing the supply chain behavior. In turn, some disadvantages are also noteworthy, such as: requirement of a significant amount of data; large experience and knowledge about the utilized software; considerable time demand to properly represent the aimed model (Ingallis, 1998Ingallis, R. (1998). The value of simulation in modeling supply chains. In Winter Simulation Conference Proceedings (Vol. 2, pp. 1371-1375). New York: Association for Computing Machinery. http://dx.doi.org/10.1109/WSC.1998.746004.
http://dx.doi.org/10.1109/WSC.1998.74600...
; Robinson, 2004Robinson, S. (2004). Simulation: the practice of model development and use. Chichester: Wiley.).
To select the type of simulation approach to be used, the characteristics of the variables and the nature of the system to be modeled and simulated should be considered. According to Oliveira et al. (2016)Oliveira, J., Lima, R., & Montevechi, J. (2016). Perspectives and relationships in Supply Chain Simulation: A systematic literature review. Simulation Modelling Practice and Theory, 62, 166-191. http://dx.doi.org/10.1016/j.simpat.2016.02.001.
http://dx.doi.org/10.1016/j.simpat.2016....
, the four types of simulation approaches more frequently applied to supply chain problems are the events-based (mainly discrete events), agent-based, continuous simulations and dynamic simulations. Archibald et al. (1999)Archibald, G., Karabakal, N., & Karlsson, P. (1999). Supply chain vs. supply chain: using simulation to compete beyond the four walls. In Proceedings of the 31st Conference on Winter Simulation: a Bridge to the Future (Vol. 2, pp. 1207-1214). New York: ACM. http://dx.doi.org/10.1145/324898.325039.
http://dx.doi.org/10.1145/324898.325039...
, for instance, described the computational simulation of a food sector supply chain to verify the effectiveness of alternative logistic management strategies, especially the adoption of continuous replacement policies. Persson & Olhager (2002)Persson, F., & Olhager, J. (2002). Performance simulation of supply chain designs. International Journal of Production Economics, 77(3), 231-245. http://dx.doi.org/10.1016/S0925-5273(00)00088-8.
http://dx.doi.org/10.1016/S0925-5273(00)...
evaluated different supply chains for a mobile communication industry according to performance indicators such as quality, lead time and costs. Meanwhile, Frazzon et al. (2017)Frazzon, E., Tortorella, G., Dávalos, R., Holtz, T., & Coelho, L. (2017). Simulation-based analysis of a supplier-manufacturer relationship in lean supply chains. International Journal of Lean Six Sigma, 8(3), 262-274. http://dx.doi.org/10.1108/IJLSS-03-2016-0009.
http://dx.doi.org/10.1108/IJLSS-03-2016-...
tested two different configurations for the integration between transport and material flows in terms of delivery service level and lead time performances.
In healthcare context, some studies using computational simulation are also found, although the evidence is much scarcer. However, Young et al. (2004)Young, T., Brailsford, S., Connell, C., Davies, R., Harper, P., & Klein, J. (2004). Using industrial processes to improve patient care. BMJ, 328(7432), 162-164. http://dx.doi.org/10.1136/bmj.328.7432.162. PMid:14726351.
http://dx.doi.org/10.1136/bmj.328.7432.1...
argued that simulation modeling is an important technique to identify the benefits of implementing new approaches in healthcare supply chain contexts. Kumar et al. (2008)Kumar, A., Ozdamar, L., & Ning Zhang, C. (2008). Supply chain redesign in the healthcare industry of Singapore. Supply Chain Management, 13(2), 95-103. http://dx.doi.org/10.1108/13598540810860930.
http://dx.doi.org/10.1108/13598540810860...
, for instance, used a simulation model to evaluate the unification of a sterilization service center to supply three hospitals in Singapore. Savino et al. (2015)Savino, M., Mazza, A., & Marchetti, B. (2015). Lean manufacturing within critical healthcare supply chain: an exploratory study through value chain simulation. International Journal of Procurement Management, 8(1-2), 3-24. http://dx.doi.org/10.1504/IJPM.2015.066285.
http://dx.doi.org/10.1504/IJPM.2015.0662...
applied simulation to assess the impacts of lean implementation in supply chain, focusing on more efficient energy consumptions in healthcare. Finally, Kane et al. (2007)Kane, R., Shamliyan, T., Mueller, C., Duval, S., & Wilt, T. (2007). The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Medical Care, 45(12), 1195-1204. http://dx.doi.org/10.1097/MLR.0b013e3181468ca3. PMid:18007170.
http://dx.doi.org/10.1097/MLR.0b013e3181...
emphasized that demand amplification can be considered as one of the main causes of healthcare supply chain stress, reducing access to services and, hence, service quality degradation.
3. Method
The proposed method consists of eight main steps, as follows: (i) selection of the healthcare organization and its supply chain; (ii) current state mapping; (iii) future state design; (iv) quantitative data collection; (v) supply chain inventory policies proposition; (vi) definition of supply chain performance parameters; (vii) theoretical/conceptual model construction; and (viii) verification and validation of the proposed policies. These steps are described in detail below.
Step (i) consists of selecting an appropriate healthcare organization and its supply chain value stream to conduct the study. Some criteria were determined for an appropriate selection. First, the healthcare organization should present a clear initiative regarding lean practices implementation (Terra & Berssaneti, 2018Terra, J., & Berssaneti, F. (2018). Application of lean healthcare in hospital services: a review of the literature (2007 to 2017). Production, 28, e20180009. http://dx.doi.org/10.1590/0103-6513.20180009.
http://dx.doi.org/10.1590/0103-6513.2018...
), which would provide a greater legitimacy of the involved team and allow more assertive results for the computational simulation model. Second, senior management from this organization should support and commit to share the information needed to develop the study (Dickson et al., 2009Dickson, E., Anguelov, Z., Vetterick, D., Eller, A., & Singh, S. (2009). Use of lean in the emergency department: a case series of 4 hospitals. Annals of Emergency Medicine, 54(4), 504-510. http://dx.doi.org/10.1016/j.annemergmed.2009.03.024. PMid:19423187.
http://dx.doi.org/10.1016/j.annemergmed....
; Teichgräber & De Bucourt, 2012Teichgräber, U., & De Bucourt, M. (2012). Applying value stream mapping techniques to eliminate non-value-added waste for the procurement of endovascular stents. European Journal of Radiology, 81(1), e47-e52. http://dx.doi.org/10.1016/j.ejrad.2010.12.045. PMid:21316173.
http://dx.doi.org/10.1016/j.ejrad.2010.1...
). More specifically, regarding the selected supply chain, it should have significant relevance to the performance of the healthcare organization. Such relevance may be of different nature, such as financial or service quality (Regis et al., 2018Regis, T., Gohr, C., & Santos, L. (2018). Lean healthcare implementation: experiences and lessons learned from Brazilian hospitals. Revista de Administração de Empresas, 58(1), 30-43.). In addition, the supply chain value stream was expected to involve a significant number of departments within the healthcare organization, allowing a horizontal assessment of lean implementation from a more holistic perspective. Finally, it is suggested that the selected supply chain presented improvement opportunities that are under organization's leadership responsibility. Such criterion enables increasing the likelihood of actually adopting the indications from this study; i.e. we mainly aimed for a hospital’s internal supply chain (Rivard-Royer et al., 2002Rivard-Royer, H., Landry, S., & Beaulieu, M. (2002). Hybrid stockless: a case study. Lessons for health-care supply chain integration. International Journal of Operations & Production Management, 22(4), 412-424. http://dx.doi.org/10.1108/01443570210420412.
http://dx.doi.org/10.1108/01443570210420...
).
In Step (ii), the current state of the selected supply chain was mapped in order to analyze processes, flows and identify wastes, determining the steps that added value to the service (Hines & Rich, 1997Hines, P., & Rich, N. (1997). The seven value stream mapping tools. International Journal of Operations & Production Management, 17(1), 46-64. http://dx.doi.org/10.1108/01443579710157989.
http://dx.doi.org/10.1108/01443579710157...
). In this step, it is recommended to involve a cross-functional team including employees with in-depth knowledge of processes and experienced leaders in lean implementation (Tortorella et al., 2017bTortorella, G., Fogliatto, F., Anzanello, M., Marodin, G., Garcia, M., & Reis Esteves, R. (2017b). Making the value flow: application of value stream mapping in a Brazilian public healthcare organization. Total Quality Management & Business Excellence, 28(13-14), 1544-1558. http://dx.doi.org/10.1080/14783363.2016.1150778.
http://dx.doi.org/10.1080/14783363.2016....
). Three approaches were simultaneously applied to collect information and draw the current state map: (i) guided on-site visits; (ii) observation; and (iii) focused groups with the cross-functional team. Through these approaches, process information, such as cycle times, lead times, number of workers, information flow, etc., was deterministically collected (assuming no variation occurrence). The current state map analysis allowed a better understanding about the value stream from customer's perspective and, hence, identifying wastes that would be addressed in the future state map as improvement opportunities (Tortorella et al., 2018Tortorella, G., Silva, G., Campos, L. M., Pizzeta, C., Latosinski, A., & Soares, A. (2018). Productivity improvement in solid waste recycling centres through lean implementation aided by multi-criteria decision analysis. Benchmarking, 25(5), 1480-1499. http://dx.doi.org/10.1108/BIJ-01-2017-0013.
http://dx.doi.org/10.1108/BIJ-01-2017-00...
).
To clearly define the improvement opportunities, Step (iii) consists in designing a desired (future) state for the supply chain value stream. This future state value stream should be focused on increasing system flexibility, minimizing inventories, standardizing processes and inventory policies, improving material and information flows efficiency and eliminating waste (Rother & Shook, 2003Rother, M., & Shook, J. (2003). Learning to see: value stream mapping to add value and eliminate muda. Cambridge: Lean Enterprise Institute.; Duggan, 2012Duggan, K. (2012). Creating mixed model value streams: practical lean techniques for building to demand. New York: Productivity Press.). Semi-structured interviews (see script in Appendix A
Appendix A
Semi-structured interviews script.
1. Which improvement initiatives does the organization already have?
2. Give examples of lean practices successfully implemented and the impacts they have caused.
3. Give examples of lean practices implemented that have not had the expected result.
4. What are the tasks performed in the sector?
5. Which activities do you believe take more time in your job?
6. In your opinion, what are the great improvement opportunities in the process?
) were additionally conducted with experienced hospital’s leaders from supplies and materials sector. Recording of interviews was done through annotations, which were later compiled for analysis. In addition, four researchers (one PhD candidate and three master students) with lean practices experience carried-out these interviews in order to allow a greater research covalidity and avoid information collection tendency, enabling the verification of data convergences/divergences (Eisenhardt, 1989Eisenhardt, K. (1989). Building theories from case study research. Academy of Management Review, 14(4), 532-550. http://dx.doi.org/10.5465/amr.1989.4308385.
http://dx.doi.org/10.5465/amr.1989.43083...
). Finally, the future state design of the supply chain value stream was consolidated with the same cross-functional team that mapped Step (ii), so that the ideas and improvement targets were shared among team members increasing their engagement and commitment in its implementation.
Step (iv) consists of collecting further quantitative data of the supply chain, so that variability of uncertainty sources was captured. According to Simangunsong et al. (2011)Simangunsong, E., Hendry, L. C., & Stevenson, M. (2011). Supply chain uncertainty: a review and theoretical foundation for future research. International Journal of Production Research, 50(16), 4493-4523. http://dx.doi.org/10.1080/00207543.2011.613864.
http://dx.doi.org/10.1080/00207543.2011....
, supply chain uncertainties can be classified into three groups: (a) organization’s internal uncertainties, related to the internal processes and behavioral characteristics of the organization, (b) supply chain’s internal uncertainties, related to aspects of customer demand, supplier delivery time, etc., and (c) external uncertainties, which are out of the supply chain members’ control, such as economic regulations, government policies, macroeconomic issues and disasters. In this sense, the quantitative data to be collected in this step referred to the organization and supply chain’s internal uncertainties, such as: processes lead time, changes in customer demand and variation at suppliers’ delivery time. Thus, we gathered data from two sources: historical data available in hospital’s system and data recorded in a spreadsheet especially established for this study.
In step (v) we determined the inventory policies for each product contemplated in the selected supply chain. Based upon hospital’s current inventory control methodology, inventory policies followed the continuous inventory review management approach. In this sense, three parameters were determined: cyclic stock, safety stock and reorder point. Since product families are managed in consignation with suppliers, the contractually agreed replenishment time was used as input parameter for the cyclic inventory calculation. In addition, this parameter was considered deterministic, since evidence showed that suppliers present a minimum variability in replenishment lead time. Thus, cyclic stock sc was determined by the following Equation 1:
where: L = number of days for product replacement contractually agreed with suppliers; and d = average daily units of product demand.
Furthermore, the ABC classification of the products was performed according to products annual demand. Then, the desired service levels for each type of product (A, B or C) were determined. For this, the same leaders previously interviewed in Step (iii) were consulted to establish the desired service level based on medical criticality of their eventual scarcity. The data collected in Step (iv) also allowed the identification of demand variability (standard deviation) of each product during replacement lead time. Thus, Equation 2 was used to determine the safety stock component ss (Krajewski et al., 2016Krajewski, L., Malhotra, M., & Ritzman, L. (2016). Operations management: processes and supply chains (10th ed.). Upper Saddle River: Pearson.):
where: z = tabulated value related to the desired service level.
Finally, the reorder point (R) of each product was initially determined by:
After inventory policies calculation, meetings with the same leaders were undertaken in order to present the numerical results and verify their agreement. Thus, based on their operational experience, such leaders have qualitatively adjusted the sc, ss and R of each product. The qualitative adjustment of quantitative parameters is a common practice in studies that involve products planning and control (e.g. Fogliatto et al., 2018Fogliatto, F., Anzanello, M., Tortorella, G., Schneider, D., Pereira, C., & Schaan, B. (2018). A Six Sigma approach to analyze time-to-assembly variance of surgical trays in a sterile services department. Journal for Healthcare Quality, 40(3), e46-e53. http://dx.doi.org/10.1097/JHQ.0000000000000078. PMid:28346244.
http://dx.doi.org/10.1097/JHQ.0000000000...
; Meneghini et al., 2018Meneghini, M., Anzanello, M., Kahmann, A., & Tortorella, G. (2018). Quantitative demand forecasting adjustment based on qualitative factors: case study at a fast food restaurant. Sistemas & Gestão, 13(1), 68-80. http://dx.doi.org/10.20985/1980-5160.2018.v13n1.1188.
http://dx.doi.org/10.20985/1980-5160.201...
).
The supply chain performance parameters were defined in Step (vi). Such performance parameters would allow to verify the effect of the employed strategy or technique (Gunasekaran et al., 2004Gunasekaran, A., Patel, C., & McGaughey, R. (2004). A framework for supply chain performance measurement. International Journal of Production Economics, 87(3), 333-347. http://dx.doi.org/10.1016/j.ijpe.2003.08.003.
http://dx.doi.org/10.1016/j.ijpe.2003.08...
). Considering the essentiality of services provided in healthcare organizations, one of the most important parameters to be evaluated is the delivery service level. Delivery service level refers to the proportion of the demand met on-time and in-full (Ganeshan et al., 2001Ganeshan, R., Boone, T., & Stenger, A. (2001). The impact of inventory and flow planning parameters on supply chain performance: an exploratory study. International Journal of Production Economics, 71(1-3), 111-118. http://dx.doi.org/10.1016/S0925-5273(00)00109-2.
http://dx.doi.org/10.1016/S0925-5273(00)...
), hence, no material shortages should be expected in hospitals (i.e. delivery service level of 100%). Another relevant performance parameter is lead time. In order to mitigate the demand and supplier delivery time variability effects, it is common to oversize inventory policies, leading to longer lead times and increased costs (Mapes et al., 2000Mapes, J., Szwejczewski, M., & New, C. (2000). Process variability and its effect on plant performance. International Journal of Operations & Production Management, 20(7), 792-808. http://dx.doi.org/10.1108/01443570010330775.
http://dx.doi.org/10.1108/01443570010330...
). In this sense, since healthcare organizations are under constant pressure to reduce costs (Waring & Bishop, 2010Waring, J., & Bishop, S. (2010). Lean healthcare: rhetoric, ritual and resistance. Social Science & Medicine, 71(7), 1332-1340. http://dx.doi.org/10.1016/j.socscimed.2010.06.028. PMid:20702013.
http://dx.doi.org/10.1016/j.socscimed.20...
), lead time reductions contribute to such goal.
In Step (vii) the theoretical/conceptual model is constructed. At this step the initial simulation sketch with the structure of the model, the logic and the constraints were described. Commonly, it starts with a simpler model, increasing progressively the complexity until it meets the problem’s requirements. At this point, it is defined which variables should be included in the model and the causal relationships between them. The involvement of stakeholders is important at this step to ensure the representativeness of the model. It is worth mentioning that some level of abstraction is necessary so that the model is analyzed with proper resolution methods (Banks, 2009Banks, C. (2009). What is modeling and simulation. In J. Sokolowski & C. Banks (Eds.), Principles of modeling and simulation. Hoboken: Wiley.; Frazzon et al., 2017Frazzon, E., Tortorella, G., Dávalos, R., Holtz, T., & Coelho, L. (2017). Simulation-based analysis of a supplier-manufacturer relationship in lean supply chains. International Journal of Lean Six Sigma, 8(3), 262-274. http://dx.doi.org/10.1108/IJLSS-03-2016-0009.
http://dx.doi.org/10.1108/IJLSS-03-2016-...
).
In this sense, we opted for the simplification and division of products according to the ABC classification based on annual demand volume. This classification is mainly indicated for practical situations where the number of items is too large to implement a specific inventory control system for each one of them (Ernst & Cohen, 1990Ernst, R., & Cohen, M. (1990). Operations related groups (ORGs): a clustering procedure for production/inventory systems. Journal of Operations Management, 9(4), 574-598. http://dx.doi.org/10.1016/0272-6963(90)90010-B.
http://dx.doi.org/10.1016/0272-6963(90)9...
). The theoretical/conceptual model represented the relationships among all variables following the approach of continuous revision for inventory control. Therefore, the structure was based on Ivanov’s (2016)Ivanov, D. (2016). Operations and supply chain simulation with AnyLogic 7.2 (2nd ed.). Berlin: School of Economics and Law. suggestion for continuous revision inventory control. For each type of product (A, B or C), an initial stock amount would be available. Products consumption would follow the demand profiles determined in Step (v). Whenever the stock level reached the reorder point, a replenishment order was generated for suppliers, which had a lead time to deliver. Hence, stock was replenished, and a new order would be generated once the reorder point was once again reached. We assumed that no restriction in suppliers’ delivery capacity. According to Olhager & Persson (2006)Olhager, J., & Persson, F. (2006). Simulating production and inventory control systems: a learning approach to operational excellence. Production Planning and Control, 17(2), 113-127. http://dx.doi.org/10.1080/09537280500223921.
http://dx.doi.org/10.1080/09537280500223...
, a fixed replenishment quantity favors process stability. Finally, such relationships were verified and agreed with hospital’s leaders, ensuring the representativeness of the model.
Finally, Step (viii) verifies and validates the proposed inventory policies. This step simulates the inventory policies proposed for each type of product, verifying if the delivery service level and lead time met the organizational needs and expectations. Thus, through computational simulation using Anylogic® software, the proposed model was analyzed for a one-year period for each of the three types of products (A, B or C). According to Frazzon et al. (2017)Frazzon, E., Tortorella, G., Dávalos, R., Holtz, T., & Coelho, L. (2017). Simulation-based analysis of a supplier-manufacturer relationship in lean supply chains. International Journal of Lean Six Sigma, 8(3), 262-274. http://dx.doi.org/10.1108/IJLSS-03-2016-0009.
http://dx.doi.org/10.1108/IJLSS-03-2016-...
, the creation of scenarios can provide relevant information about the system’s behavior in different situations. The model was replicated one hundred times considering fixed reorder point and replenishment quantity as defined in Step (v). Simulation results were then presented to hospital’s leaders in order to enable their critical analyzes and to collect feedback on such results.
4. Results
The proposed method was applied in a fifty-year-old public university-hospital located in the South of Brazil, which has 180 beds and 5,000 employees, and treats 3,900 patients per month approximately. Top management of this organization supports the continuous improvement of its processes, meeting the criteria established in Step (i) of the proposed method. In addition, the organization presents some lean implementation initiatives such as 5S, standardized work procedures and visual management. Nevertheless, the hospital has no lean certification. It is also worth mentioning that the hospital is part of the Brazilian Unified Health System (SUS), which promotes public health usually addressed to lower-income population (Dias et al., 2012Dias, M., Martins, M., & Navarro, N. (2012). Adverse outcome screening in hospitalizations of the Brazilian Unified Health System. Revista de Saude Publica, 46(4), 719-729. http://dx.doi.org/10.1590/S0034-89102012005000054. PMid:22832808.
http://dx.doi.org/10.1590/S0034-89102012...
). Due to decreasing government support, hospitals under SUS generally face a poor infrastructure and scarcity of qualified staff (Silva, 2011Silva, S. (2011). The organization of regional and integrated healthcare delivery systems: challenges facing Brazil’s Unified Health System. Ciência & Saúde Coletiva, 16(6), 2753-2764. PMid:21709973.), which aggravates our research scenario.
In order to select the supply chain to be studied, senior managers indicated that consigned products, denoted as OPSM (orthoses, prostheses and special materials), would be the priority mainly due to their financial relevance (approximately 21% of hospital's total expenses). Further, this supply chain involved a significant number of departments (approximately 10 hospital units), denoting its horizontal representativeness. Then, a cross-functional group was put together. The group consisted of 16 hospital members, from 12 different areas and with an average of 15 years of experience in the organization (see Appendix B Appendix B Hospital’s team members characteristics. Table 1B. Hospital’s team members. Hospital member Department or Unit Hospital experience time (years) 1 Material Planning 3.5 2 Purchase 2.5 3 Supply coordination 37 4 Administrative management 37 5 Consigned materials 1.5 6 Consigned materials 1.5 7 Consigned materials 2.5 8 Warehouse Not informed 9 Bidding 34 10 Financial 32 11 Financial 6 12 Healthcare management 32 13 Hospital Infection Control Committee 25 14 Hospital Infection Control Committee 13 15 Sterilization 9 16 Surgery Center 4 ), and six people with knowledge in lean implementation (one professor and five graduate students). To draw the current state map, two meetings of approximately three hours each involving the cross-functional team were carried out with on-site visits, data collection and discussions about the processes. Data collected for the value stream mapping was based on samples available at the time of the mapping activity and, consequently, did not reflect the variability in this supply chain. Figure 2 shows the current state map for OPSM family.
OPSM family had about 300 different items, although only 210 items were consumed in 2017, with a total annual demand of 2,623 units. Suppliers delivery time was contractually established for five days, and they had the obligation to exchange the consigned items that were out of date without additional charges to the hospital. Therefore, such contextual factors led to an inadequate management of products, with great potential for improvement opportunities. There was no systematic replenishment policy for this product family, and this task was solely based on employees’ experience. Moreover, there was no systematic way to manage inventory. These consigned products were supplied to several units of the hospital, with the greatest demands being those of hemodynamics and the surgical centers. The current information flow was not standardized. Requests were made by each of the hospital’s units in different ways, such as e-mail, physical request or telephone calls. Once received the orders, items were separated to await pick-up by the requesting unit. The unit that has collected the items, after using them, should present the medical report to certify the utilization and ensure traceability of the material. Throughout the value stream three scheduling points were identified: one in the request, one in the receiving/conference and another in the material pick-up. The lead time observed was 211 days and the total processing time was approximately 30 minutes.
After mapping the current state map, improvement opportunities have emerged and future state map could be designed (see Figure 3). For that, two meetings of approximately three hours were held with the cross-functional team. In addition, semi-structured interviews were carried out with hospital’s leaders, which allowed to consolidate the lean implementation opportunities. Table 1 presents the main comments of the interviewees which helped to consolidate three great opportunities. The first great opportunity concerned the standardization of materials requisition, which is fundamentally linked to the information flow. This opportunity was evidenced by the fact that the organization worked with different ways of requisition (e-mail, telephone, paper form), entailing confusion and an unassertive communication. The second opportunity was related to visual management of inventories. Such opportunity was identified from the problems related to materials conference and collection, which took a long time and were not effective. Finally, more closely related to the material flow, the need for implementing a pull system was identified. This opportunity contemplated the establishment of inventory policies, with the elaboration of a systematic to define reordering points, minimum and maximum stocks and quantities to be replenished. Since pull system implementation has a more prominent effect on supply chain lead time (Duggan, 2012Duggan, K. (2012). Creating mixed model value streams: practical lean techniques for building to demand. New York: Productivity Press.), we prioritized this improvement opportunity.
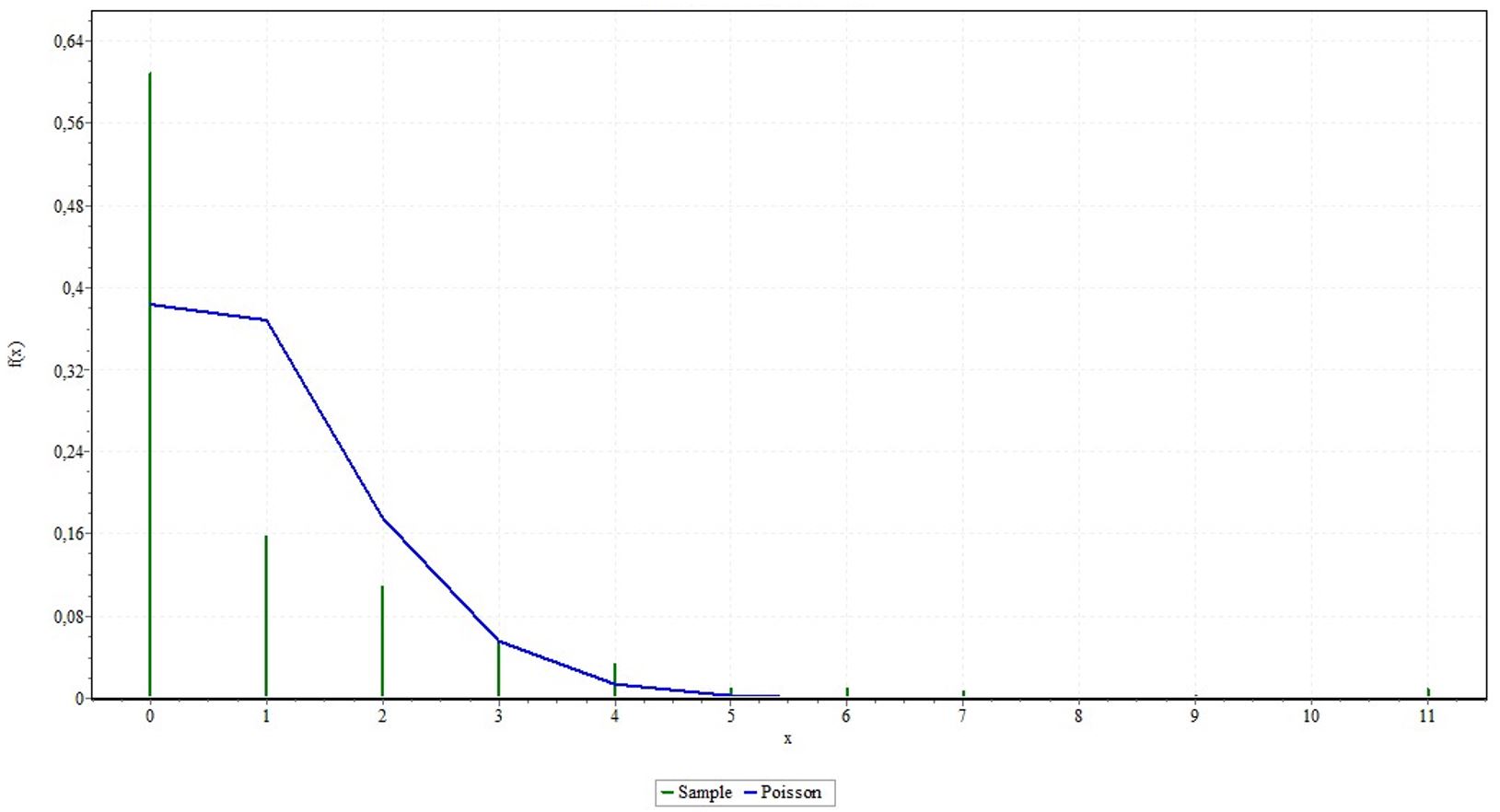
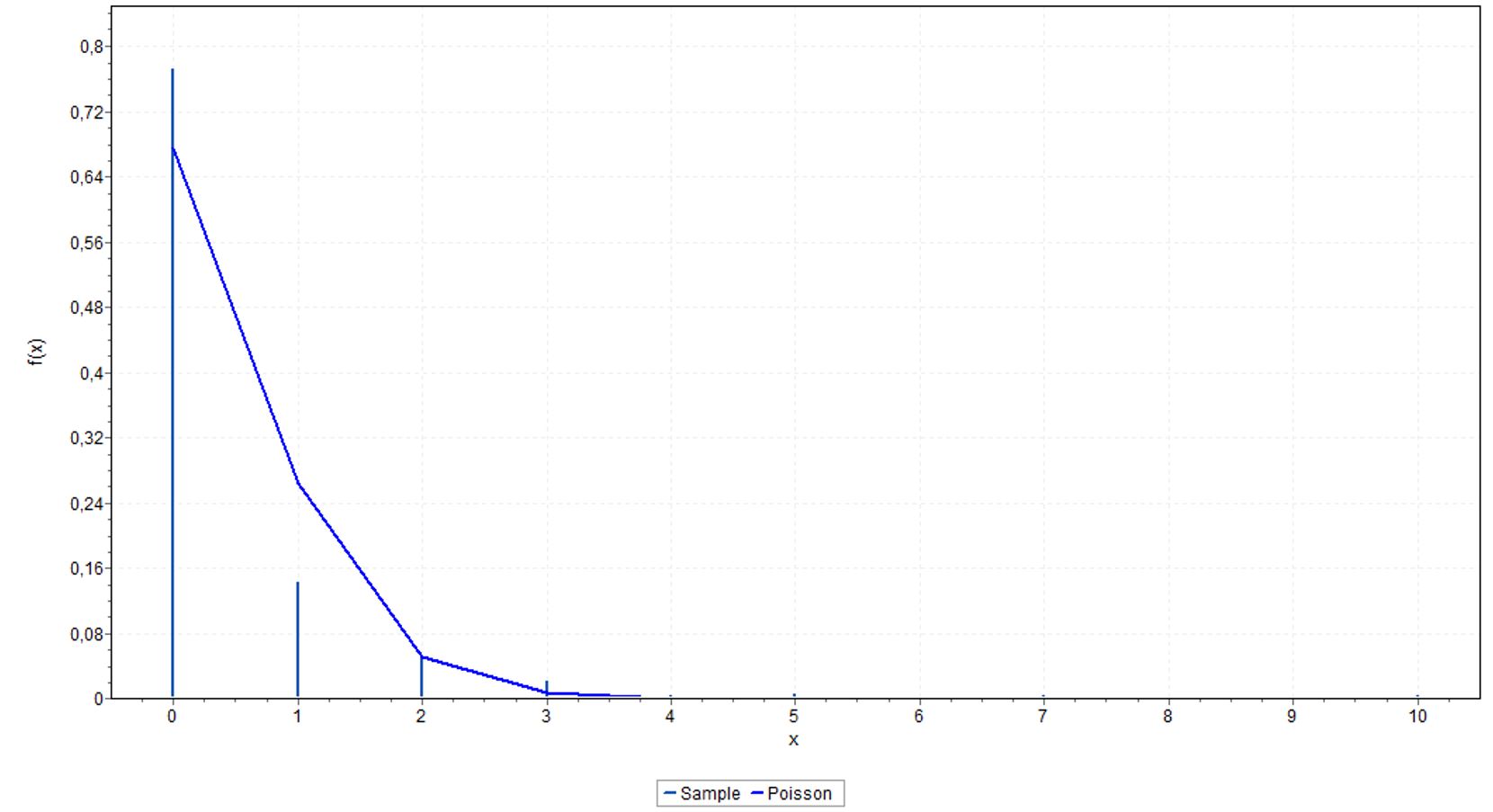
Then, we collected quantitative data in order to understand the demand profiles and the supplier delivery times variability. For demand, we used the available historic data, which comprised the year of 2017. Product were categorized and grouped as A (up to 80% of total demand), B (up to 15% of total demand) and C (up to 5% of total demand), and had their demands’ probability density functions identified through utilization of Easyfit® software (see Appendix C
Appendix C
Probability density functions for demands.
Figure 1C
Probability density function for type-A products.
Figure 2C
Probability density function for type-B products.
Figure 3C
Probability density function for type-C products.
). Data related to suppliers’ delivery time was not formally registered in hospital’s system. Although there was a contractual agreement of a 5-day limit, the involved leaders informed that eventually the replenishment time can take up to 7 days, especially in cases where the order is sent close to weekends. Therefore, we considered a triangular distribution (Law, 2016Law, A. (2016). A tutorial on how to select simulation input probability distributions. In Proceedings of the 2016 Winter Simulation Conference (pp. 1-15). USA: IEEE. http://dx.doi.org/10.1109/WSC.2016.7822083.
http://dx.doi.org/10.1109/WSC.2016.78220...
), whose pessimistic and optimistic scenarios (i.e. the identification of distribution interval) were established based on the leaders’ experience in that area. The minimum and maximum values were determined as 3 and 7 days for delivery, respectively, and a mean value of 5 days. Regarding inventory in the hospital, we collected data during 30 consecutive days of each product. Results for the sum of this inventory showed that the total lead time of the internal supply chain varied from 198 to 230 days, with an average time of approximately 211 days (see Figure 4).
We then determined cyclic and safety stocks, and the reordering points for each product contemplated in the supply chain value stream. In agreement with leadership, it was determined a delivery service level of 99% for all types of products (A, B or C) and a replenishment time of 5 days (contractually agreed). Further, calculated parameters were qualitatively assessed by leadership who adjusted those values based on their experience and certain specificities of products that the inventory policies calculation does not consider. For instance, some products had a huge size diversity, requiring at least one unit of each in stock. There was also the case of products that should not be kept in stock since they were only ordered when there was a medical request. Finally, leaders identified products whose utilization was supposed to be reduced due to the entrance of new materials and/or products, adjusting the inventory quantities for such phase-out. Such parameters were input into the simulation model construction (see Table 2).
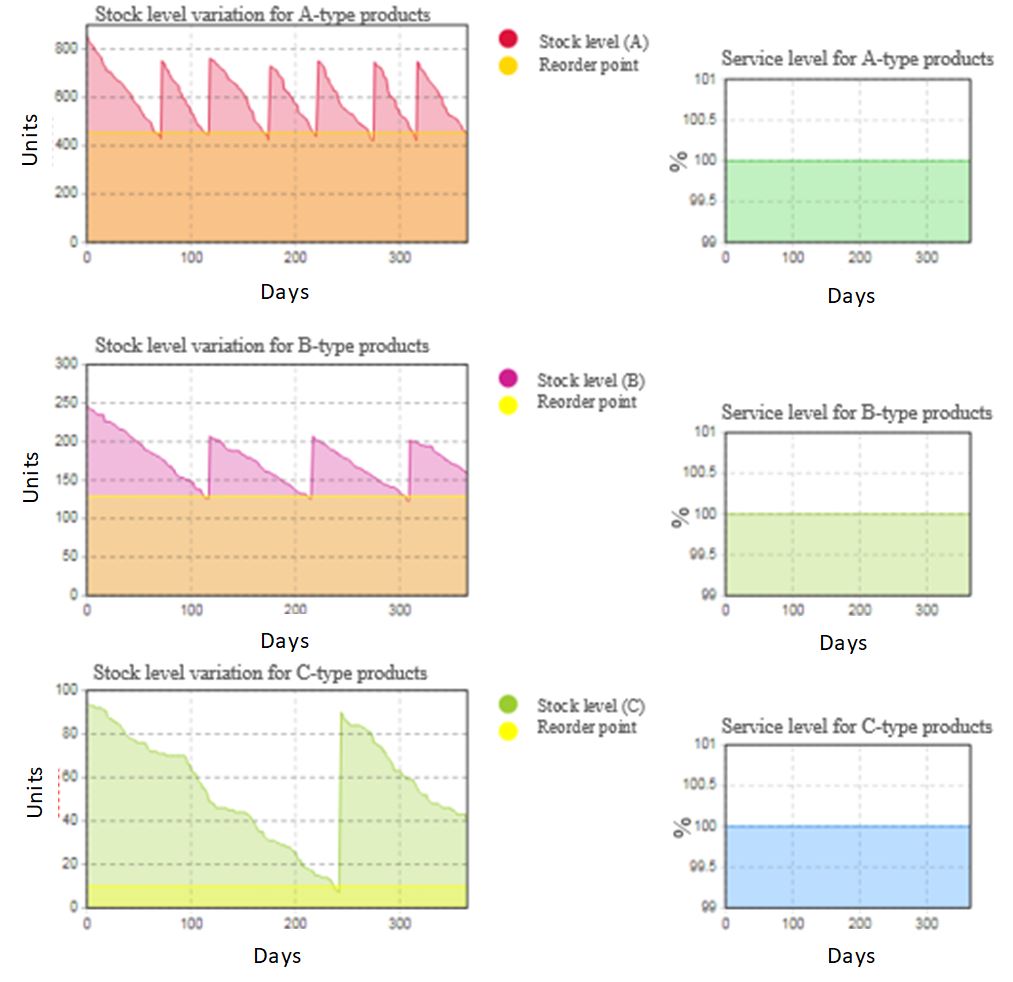
The computational simulation results are shown in Figure 5. As expected, delivery service level remained at 100% for all three simulated scenarios (product types A, B or C), meeting the first leadership expectation. Regarding lead time, the proposed inventory policy resulted in a maximum lead time of approximately 168 days, which was 20.4% lower than the average value observed during the 30-day data collection period illustrated in Figure 4. It is noteworthy that when analyzing each product type, different lead time variations were observed. For type-A products, lead time ranged from a minimum of approximately 62 days to a maximum of 130 days. For type-B products, the minimum was about 123 days and the maximum of 221 days. Finally, for type-C products, the minimum resulted in 10 days and the maximum in 233 days. These variations are shown in Table 3. Overall, simulation modelling indicated that the proposed inventory policies would meet delivery service level requirements and simultaneously reduce supply chain lead time, despite the additional improvement opportunities.
5. Conclusion
This study aimed at evaluating the impact of lean practices implementation in the internal supply chain of a healthcare organization aided by computational simulation modelling. Data from a specific product family of a Brazilian public hospital was collected to illustrate the proposed method. Two major contributions can be highlighted from this study and deserve further discussion in the subsequent sections.
5.1. Implications for theory
In theoretical terms, the proposition of a method that uses computational simulation to evaluate the impact of lean practices implementation in healthcare supply chain features a first contribution. The proposed method integrates value stream mapping of the hospital’s internal supply chain into computational simulation modelling, so that the effects of the proposed improvements are examined and validated. Considering the scarcity of studies that combine empirical approaches with analytical models, the proposed method brings a differentiated approach to analyze lean implementation in a healthcare supply chain, thus contributing to the body of knowledge in the field. Furthermore, studies concerning lean implementation in healthcare supply chain are still scarce (Borges et al., 2019Borges, G., Tortorella, G., Rossini, M., & Portioli-Staudacher, A. (2019). Lean implementation in healthcare supply chain: a scoping review. Journal of Health Organization and Management, 33(3), 304-322. http://dx.doi.org/10.1108/JHOM-06-2018-0176. PMid:31122116.
http://dx.doi.org/10.1108/JHOM-06-2018-0...
), especially when compared to other industry sectors, such as manufacturing. Therefore, the utilization of a combined methodological approach to understand lean implementation in healthcare supply chain sheds light on a research topic that still lacks a deeper understanding, entailing another contribution of our study.
5.2. Practical contributions
From a practical perspective, this research helps managers to focus their efforts related to lean implementation in healthcare organizations. The simulation model supports a more assertive decision-making process on lean implementation, allowing the organization to ensure that the quality and efficiency of healthcare is not affected, since it considers as inputs the variabilities related to suppliers and to customers. In our study, service level and lead time were used as performance parameters and both indicated that the proposed improvements may contribute to an increased supply chain efficiency. Thus, using the proposed approach, managers and leaders of healthcare organizations can check beforehand the impact of their lean improvement initiatives, providing a more effective implementation. Additionally, our study provides hospital managers arguments to customize their inventory policies according to the representativeness of the items. The simulation analysis has shown different performance outcomes based on different inventory policies (A-, B- or C-type). This result demystifies the one-size-fits-all inventory management approach currently used in this hospital, suggesting that managers must deepen their analysis and adapt their inventory policies.
5.3. Limitations and future research
Regarding this study’s limitations, it is worth mentioning some aspects. The first limitation concerns the use of a single case study to evaluate lean implementation in healthcare supply chain, which limits the results validity and generalization. This limitation entails specific research outcomes that may be derived of the particular characteristics of the studied hospital. For instance, the purchasing process in public hospital usually takes a longer time since it significantly differs from private ones. Second, the proposed model simplifies and groups products according to the ABC classification based on annual demand volume. This classification, although recommended for situations where the number of inventory items is too large to implement a specific inventory control system for each item, may blur particular demand behaviors of certain products. In this sense, data with a more accurate level of detail could contribute to a more reliable analysis. Additionally, this classification neglects other aspects that may be important depending on the product family under investigation, such as perishability. Future studies could insert additional parameters to properly categorize items and establish their inventory policies. Finally, we suggest the simulation of different control and inventory management methods, since our study considered only the continuous revision inventory management approach. Despite its greater accuracy, this approach is generally more expensive, and may be unfeasible both technically and financially for many hospital products. In this sense, future work can verify the validity of inventory policies under different control approaches, thus, determining their validity for the healthcare context.
Appendix A Semi-structured interviews script.
1. Which improvement initiatives does the organization already have?
2. Give examples of lean practices successfully implemented and the impacts they have caused.
3. Give examples of lean practices implemented that have not had the expected result.
4. What are the tasks performed in the sector?
5. Which activities do you believe take more time in your job?
6. In your opinion, what are the great improvement opportunities in the process?
Appendix B Hospital’s team members characteristics.
Table 1B. Hospital’s team members.
| Hospital member | Department or Unit | Hospital experience time (years) |
|---|---|---|
| 1 | Material Planning | 3.5 |
| 2 | Purchase | 2.5 |
| 3 | Supply coordination | 37 |
| 4 | Administrative management | 37 |
| 5 | Consigned materials | 1.5 |
| 6 | Consigned materials | 1.5 |
| 7 | Consigned materials | 2.5 |
| 8 | Warehouse | Not informed |
| 9 | Bidding | 34 |
| 10 | Financial | 32 |
| 11 | Financial | 6 |
| 12 | Healthcare management | 32 |
| 13 | Hospital Infection Control Committee | 25 |
| 14 | Hospital Infection Control Committee | 13 |
| 15 | Sterilization | 9 |
| 16 | Surgery Center | 4 |
Appendix C Probability density functions for demands.
-
How to cite this article: Borges, G. A., Tortorella, G. L., Martínez, F., & Thurer, M. (2020). Simulation-based analysis of lean practices implementation on the supply chain of a public hospital. Production, 30, e20190131. https://doi.org/10.1590/0103-6513.20190131.
References
- Adebanjo, D., Laosirihongthong, T., & Samaranayake, P. (2016). Prioritizing lean supply chain management initiatives in healthcare service operations: a fuzzy AHP approach. Production Planning and Control, 27(12), 953-966. http://dx.doi.org/10.1080/09537287.2016.1164909
» http://dx.doi.org/10.1080/09537287.2016.1164909 - Aherne, J., & Whelton, J. (Eds.). (2010). Applying lean in healthcare: a collection of international case studies Boca Raton: CRC Press. http://dx.doi.org/10.1201/EBK1439827390
» http://dx.doi.org/10.1201/EBK1439827390 - Archibald, G., Karabakal, N., & Karlsson, P. (1999). Supply chain vs. supply chain: using simulation to compete beyond the four walls. In Proceedings of the 31st Conference on Winter Simulation: a Bridge to the Future (Vol. 2, pp. 1207-1214). New York: ACM. http://dx.doi.org/10.1145/324898.325039
» http://dx.doi.org/10.1145/324898.325039 - Aronsson, H., Abrahamsson, M., & Spens, K. (2011). Developing lean and agile health care supply chains. Supply Chain Management, 16(3), 176-183. http://dx.doi.org/10.1108/13598541111127164
» http://dx.doi.org/10.1108/13598541111127164 - Banks, C. (2009). What is modeling and simulation. In J. Sokolowski & C. Banks (Eds.), Principles of modeling and simulation Hoboken: Wiley.
- Bendavid, Y., Boeck, H., & Philippe, R. (2010). Redesigning the replenishment process of medical supplies in hospitals with RFID. Business Process Management Journal, 16(6), 991-1013. http://dx.doi.org/10.1108/14637151011093035
» http://dx.doi.org/10.1108/14637151011093035 - Bhasin, S. (2011). Performance of organizations treating lean as an ideology. Business Process Management Journal, 17(6), 986-1011. http://dx.doi.org/10.1108/14637151111182729
» http://dx.doi.org/10.1108/14637151111182729 - Böhme, T., Williams, S. J., Childerhouse, P., Deakins, E., & Towill, D. (2013). Methodology challenges associated with benchmarking healthcare supply chains. Production Planning and Control, 24(10-11), 1002-1014. http://dx.doi.org/10.1080/09537287.2012.666918
» http://dx.doi.org/10.1080/09537287.2012.666918 - Borges, G., Tortorella, G., Frazzon, E., & Martinez, F. (2018, June). Simulation-based analysis of lean implementation in healthcare. In Proceedings from 25th International Annual EurOMA Conference Brussels: European Operations Management Association.
- Borges, G., Tortorella, G., Rossini, M., & Portioli-Staudacher, A. (2019). Lean implementation in healthcare supply chain: a scoping review. Journal of Health Organization and Management, 33(3), 304-322. http://dx.doi.org/10.1108/JHOM-06-2018-0176 PMid:31122116.
» http://dx.doi.org/10.1108/JHOM-06-2018-0176 - Brandão de Souza, L. (2009). Trends and approaches in lean healthcare. Leadership in Health Services, 22(2), 121-139. http://dx.doi.org/10.1108/17511870910953788
» http://dx.doi.org/10.1108/17511870910953788 - Chen, I., & Paulraj, A. (2004). Towards a theory of supply chain management: the constructs and measurements. Journal of Operations Management, 22(2), 119-150. http://dx.doi.org/10.1016/j.jom.2003.12.007
» http://dx.doi.org/10.1016/j.jom.2003.12.007 - Chiarini, A. (2013). Waste savings in patient transportation inside large hospitals using lean thinking tools and logistic solutions. Leadership in Health Services, 26(4), 356-367. http://dx.doi.org/10.1108/LHS-05-2012-0013
» http://dx.doi.org/10.1108/LHS-05-2012-0013 - Chung, C. (Ed.). (2013). Simulation modeling handbook: a practical approach London: CRC Press.
- Costa, L. B. M., Godinho Filho, M., Rentes, A. F., Bertani, T. M., & Mardegan, R. (2017). Lean healthcare in developing countries: evidence from Brazilian hospitals. The International Journal of Health Planning and Management, 32(1), e99-e120. http://dx.doi.org/10.1002/hpm.2331 PMid:26681656.
» http://dx.doi.org/10.1002/hpm.2331 - D’Andreamatteo, A., Ianni, L., Lega, F., & Sargiacomo, M. (2015). Lean in healthcare: a comprehensive review. Health Policy, 119(9), 1197-1209. http://dx.doi.org/10.1016/j.healthpol.2015.02.002 PMid:25737260.
» http://dx.doi.org/10.1016/j.healthpol.2015.02.002 - Dias, M., Martins, M., & Navarro, N. (2012). Adverse outcome screening in hospitalizations of the Brazilian Unified Health System. Revista de Saude Publica, 46(4), 719-729. http://dx.doi.org/10.1590/S0034-89102012005000054 PMid:22832808.
» http://dx.doi.org/10.1590/S0034-89102012005000054 - Dickson, E., Anguelov, Z., Vetterick, D., Eller, A., & Singh, S. (2009). Use of lean in the emergency department: a case series of 4 hospitals. Annals of Emergency Medicine, 54(4), 504-510. http://dx.doi.org/10.1016/j.annemergmed.2009.03.024 PMid:19423187.
» http://dx.doi.org/10.1016/j.annemergmed.2009.03.024 - Dobrzykowski, D., Deilami, V., Hong, P., & Kim, S. (2014). A structured analysis of operations and supply chain management research in healthcare (1982–2011). International Journal of Production Economics, 147, 514-530. http://dx.doi.org/10.1016/j.ijpe.2013.04.055
» http://dx.doi.org/10.1016/j.ijpe.2013.04.055 - Dooner, R. (2014). How supply chain management can help to control health-care costs. CSCMP’s Supply Chain Quarterly, 8(3), 50-53.
- Duggan, K. (2012). Creating mixed model value streams: practical lean techniques for building to demand New York: Productivity Press.
- Eisenhardt, K. (1989). Building theories from case study research. Academy of Management Review, 14(4), 532-550. http://dx.doi.org/10.5465/amr.1989.4308385
» http://dx.doi.org/10.5465/amr.1989.4308385 - Ernst, R., & Cohen, M. (1990). Operations related groups (ORGs): a clustering procedure for production/inventory systems. Journal of Operations Management, 9(4), 574-598. http://dx.doi.org/10.1016/0272-6963(90)90010-B
» http://dx.doi.org/10.1016/0272-6963(90)90010-B - Farrokhi, F. R., Gunther, M., Williams, B., & Blackmore, C. C. (2013). Application of lean methodology for improved quality and efficiency in operating room instrument availability. Journal for Healthcare Quality, 37(5), 277-286 PMid:
- Fillingham, D. (2007). Can lean save lives? Leadership in Health Services, 20(4), 231-241. http://dx.doi.org/10.1108/17511870710829346 PMid:20698096.
» http://dx.doi.org/10.1108/17511870710829346 - Fogliatto, F., Anzanello, M., Tortorella, G., Schneider, D., Pereira, C., & Schaan, B. (2018). A Six Sigma approach to analyze time-to-assembly variance of surgical trays in a sterile services department. Journal for Healthcare Quality, 40(3), e46-e53. http://dx.doi.org/10.1097/JHQ.0000000000000078 PMid:28346244.
» http://dx.doi.org/10.1097/JHQ.0000000000000078 - Frazzon, E., Tortorella, G., Dávalos, R., Holtz, T., & Coelho, L. (2017). Simulation-based analysis of a supplier-manufacturer relationship in lean supply chains. International Journal of Lean Six Sigma, 8(3), 262-274. http://dx.doi.org/10.1108/IJLSS-03-2016-0009
» http://dx.doi.org/10.1108/IJLSS-03-2016-0009 - Ganeshan, R., Boone, T., & Stenger, A. (2001). The impact of inventory and flow planning parameters on supply chain performance: an exploratory study. International Journal of Production Economics, 71(1-3), 111-118. http://dx.doi.org/10.1016/S0925-5273(00)00109-2
» http://dx.doi.org/10.1016/S0925-5273(00)00109-2 - Graban, M. (2016). Lean hospitals: improving quality, patient safety, and employee engagement New York: CRC Press. http://dx.doi.org/10.1201/b11740
» http://dx.doi.org/10.1201/b11740 - Gunasekaran, A., Patel, C., & McGaughey, R. (2004). A framework for supply chain performance measurement. International Journal of Production Economics, 87(3), 333-347. http://dx.doi.org/10.1016/j.ijpe.2003.08.003
» http://dx.doi.org/10.1016/j.ijpe.2003.08.003 - Habidin, N. F., Shazali, N. A., Ali, N., Khaidir, N. A., & Jamaludin, N. H. (2014). Exploring lean healthcare practice and supply chain innovation for Malaysian healthcare industry. International Journal of Business Excellence, 7(3), 394-410. http://dx.doi.org/10.1504/IJBEX.2014.060782
» http://dx.doi.org/10.1504/IJBEX.2014.060782 - Haddad, M., Zouein, P., Salem, J., & Otayek, R. (2016). Case study of lean in hospital admissions to inspire culture change. Engineering Management Journal, 28(4), 209-223. http://dx.doi.org/10.1080/10429247.2016.1234896
» http://dx.doi.org/10.1080/10429247.2016.1234896 - Hasle, P., Nielsen, A., & Edwards, K. (2016). Application of lean manufacturing in hospitals: the need to consider maturity, complexity, and the value concept. Human Factors and Ergonomics in Manufacturing & Service Industries, 26(4), 430-442. http://dx.doi.org/10.1002/hfm.20668
» http://dx.doi.org/10.1002/hfm.20668 - Hines, P., & Rich, N. (1997). The seven value stream mapping tools. International Journal of Operations & Production Management, 17(1), 46-64. http://dx.doi.org/10.1108/01443579710157989
» http://dx.doi.org/10.1108/01443579710157989 - Ingallis, R. (1998). The value of simulation in modeling supply chains. In Winter Simulation Conference Proceedings (Vol. 2, pp. 1371-1375). New York: Association for Computing Machinery. http://dx.doi.org/10.1109/WSC.1998.746004
» http://dx.doi.org/10.1109/WSC.1998.746004 - Ivanov, D. (2016). Operations and supply chain simulation with AnyLogic 7.2 (2nd ed.). Berlin: School of Economics and Law.
- Jahre, M., Dumoulin, L., Greenhalgh, L., Hudspeth, C., Limlim, P., & Spindler, A. (2012). Improving health in developing countries: reducing complexity of drug supply chains. Journal of Humanitarian Logistics and Supply Chain Management, 2(1), 54-84. http://dx.doi.org/10.1108/20426741211226000
» http://dx.doi.org/10.1108/20426741211226000 - Jin, M., Switzer, M., & Agirbas, G. (2008). Six Sigma and Lean in healthcare logistics centre design and operation: a case at North Mississippi Health Services. International Journal of Six Sigma and Competitive Advantage, 4(3), 270-288. http://dx.doi.org/10.1504/IJSSCA.2008.021840
» http://dx.doi.org/10.1504/IJSSCA.2008.021840 - Kane, R., Shamliyan, T., Mueller, C., Duval, S., & Wilt, T. (2007). The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Medical Care, 45(12), 1195-1204. http://dx.doi.org/10.1097/MLR.0b013e3181468ca3 PMid:18007170.
» http://dx.doi.org/10.1097/MLR.0b013e3181468ca3 - Kates, S. (2014). Lean business model and implementation of a geriatric fracture center. Clinics in Geriatric Medicine, 30(2), 191-205. http://dx.doi.org/10.1016/j.cger.2014.01.002 PMid:24721360.
» http://dx.doi.org/10.1016/j.cger.2014.01.002 - Khorasani, S., Maghazei, O., & Cross, J. (2015). A structured review of lean supply chain management in health care. In Proceedings of the International Annual Conference of the American Society for Engineering Management (p. 1). Huntsville: ASEM.
- Kimsey, D. (2010). Lean methodology in health care. AORN Journal, 92(1), 53-60. http://dx.doi.org/10.1016/j.aorn.2010.01.015 PMid:20619772.
» http://dx.doi.org/10.1016/j.aorn.2010.01.015 - Krajewski, L., Malhotra, M., & Ritzman, L. (2016). Operations management: processes and supply chains (10th ed.). Upper Saddle River: Pearson.
- Kumar, A., Ozdamar, L., & Ning Zhang, C. (2008). Supply chain redesign in the healthcare industry of Singapore. Supply Chain Management, 13(2), 95-103. http://dx.doi.org/10.1108/13598540810860930
» http://dx.doi.org/10.1108/13598540810860930 - Kumar, S., Swanson, E., & Tran, T. (2009). RFID in the healthcare supply chain: usage and application. International Journal of Health Care Quality Assurance, 22(1), 67-81. http://dx.doi.org/10.1108/09526860910927961 PMid:19284172.
» http://dx.doi.org/10.1108/09526860910927961 - Law, A. (2016). A tutorial on how to select simulation input probability distributions. In Proceedings of the 2016 Winter Simulation Conference (pp. 1-15). USA: IEEE. http://dx.doi.org/10.1109/WSC.2016.7822083
» http://dx.doi.org/10.1109/WSC.2016.7822083 - Lim, J., Norman, B., & Rajgopal, J. (2017). Process redesign and simplified policies for more effective vaccine inventory management. Engineering Management Journal, 29(1), 17-25. http://dx.doi.org/10.1080/10429247.2016.1277446
» http://dx.doi.org/10.1080/10429247.2016.1277446 - Liu, M., Zhang, L., & Zhang, Z. (2015). Optimal scheduling of logistical support for medical resources order and shipment in community health service centers. Journal of Industrial Engineering and Management, 8(5), 1362. http://dx.doi.org/10.3926/jiem.1463
» http://dx.doi.org/10.3926/jiem.1463 - Liu, T., Shen, A., Hu, X., Tong, G., Gu, W., & Yang, S. (2016). SPD-based logistics management model of medical consumables in hospitals. Iranian Journal of Public Health, 45(10), 1288-1299. PMid:27957435.
- Lummus, R., & Vokurka, R. (1999). Defining supply chain management: a historical perspective and practical guidelines. Industrial Management & Data Systems, 99(1), 11-17. http://dx.doi.org/10.1108/02635579910243851
» http://dx.doi.org/10.1108/02635579910243851 - Machado, C., Carvalho, J. C., & Maia, A. (2013). Vendor managed inventory (VMI): evidences from lean deployment in healthcare. Strategic Outsourcing, 6(1), 8-24. http://dx.doi.org/10.1108/17538291311316045
» http://dx.doi.org/10.1108/17538291311316045 - Machado, C., Scavarda, A., & Vaccaro, G. (2014). Lean healthcare supply chain management: minimizing waste and costs. Independent Journal of Management & Production, 5(4), 1071-1088. http://dx.doi.org/10.14807/ijmp.v5i4.245
» http://dx.doi.org/10.14807/ijmp.v5i4.245 - Mapes, J., Szwejczewski, M., & New, C. (2000). Process variability and its effect on plant performance. International Journal of Operations & Production Management, 20(7), 792-808. http://dx.doi.org/10.1108/01443570010330775
» http://dx.doi.org/10.1108/01443570010330775 - McKone‐Sweet, K., Hamilton, P., & Willis, S. (2005). The ailing healthcare supply chain: a prescription for change. The Journal of Supply Chain Management, 41(1), 4-17. http://dx.doi.org/10.1111/j.1745-493X.2005.tb00180.x
» http://dx.doi.org/10.1111/j.1745-493X.2005.tb00180.x - Meneghini, M., Anzanello, M., Kahmann, A., & Tortorella, G. (2018). Quantitative demand forecasting adjustment based on qualitative factors: case study at a fast food restaurant. Sistemas & Gestão, 13(1), 68-80. http://dx.doi.org/10.20985/1980-5160.2018.v13n1.1188
» http://dx.doi.org/10.20985/1980-5160.2018.v13n1.1188 - Mentzer, J., Dewitt, W., Keebler, J., Min, S., Nix, N., Smith, C., & Zacharia, Z. (2001). Defining supply chain management. Journal of Business Logistics, 22(2), 1-25. http://dx.doi.org/10.1002/j.2158-1592.2001.tb00001.x
» http://dx.doi.org/10.1002/j.2158-1592.2001.tb00001.x - Narayanamurthy, G., & Gurumurthy, A. (2018). Is the hospital lean? A mathematical model for assessing the implementation of lean thinking in healthcare institutions. Operations Research for Health Care, 18, 84-98. http://dx.doi.org/10.1016/j.orhc.2017.05.002
» http://dx.doi.org/10.1016/j.orhc.2017.05.002 - Nelson, D., Moody, P., & Stegner, J. (2001). The purchasing machine New York; The Free Press.
- Olhager, J., & Persson, F. (2006). Simulating production and inventory control systems: a learning approach to operational excellence. Production Planning and Control, 17(2), 113-127. http://dx.doi.org/10.1080/09537280500223921
» http://dx.doi.org/10.1080/09537280500223921 - Oliveira, J., Lima, R., & Montevechi, J. (2016). Perspectives and relationships in Supply Chain Simulation: A systematic literature review. Simulation Modelling Practice and Theory, 62, 166-191. http://dx.doi.org/10.1016/j.simpat.2016.02.001
» http://dx.doi.org/10.1016/j.simpat.2016.02.001 - Papalexi, M., Bamford, D., & Dehe, B. (2016). A case study of kanban implementation within the pharmaceutical supply chain. International Journal of Logistics Research and Applications, 19(4), 239-255. http://dx.doi.org/10.1080/13675567.2015.1075478
» http://dx.doi.org/10.1080/13675567.2015.1075478 - Persson, F., & Olhager, J. (2002). Performance simulation of supply chain designs. International Journal of Production Economics, 77(3), 231-245. http://dx.doi.org/10.1016/S0925-5273(00)00088-8
» http://dx.doi.org/10.1016/S0925-5273(00)00088-8 - Plsek, P. E., & Greenhalgh, T. (2001). The challenge of complexity in health care: an introduction. BMJ, 323(7314), 625-628. http://dx.doi.org/10.1136/bmj.323.7313.625 PMid:11557716.
» http://dx.doi.org/10.1136/bmj.323.7313.625 - Radnor, Z., Holweg, M., & Waring, J. (2012). Lean in healthcare: the unfilled promise? Social Science & Medicine, 74(3), 364-371. http://dx.doi.org/10.1016/j.socscimed.2011.02.011 PMid:21414703.
» http://dx.doi.org/10.1016/j.socscimed.2011.02.011 - Regis, T., Gohr, C., & Santos, L. (2018). Lean healthcare implementation: experiences and lessons learned from Brazilian hospitals. Revista de Administração de Empresas, 58(1), 30-43.
- Rivard-Royer, H., Landry, S., & Beaulieu, M. (2002). Hybrid stockless: a case study. Lessons for health-care supply chain integration. International Journal of Operations & Production Management, 22(4), 412-424. http://dx.doi.org/10.1108/01443570210420412
» http://dx.doi.org/10.1108/01443570210420412 - Roberts, R., Wilson, A., & Quezado, Z. (2017). Using Lean Six Sigma methodology to improve quality of the anesthesia supply chain in a pediatric hospital. Anesthesia and Analgesia, 124(3), 922-924. http://dx.doi.org/10.1213/ANE.0000000000001621 PMid:27749347.
» http://dx.doi.org/10.1213/ANE.0000000000001621 - Robinson, S. (2004). Simulation: the practice of model development and use Chichester: Wiley.
- Rother, M., & Shook, J. (2003). Learning to see: value stream mapping to add value and eliminate muda Cambridge: Lean Enterprise Institute.
- Sakurada, N., & Miyake, D. (2009). Aplicação de simuladores de eventos discretos no processo de modelagem de sistemas de operações de serviços. Gestão & Produção, 16(1), 25-43. http://dx.doi.org/10.1590/S0104-530X2009000100004
» http://dx.doi.org/10.1590/S0104-530X2009000100004 - Savino, M., Mazza, A., & Marchetti, B. (2015). Lean manufacturing within critical healthcare supply chain: an exploratory study through value chain simulation. International Journal of Procurement Management, 8(1-2), 3-24. http://dx.doi.org/10.1504/IJPM.2015.066285
» http://dx.doi.org/10.1504/IJPM.2015.066285 - Schwarting, D., Bitar, J., Arya, Y., & Pfeiffer, T. (2011). The transformative hospital supply chain: balancing costs with quality USA: Booz & Company.
- Setijono, D., Mohajeri Naraghi, A., & Pavan Ravipati, U. (2010). Decision support system and the adoption of lean in a swedish emergency ward: balancing supply and demand towards improved value stream. International Journal of Lean Six Sigma, 1(3), 234-248. http://dx.doi.org/10.1108/20401461011075026
» http://dx.doi.org/10.1108/20401461011075026 - Shah, R., Goldstein, S., Unger, B., & Henry, T. (2008). Explaining anomalous high performance in a health care supply chain. Decision Sciences, 39(4), 759-789. http://dx.doi.org/10.1111/j.1540-5915.2008.00211.x
» http://dx.doi.org/10.1111/j.1540-5915.2008.00211.x - Sharma, V., Abel, J., Al‐Hussein, M., Lennerts, K., & Pfründer, U. (2007). Simulation application for resource allocation in facility management processes in hospitals. Facilities, 25(13/14), 493-506. http://dx.doi.org/10.1108/02632770710822599
» http://dx.doi.org/10.1108/02632770710822599 - Sheikh, A., Sood, H., & Bates, D. (2015). Leveraging health information technology to achieve the “triple aim” of healthcare reform. Journal of the American Medical Informatics Association, 22(4), 849-856. http://dx.doi.org/10.1093/jamia/ocv022 PMid:25882032.
» http://dx.doi.org/10.1093/jamia/ocv022 - Silva, S. (2011). The organization of regional and integrated healthcare delivery systems: challenges facing Brazil’s Unified Health System. Ciência & Saúde Coletiva, 16(6), 2753-2764. PMid:21709973.
- Simangunsong, E., Hendry, L. C., & Stevenson, M. (2011). Supply chain uncertainty: a review and theoretical foundation for future research. International Journal of Production Research, 50(16), 4493-4523. http://dx.doi.org/10.1080/00207543.2011.613864
» http://dx.doi.org/10.1080/00207543.2011.613864 - Teichgräber, U., & De Bucourt, M. (2012). Applying value stream mapping techniques to eliminate non-value-added waste for the procurement of endovascular stents. European Journal of Radiology, 81(1), e47-e52. http://dx.doi.org/10.1016/j.ejrad.2010.12.045 PMid:21316173.
» http://dx.doi.org/10.1016/j.ejrad.2010.12.045 - Terra, J., & Berssaneti, F. (2018). Application of lean healthcare in hospital services: a review of the literature (2007 to 2017). Production, 28, e20180009. http://dx.doi.org/10.1590/0103-6513.20180009
» http://dx.doi.org/10.1590/0103-6513.20180009 - Tortorella, G., Miorando, R., & Tlapa, D. (2017a). Implementation of lean supply chain: an empirical research on the effect of context. The TQM Journal, 29(4), 610-623. http://dx.doi.org/10.1108/TQM-11-2016-0102
» http://dx.doi.org/10.1108/TQM-11-2016-0102 - Tortorella, G., Fogliatto, F., Anzanello, M., Marodin, G., Garcia, M., & Reis Esteves, R. (2017b). Making the value flow: application of value stream mapping in a Brazilian public healthcare organization. Total Quality Management & Business Excellence, 28(13-14), 1544-1558. http://dx.doi.org/10.1080/14783363.2016.1150778
» http://dx.doi.org/10.1080/14783363.2016.1150778 - Tortorella, G., Silva, G., Campos, L. M., Pizzeta, C., Latosinski, A., & Soares, A. (2018). Productivity improvement in solid waste recycling centres through lean implementation aided by multi-criteria decision analysis. Benchmarking, 25(5), 1480-1499. http://dx.doi.org/10.1108/BIJ-01-2017-0013
» http://dx.doi.org/10.1108/BIJ-01-2017-0013 - Waring, J., & Bishop, S. (2010). Lean healthcare: rhetoric, ritual and resistance. Social Science & Medicine, 71(7), 1332-1340. http://dx.doi.org/10.1016/j.socscimed.2010.06.028 PMid:20702013.
» http://dx.doi.org/10.1016/j.socscimed.2010.06.028 - Whittington, J. W., Nolan, K., Lewis, N., & Torres, T. (2015). Pursuing the triple aim: the first 7 years. The Milbank Quarterly, 93(2), 263-300. http://dx.doi.org/10.1111/1468-0009.12122 PMid:26044630.
» http://dx.doi.org/10.1111/1468-0009.12122 - Wijewardana, R., & Rupasinghe, T. (2013). Applicability of Lean Healthcare in Sri Lankan Healthcare Supply Chains. International Journal of Supply Chain Management, 2(4), 42-49.
- Womack, J., Byrne, A., Fiume, O., Kaplan, G., & Toussaint, J. (2005). Going lean in health care Cambridge: Institute for Healthcare Improvement.
- Young, T., Brailsford, S., Connell, C., Davies, R., Harper, P., & Klein, J. (2004). Using industrial processes to improve patient care. BMJ, 328(7432), 162-164. http://dx.doi.org/10.1136/bmj.328.7432.162 PMid:14726351.
» http://dx.doi.org/10.1136/bmj.328.7432.162
Publication Dates
-
Publication in this collection
15 June 2020 -
Date of issue
2020
History
-
Received
18 Sept 2019 -
Accepted
29 Apr 2020