Abstract
Background
Venous thromboembolism (VTE) is a silent and potentially lethal disease that affects a considerable proportion of hospitalized patients. It has high morbidity and mortality and is responsible for a heavy financial burden on healthcare systems. However, VTE can be prevented using prophylaxis measures that have been established in the literature. Nonetheless, in the real world, mean rates of appropriately administered VTE prophylaxis are lower than 50%.
Objectives
To define the epidemiological profile of patients with VTE in a University Hospital and the rate of appropriately administered VTE prophylaxis at that service and to identify measures to improve the rate.
Methods
A cross-sectional, observational study was conducted with data collected from the medical records of patients who met the inclusion criteria. The rates of correct VTE prophylaxis prescribed to clinical and surgical patients were compared, assessed according to guidelines published by the Brazilian Society of Angiology and Vascular Surgery (SBACV), based on VTE risk classification.
Results
The overall rate of correctly-prescribed VTE prophylaxis was 42.1%, while 57.9% of patients were not managed correctly in this respect. Clinical patients had a 52.9% rate of appropriate prophylaxis, while the equivalent rate for surgical patients was 37.5%.
Conclusions
Rates of correctly-prescribed VTE prophylaxis are still lower than they should be. Ongoing education, measures to encourage bedside risk stratification, and improvements to the electronic prescription system could increase appropriate VTE prophylaxis rates.
Keywords:
venous thromboembolism; venous thrombosis; emboli; thrombosis
Resumo
Contexto
O tromboembolismo venoso (TEV) é uma doença silenciosa e potencialmente letal que acomete parcela importante dos pacientes hospitalizados. Com alta morbimortalidade e elevado custo financeiro para o sistema de saúde, o TEV pode ser prevenido com uso da profilaxia, já estabelecida pela literatura. No mundo real, a profilaxia para TEV possui média de adequação inferior a 50%.
Objetivos
Definir o perfil epidemiológico do doente com TEV em um hospital universitário e a taxa de adequação da profilaxia para TEV no referido serviço, além de determinar meios para melhorá-la.
Métodos
Estudo transversal observacional realizado pela coleta de dados no prontuário médico dos pacientes que preencheram critérios de inclusão. Comparou-se a taxa de adequação da profilaxia para TEV prescrita para pacientes clínicos e cirúrgicos, segundo diretrizes da Sociedade Brasileira de Angiologia e Cirurgia Vascular (SBACV), de acordo com sua classificação de risco para TEV.
Resultados
A taxa global de adequação das prescrições de profilaxia para TEV foi de 42,1% versus 57,9% de inadequação. Pacientes clínicos obtiveram taxa de adequação de 52,9%, enquanto pacientes cirúrgicos obtiveram taxa de adequação de 37,5%.
Conclusões
As taxas de prescrição adequada para profilaxia para TEV ainda se encontram aquém do esperado. Educação continuada, estímulo à aplicação da estratificação de risco à beira do leito e adequações no sistema de prescrição eletrônica podem aumentar as taxas de prescrição adequada para profilaxia de TEV.
Palavras-chave:
tromboembolia venosa; trombose venosa; embolia; trombose
INTRODUCTION
Pharmaceutical and mechanical prophylactic measures to prevent venous thromboembolism (VTE) are well-established in international consensuses, for both clinical and surgical patients, 11 Guyatt GH, Eikelboom JW, Gould MK, et al. Approach to outcome measurement in the prevention of thrombosis in surgical and medical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e185S-94S. http://dx.doi.org/10.1378/chest.11-2289.
http://dx.doi.org/10.1378/chest.11-2289...
,22 Caprini JA, Arcelus JI, Reyna JJ. Effective risk stratification of surgical and nonsurgical patients for venous thromboembolic disease. Semin Hematol. 2001;38:12-9. http://dx.doi.org/10.1016/S0037-1963(01)90094-0.
http://dx.doi.org/10.1016/S0037-1963(01...
based on risk stratification models. 33 Stinnett JM, Pendleton R, Skordos L, Wheeler M, Rodgers GM. Venous thromboembolism prophylaxis in medically ill patients and the development of strategies to improve prophylaxis rates. Am J Hematol. 2005;78(3):167-72. http://dx.doi.org/10.1002/ajh.20281.
http://dx.doi.org/10.1002/ajh.20281 ...
4 Jacobson BF, Louw S, Buller H, et al. Venous thromboembolism: prophylactic and therapeutic practice guideline. S Afr Med J. 2013;103(4):261-7. http://dx.doi.org/10.7196/SAMJ.6706.
http://dx.doi.org/10.7196/SAMJ.6706 ...
-55 Caiafa JS, Bastos MD. Programa de profilaxia do tromboembolismo venoso do Hospital Naval Marcílio Dias: um modelo de educação continuada. J Vasc Bras. 2002;1:103-12. However, many Brazilian 55 Caiafa JS, Bastos MD. Programa de profilaxia do tromboembolismo venoso do Hospital Naval Marcílio Dias: um modelo de educação continuada. J Vasc Bras. 2002;1:103-12. ,66 Engelhorn CA, Nardelli J, Iwamura AP, Salgado LD, Hartmann MO, Witt NC. Drug prophylaxis of deep vein thrombosis in patients submitted to trauma surgery in a university hospital. J Vasc Bras. 2012;11(2):97-101. http://dx.doi.org/10.1590/S1677-54492012000200005.
http://dx.doi.org/10.1590/S1677-5449201...
and international publications show that, in the real world, approximately 50% of patients at risk of VTE are not being prescribed chemical prophylaxis when it is indicated, or are being given inappropriate prophylaxis. 77 Goldhaber SZ. DVT prevention: what is happening in the “real world”? Semin Thromb Hemost. 2003;29(Suppl 1):23-31. http://dx.doi.org/10.1055/s-2003-45414.
http://dx.doi.org/10.1055/s-2003-45414 ...
,88 Deheinzelin D, Braga A, Martins L, et al. Incorrect use of thromboprophylaxis for venous thromboembolism in medical and surgical patients: results of a multicentric, observational and cross‐sectional study in Brazil. J Thromb Haemost. 2006;4(6):1266-70. http://dx.doi.org/10.1111/j.1538-7836.2006.01981.x.
http://dx.doi.org/10.1111/j.1538-7836.2...
Rates of correctly-prescribed prophylaxis vary across different countries and different services from 2 to 92%. 99 Carneiro JLDA, Targueta GP, Marino LO. Avaliação da profilaxia do tromboembolismo venoso em hospital de grande porte; Evaluation of venous thromboembolism prophylaxis in a high complexity hospital. Rev Col Bras Cir. 2010;37(3):204-10. http://dx.doi.org/10.1590/S0100-69912010000300008.
http://dx.doi.org/10.1590/S0100-6991201...
10 Marchi C, Schlup IB, Lima CAD, Schlup HA. Avaliação da profilaxia da trombose venosa profunda em um hospital geral. J Vasc Bras. 2005;4:171-5. -1111 Cohen AT, Tapson VF, Bergmann JF, et al. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet. 2008;371(9610):387-94. http://dx.doi.org/10.1016/S0140-6736(08)60202-0.
http://dx.doi.org/10.1016/S0140-6736(08...
According to the ENDORSE study, Brazil has inappropriate prophylaxis rates of 41% for clinical patients and 54% for surgical patients. 1111 Cohen AT, Tapson VF, Bergmann JF, et al. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet. 2008;371(9610):387-94. http://dx.doi.org/10.1016/S0140-6736(08)60202-0.
http://dx.doi.org/10.1016/S0140-6736(08...
Some Brazilian studies have found even higher rates of up to 61% for clinical and surgical patients. 1212 Carandina RF. Revisão sistemática e metanálise do perfil de risco e profilaxia de tromboembolismo venoso no Brasil e no mundo. J Vasc Bras. 2016;15:339-40.
In addition to the morbidity and mortality that a hospital stay complicated by VTE can cause (2 million cases of deep venous thrombosis (DVT) and 200 thousand deaths/year in the United States, for example), the financial costs of the disease are also a cause for concern among administrators and managers. In one University Hospital in Brazil, the in-hospital VTE treatment cost, to the point at which therapeutic levels are achieved, varied from US$ 69.11 when treated with low molecular weight heparin (LMWH) to US$ 88.39, when unfractionated heparin (UFH) was used, covering only the costs of the materials and medications employed, excluding the infusion pumps. 1313 Argenta C, Beltrami L. Análise de custo-minimização do uso de heparina não-fracionada e enoxaparina em uma coorte de pacientes em tratamento de tromboembolismo venoso [dissertação]. Porto Alegre: Universidade Federal do Rio Grande do Sul; 2007 [citado 2018 out 16]. http://www.lume.ufrgs.br/handle/10183/11453
http://www.lume.ufrgs.br/handle/10183/1...
Much higher sums are observed when the full treatment provided for this disease over a 90-day period with home care is considered: a retrospective cohort study in Canada reported figures of US$ 9,347.00 when treated with LMWH and US$ 11,930.00 when treated with UFH. 1414 Spyropoulos AC, Hurley JS, Ciesla GN, Lissovoy G. Management of acute proximal deep vein thrombosis: pharmacoeconomic evaluation of outpatient treatment with enoxaparin vs inpatient treatment with unfractionated heparin. Chest. 2002;122(1):108-14. http://dx.doi.org/10.1378/chest.122.1.108.
http://dx.doi.org/10.1378/chest.122.1.1...
According to Brazilian and international guidelines, introduction of Hospital VTE Prevention Commissions (HVTEPC) would be an important element for improving VTE prevention. 1515 Edo A, Fa B, Melo DSÂ, Alves da Costa TD, Fernandes MC, Fernandes MC. Fatores de risco e profilaxia para tromboembolismo venoso em hospitais da cidade de Manaus. J Bras Pneumol. 2009;35(2):114-121.
16 Rocha ATC, Paiva EFD, Araújo DMD, et al. Impacto de um programa para profilaxia de tromboembolismo venoso em pacientes clínicos em quatro hospitais de Salvador. Rev Assoc Med Bras. 2010;56(2):197-203. http://dx.doi.org/10.1590/S0104-42302010000200019.
http://dx.doi.org/10.1590/S0104-4230201...
-1717 Sociedade Brasileira de Angiologia e de Cirurgia Vascular – SBACV. Normas de orientação clínica para a prevenção, o diagnóstico e o tratamento da trombose venosa profunda. J Vasc Bras. 2005;2005:S185-94. Although VTE prophylaxis is well-established in Brazilian and international consensuses, it is disconcerting that it is still not being appropriately administered at Brazilian health services.
São Paulo’s state universities run the largest and most important university hospitals outside of the state capital and are responsible for providing care to a significant proportion of the population that is dependent on the Brazilian National Health Service (SUS - Sistema Único de Saúde). Implementation of HVTEPC is being rolled out timidly at these institutions and it is necessary to conduct a wide-ranging survey of the true state of VTE prophylaxis.
The objectives of this study were to assess the risk profile of patients admitted to a public university hospital in Brazil, determine rates of inappropriate VTE prophylaxis, identify the causes of these failures, and suggest measures to solve the problem.
METHODS
This is a cross-sectional, observational study investigating adult patients over the age of 18 years admitted to a public university hospital in Brazil and treated by the SUS, from October 2015 to February 2016, by orthopedic surgery, general surgery, gastrointestinal surgery, vascular surgery, urology, gynecology, internal medicine, and intensive care specialties. Patients already assessed during previous admissions were not reassessed and pregnant women, patients with contraindications to anticoagulants, with indications for vena cava filters, on full anticoagulation, or not meeting the inclusion criteria outlined above were all excluded.
Data were collected from information on the electronic medical records of patients admitted to the hospital using MV-PEP® software, with prior authorization from the hospital’s Research Ethics Committee and consent from the physician responsible for each specialty, but without informing the treating teams in advance.
The sample size was defined after a statistical assessment using preliminary data from a pilot study with information on 80 patients. The sample size was estimated at 500 patients, with similar numbers of patients from each specialty. Data were collected at random as patients were admitted during the data collection period.
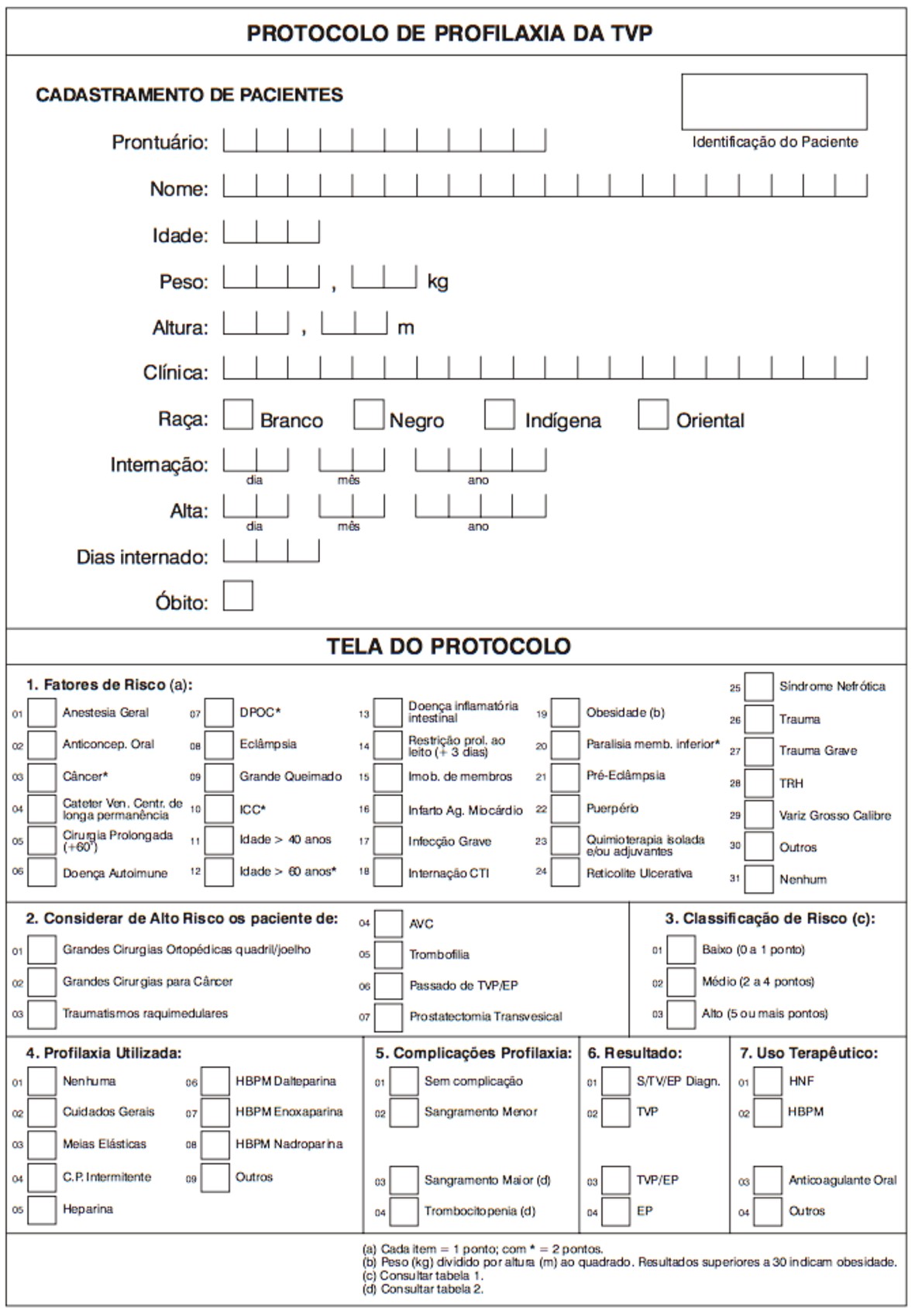
The 2005 VTE prophylaxis guidelines published by the Brazilian Society of Angiology and Vascular Surgery (SBACV) were used to determine risk and prophylaxis indications ( Figure 1 ). Data were collected by the researchers and tabulated in an Excel® spreadsheet in a standardized manner for later statistical analysis.
Brazilian Society of Angiology and Vascular Surgery deep venous thrombosis prophylaxis protocol (in Portuguese).
Patients were separated into two major groups (clinical and surgical) and then subdivided according to SBAVC VTE risk strata into low and high risk clinical patients and low, moderate, and high risk surgical patients risk. 1717 Sociedade Brasileira de Angiologia e de Cirurgia Vascular – SBACV. Normas de orientação clínica para a prevenção, o diagnóstico e o tratamento da trombose venosa profunda. J Vasc Bras. 2005;2005:S185-94. Results were then analyzed to determine the relationship between risk classification and prophylaxis prescribed, defining prophylaxis as appropriate only if it complied with the criteria set out in the SBACV VTE guidelines. Data and results were double-checked by the researchers.
Only mechanical prophylaxis measures that could be selected on the hospital’s MV-PEP® system were defined as correct, as follows: instruct/encourage early mobilization and motor physiotherapy. Other methods of mechanical prophylaxis, such as graduated compression elastic stockings and/or intermittent pneumatic compression devices were not available to the healthcare team. Along the same lines, the only pharmaceutical prophylaxis measures considered appropriate were those set out in the SBACV guidelines and available on the hospital’s MV-PEP® system: 20 mg enoxaparin once a day, 40 mg enoxaparin once a day, 5,000 international units (IU) of unfractionated heparin every 8 hours or every 12 hours, and 2.5 mg fondaparinux once a day. Dalteparin and nadroparin, which are also recommended by the SBACV, were not available at this hospital.
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS®), using the chi-square test for categorical variables and Student’s t test to compare the means of continuous variables, with statistical help provided by the institution’s research support office.
RESULTS
Eligibility and demographics
Electronic patient records were analyzed for 500 patients selected at random, 456 (100%) of whom met the inclusion criteria. The sample was divided into two categories: A) clinical patients (n = 136, 29.8%) and B) surgical patients (n = 320, 70.2%), on the basis of the protocols for risk and prophylaxis indications produced by the SBACV. The 44 patients were excluded from the sample for the following reasons: eight had indications for vena cava filters, 16 were pregnant women, and 20 were on full anticoagulation ( Figure 2 ).
The patients analyzed were hospitalized for a variety of reasons and for periods judged necessary by the healthcare team, which was responsible for choosing VTE prophylaxis prescriptions.
Male patients predominated in both the clinical (52.6% men vs. 47.4% women) and the surgical groups (60.6% men vs. 39.4% women). The clinical group had higher mean age than the surgical group by 7.4 years (62.4 vs. 55.0 years, respectively) and its mean length of hospital stay was 1.5 days longer than in the surgical patient group (6.1 days vs. 4.6 days). Table 1 illustrates the demographic profile of the patients.
Risk factors
In common with the demographic profile, risk factors were different in the two both groups. There were more risk factors related to chronic diseases (cancer, chronic obstructive pulmonary disease, congestive heart failure, acute myocardial infarction, bed confinement, and prior history of VTE) and chemotherapy medication in the clinical group, whereas factors predisposing to VTE in the surgical group were related to the surgical intervention itself (trauma, tissue wounds, general anesthesia, and postoperative immobilization) ( Table 1 ).
Overall outcomes (clinical and surgical patients)
The overall rate of appropriate VTE prophylaxis prescriptions was 42.1%, vs. 57.9% inappropriate VTE prophylaxis, for the whole sample of 456 patients analyzed ( Table 2 ).
Analysis of the 57.9% (264 patients) with inappropriate VTE prophylaxis revealed that 36.6% (167 patients) met criteria for pharmaceutical prophylaxis, but were not given it; 14.4% (66 patients) were given it, but at the wrong dosage; 1.9% (nine patients) were given it but with incorrect dose intervals; and 4.8% (22 patients) were given medication despite not meeting criteria for pharmaceutical prophylaxis ( Table 3 and Figure 3 ).
Stratified analysis of types of inappropriate prophylaxis for all patients with inappropriate prophylaxis (p < 0.05).
Flow diagram showing inclusions and exclusions, appropriate prophylaxis, and inappropriate prophylaxis with subtypes for all patients.
Outcomes in the clinical group
Analysis of the 136 (100%) clinical patients in isolation revealed that 72 (52.9%) of them were given pharmaceutical prophylaxis correctly, in conformity with the SBACV guidelines, while 64 (47.1%) patients had pharmaceutical prophylaxis managed incorrectly ( Table 4 ).
The SBACV classifies clinical patients into two groups, those at increased risk, who should be given pharmaceutical prophylaxis, and those at lower risk, who should not be given prophylactic medications and should be treated with mechanical prophylaxis only. The clinical patients were therefore classified according to the SBACV guidelines and analyzed separately for correct or incorrect pharmaceutical prophylaxis.
There were a total of 112 clinical patients at increased risk, among whom prophylaxis was prescribed correctly (i.e., pharmaceutical prophylaxis was given) for 60 (44.1% of the clinical patients) and incorrectly for the remainder (38.2% of the clinical patients) ( Table 5 ).
Analysis of clinical patients stratified by need for prophylaxis and appropriate or inappropriate prophylaxis (p < 0.05).
Analyzing just those clinical patients for whom pharmaceutical prophylaxis was managed incorrectly (64 patients) we observed that 28 (20.5% of the clinical patients) patients were not given medication despite meeting the criteria, whereas the other 36 (26.4% of the clinical patients) patients were prescribed pharmaceutical prophylaxis, but not in accordance with the SBACV protocol, because dosages or frequency were incorrect, or were given medication when they did not meet criteria for pharmaceutical prophylaxis ( Table 6 and Figure 4 ).
Stratified analysis of types of inappropriate prophylaxis for clinical patients with inappropriate prophylaxis (p < 0.05).
Flow diagram showing inclusions and exclusions, appropriate prophylaxis, and inappropriate prophylaxis with subtypes for clinical patients.
Outcomes in the surgical group
Analysis of the group of surgical patients, comprising 320 (100%) individuals, found a 37.5% (120 patients) rate of appropriate prophylaxis and a 62.5% (200 patients) rate of noncompliance with the SBACV guidelines ( Table 7 ).
The SBACV guidelines have three categories for surgical patients: low, moderate, and high risk, each of which has its own appropriate measures for pharmaceutical prophylaxis.
It was observed that 37.5% of surgical patients were given the appropriate prophylaxis, distributed by risk category as follows: 14.4% were at low risk of DVT/PTE, 5.3% were at moderate risk, and 17.8% were at high risk ( Table 8 ).
Analysis of surgical patients stratified by risk classification and appropriate or inappropriate VTE prophylaxis (p < 0.05).
Of the 200 patients put on a prophylactic regime different from that recommended by SBACV guidelines, 139 (43.4%) patients were not given pharmaceutical prophylaxis even though they met criteria for medication, while 61 (19.0%) patients were given pharmaceutical prophylaxis, but with incorrect dosage or posology, or were given medication despite not meeting criteria for pharmaceutical prophylaxis ( Table 9 and Figure 5 ).
Stratified analysis of types of inappropriate prophylaxis among surgical patients with inappropriate prophylaxis (p < 0.05).
Flow diagram showing inclusions and exclusions, appropriate prophylaxis, and inappropriate prophylaxis with subtypes for surgical patients.
DISCUSSION
The data collected reiterate the epidemiological profile described in the literature on patients at increased risk of VTE, since we found that patients had multiple comorbidities, age greater than 60 years, and mean length of hospital stay in the range 4.6 to 6.1 days. Surgical patients appear to be at greater risk, because of factors directly related to their surgical procedures.
Considering clinical and surgical patients together, the rate of appropriate prophylaxis (42.1%) was similar to a multicenter Brazilian study conducted in 2006 at five hospitals in the state of São Paulo, which reported a 42.7% overall rate of compliance with the prophylaxis protocol. 88 Deheinzelin D, Braga A, Martins L, et al. Incorrect use of thromboprophylaxis for venous thromboembolism in medical and surgical patients: results of a multicentric, observational and cross‐sectional study in Brazil. J Thromb Haemost. 2006;4(6):1266-70. http://dx.doi.org/10.1111/j.1538-7836.2006.01981.x.
http://dx.doi.org/10.1111/j.1538-7836.2...
Analyzing the outcome separately for clinical patients, prophylaxis was administered correctly in just 52.9% of cases, and even lower values were observed for surgical patients (37.5% of cases), reflecting rates slightly lower than found in the bibliographic review. 88 Deheinzelin D, Braga A, Martins L, et al. Incorrect use of thromboprophylaxis for venous thromboembolism in medical and surgical patients: results of a multicentric, observational and cross‐sectional study in Brazil. J Thromb Haemost. 2006;4(6):1266-70. http://dx.doi.org/10.1111/j.1538-7836.2006.01981.x.
http://dx.doi.org/10.1111/j.1538-7836.2...
,1111 Cohen AT, Tapson VF, Bergmann JF, et al. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet. 2008;371(9610):387-94. http://dx.doi.org/10.1016/S0140-6736(08)60202-0.
http://dx.doi.org/10.1016/S0140-6736(08...
,1818 Engelhorn ALV, Garcia ACF, Cassou MF, Birckholz L, Engelhorn CA. Profilaxia da trombose venosa profunda-estudo epidemiológico em um hospital escola. J Vasc Bras. 2002;1:97-102. Analysis of data from Brazil collected in large-scale multicenter studies such as ENDORSE revealed rates of appropriate prophylaxis of 59% and 46% for clinical and surgical patients, respectively. The overall rates of appropriate prophylaxis in data from 32 countries were 40.0% for clinical patients and 59.0% for surgical patients, but there were major differences between different countries ( Table 10 ). 1111 Cohen AT, Tapson VF, Bergmann JF, et al. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet. 2008;371(9610):387-94. http://dx.doi.org/10.1016/S0140-6736(08)60202-0.
http://dx.doi.org/10.1016/S0140-6736(08...
Despite the well-known benefits of VTE prophylaxis, the persistently high rates of noncompliance with prophylaxis guidelines are disconcerting. The importance of the data observed emphasize the need to elucidate the reasons why appropriate prophylaxis rates are lower than those reported in the literature. Data were stratified with the objective of revealing where errors occur. Previous studies have not reported information on the reasons for noncompliance and the data observed in this study suggest that clinical and surgical patients are affected by different problems.
Among the clinical patients, the majority of noncompliance with guidelines was in the form of prescription of incorrect dosage/medication (26.4%), rather than failure to prescribe medication when indicated (20.5%). The opposite was the case with the surgical patients, 43.4% of whom were not given medication even though they met the criteria for it. Several factors may be behind the figures observed.
With relation to dose/medication errors, we observed that the majority of errors were prescription of the dosage recommended for high risk patients to moderate/low risk patients. In contrast, failure to prescribe pharmaceutical prophylaxis, which was most common among surgical patients, may be because of more than one reason: the cross-sectional nature of the study takes a snapshot at the time of prescription assessed (patients in the preoperative or immediate postoperative period may not yet have been medicated, in this case, correctly); surgeons may have been cautious with regard to risk of bleeding; the monthly rotation of the residents who work in the wards may be involved; risk stratification may have been incorrect; or the VTE prophylaxis protocol may not have been used or may not have been known about. A previous study conducted in Brazil with 105 physicians, surgeons, and clinicians attempted to define where VTE prophylaxis errors were being committed, administering a questionnaire on the subject to prescribers. It observed that 100% of the physicians knew the risk factors and the methods of VTE prophylaxis and that 92.3% of them knew how to use prophylaxis correctly. 1919 Garcia ACF, Souza BVD, Volpato DE, et al. Realidade do uso da profilaxia para trombose venosa profunda: da teoria à prática. J Vasc Bras. 2005;4:35-41. ,2020 Pereira CA, Brito SSD, Martins AS, Almeida CM. Profilaxia da trombose venosa profunda: aplicação prática e conhecimento teórico em um hospital geral. J Vasc Bras. 2008;7(1):18-27. http://dx.doi.org/10.1590/S1677-54492008000100005.
http://dx.doi.org/10.1590/S1677-5449200...
Knowing that the care teams in the clinical/surgical wards are made up of residents who have passed rigorous examinations to be selected for residency programs and of specialist treating physicians, we do not think that ignorance of the protocol is the most plausible hypothesis for the low rates of appropriate prophylaxis.
Especially high rates of noncompliance with guidelines were observed for moderate risk surgical patients (40.9%), who were classified erroneously by prescribers who did not adhere to the SBACV guidelines. Many errors of non-prescription of prophylaxis originate from failure to perceive the magnitude of the problem and from individual experiences not founded in management of the subject. 2121 Geerts WH, Heit JA, Clagett GP, et al. Prevention of venous thromboembolism. Chest. 2001;119(1, Suppl):132S-75S. http://dx.doi.org/10.1378/chest.119.1_suppl.132S.
http://dx.doi.org/10.1378/chest.119.1_s...
,2222 House of Commons Health Committee. The prevention of venous thromboembolism in hospitalised patients. Second report of session 2005. London: The Stationery OYce Limited; 2005. Ordered by The House of Commons to be printed 23 February 2005. Other services also commit prophylaxis errors and these could be corrected by maintaining ongoing education of prescribers and standardizing prescription according to risk protocols. The results of these interventions could raise appropriate prophylaxis rates from 43% to 71%. 33 Stinnett JM, Pendleton R, Skordos L, Wheeler M, Rodgers GM. Venous thromboembolism prophylaxis in medically ill patients and the development of strategies to improve prophylaxis rates. Am J Hematol. 2005;78(3):167-72. http://dx.doi.org/10.1002/ajh.20281.
http://dx.doi.org/10.1002/ajh.20281 ...
Applications for smartphones and tablets, such as Caprini DVT Risk® and Thromboembolism Risk®, among others, facilitate risk stratification of patients in hospital and can be used free-of-charge, rapidly, and safely at the bedside. The medical residency programs at the institution studied include weekly lessons covering their respective specialties and subjects such as VTE prophylaxis and treatment should be emphasized in all disciplines that involve care for inpatients. Similar subjects could be dealt with for non-physician healthcare teams as part of programs for specialization and improvement.
Difficulties with and limitations restricting the medical record and prescription software used at the hospital became clear during analysis of the data. Currently, the prescription system warns the prescriber to make sure that the prophylactic medication really is indicated for patients when it is added to the prescription list. However, the system should work in the opposite manner, warning the physician to check whether the patient should be being prescribed pharmaceutical prophylaxis when this is not the case, or whether the prophylactic dose is correct for the patient’s risk class. The system could also contribute by alerting the physician if a patient has been admitted with cancer, pelvic fractures, or thrombophilias or to a stroke unit. The hospital studied does not have other types of heparin available for pharmaceutical prophylaxis or pneumatic boots for use on the wards, but use of specific elastic stockings and other types of low cost mechanical prophylaxis could easily be added, increasing prescription options.
The relevance of this study lies in the enormous social and economic cost that complications secondary to prophylaxis errors can cause. Venous thromboembolism is a silent and dangerous disease that is inherent to a large proportion of patients admitted to tertiary hospitals, but which is not always remembered by all treating physicians. 2222 House of Commons Health Committee. The prevention of venous thromboembolism in hospitalised patients. Second report of session 2005. London: The Stationery OYce Limited; 2005. Ordered by The House of Commons to be printed 23 February 2005.
When appropriately administered, VTE prophylaxis reduces morbidity and mortality and the cost of complications, admissions, and medications in all administrative areas, directly benefiting patients and the healthcare system. 1818 Engelhorn ALV, Garcia ACF, Cassou MF, Birckholz L, Engelhorn CA. Profilaxia da trombose venosa profunda-estudo epidemiológico em um hospital escola. J Vasc Bras. 2002;1:97-102.
CONCLUSIONS
At the University Hospital studied, the risk of VTE among inpatients was similar to rates reported in the literature. Prescriptions of VTE prophylaxis were correct in 42.1% of the patients in the entire sample and, when stratified, 52.9% of clinical patients and 37.5% of surgical patients received the correct VTE prophylaxis. The most common error causing incorrect prescription was failure to classify patient VTE risk. To reduce this problem, ongoing education is recommended for prescribers and non-prescribers, encouraging use of instruments for risk stratification and prescription compatible with risk levels, in addition to changes to the software used for medical records and electronic prescriptions to include risk assessment and prescription reminders for prevention of VTE.
-
How to cite: Curtarelli A, Silva LPC, Camargo PAB, et al. Venous thromboembolism, can we do better? Profile of venous thromboembolism risk and prophylaxis in a university hospital in the state of São Paulo. J Vasc Bras. 2019;18: e20180040. https://doi.org/10.1590/1677-5449.004018
-
Financial support: None.
-
The study was carried out at Hospital das Clínicas (HC), Faculdade de Medicina de Botucatu (FMB), Universidade Estadual “Júlio de Mesquita Filho” (UNESP), Botucatu, SP, Brazil.
REFERÊNCIAS
-
1Guyatt GH, Eikelboom JW, Gould MK, et al. Approach to outcome measurement in the prevention of thrombosis in surgical and medical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e185S-94S. http://dx.doi.org/10.1378/chest.11-2289.
» http://dx.doi.org/10.1378/chest.11-2289 -
2Caprini JA, Arcelus JI, Reyna JJ. Effective risk stratification of surgical and nonsurgical patients for venous thromboembolic disease. Semin Hematol. 2001;38:12-9. http://dx.doi.org/10.1016/S0037-1963(01)90094-0.
» http://dx.doi.org/10.1016/S0037-1963(01)90094-0 -
3Stinnett JM, Pendleton R, Skordos L, Wheeler M, Rodgers GM. Venous thromboembolism prophylaxis in medically ill patients and the development of strategies to improve prophylaxis rates. Am J Hematol. 2005;78(3):167-72. http://dx.doi.org/10.1002/ajh.20281.
» http://dx.doi.org/10.1002/ajh.20281 -
4Jacobson BF, Louw S, Buller H, et al. Venous thromboembolism: prophylactic and therapeutic practice guideline. S Afr Med J. 2013;103(4):261-7. http://dx.doi.org/10.7196/SAMJ.6706.
» http://dx.doi.org/10.7196/SAMJ.6706 -
5Caiafa JS, Bastos MD. Programa de profilaxia do tromboembolismo venoso do Hospital Naval Marcílio Dias: um modelo de educação continuada. J Vasc Bras. 2002;1:103-12.
-
6Engelhorn CA, Nardelli J, Iwamura AP, Salgado LD, Hartmann MO, Witt NC. Drug prophylaxis of deep vein thrombosis in patients submitted to trauma surgery in a university hospital. J Vasc Bras. 2012;11(2):97-101. http://dx.doi.org/10.1590/S1677-54492012000200005.
» http://dx.doi.org/10.1590/S1677-54492012000200005 -
7Goldhaber SZ. DVT prevention: what is happening in the “real world”? Semin Thromb Hemost. 2003;29(Suppl 1):23-31. http://dx.doi.org/10.1055/s-2003-45414.
» http://dx.doi.org/10.1055/s-2003-45414 -
8Deheinzelin D, Braga A, Martins L, et al. Incorrect use of thromboprophylaxis for venous thromboembolism in medical and surgical patients: results of a multicentric, observational and cross‐sectional study in Brazil. J Thromb Haemost. 2006;4(6):1266-70. http://dx.doi.org/10.1111/j.1538-7836.2006.01981.x.
» http://dx.doi.org/10.1111/j.1538-7836.2006.01981.x -
9Carneiro JLDA, Targueta GP, Marino LO. Avaliação da profilaxia do tromboembolismo venoso em hospital de grande porte; Evaluation of venous thromboembolism prophylaxis in a high complexity hospital. Rev Col Bras Cir. 2010;37(3):204-10. http://dx.doi.org/10.1590/S0100-69912010000300008.
» http://dx.doi.org/10.1590/S0100-69912010000300008 -
10Marchi C, Schlup IB, Lima CAD, Schlup HA. Avaliação da profilaxia da trombose venosa profunda em um hospital geral. J Vasc Bras. 2005;4:171-5.
-
11Cohen AT, Tapson VF, Bergmann JF, et al. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet. 2008;371(9610):387-94. http://dx.doi.org/10.1016/S0140-6736(08)60202-0.
» http://dx.doi.org/10.1016/S0140-6736(08)60202-0 -
12Carandina RF. Revisão sistemática e metanálise do perfil de risco e profilaxia de tromboembolismo venoso no Brasil e no mundo. J Vasc Bras. 2016;15:339-40.
-
13Argenta C, Beltrami L. Análise de custo-minimização do uso de heparina não-fracionada e enoxaparina em uma coorte de pacientes em tratamento de tromboembolismo venoso [dissertação]. Porto Alegre: Universidade Federal do Rio Grande do Sul; 2007 [citado 2018 out 16]. http://www.lume.ufrgs.br/handle/10183/11453
» http://www.lume.ufrgs.br/handle/10183/11453 -
14Spyropoulos AC, Hurley JS, Ciesla GN, Lissovoy G. Management of acute proximal deep vein thrombosis: pharmacoeconomic evaluation of outpatient treatment with enoxaparin vs inpatient treatment with unfractionated heparin. Chest. 2002;122(1):108-14. http://dx.doi.org/10.1378/chest.122.1.108.
» http://dx.doi.org/10.1378/chest.122.1.108 -
15Edo A, Fa B, Melo DSÂ, Alves da Costa TD, Fernandes MC, Fernandes MC. Fatores de risco e profilaxia para tromboembolismo venoso em hospitais da cidade de Manaus. J Bras Pneumol. 2009;35(2):114-121.
-
16Rocha ATC, Paiva EFD, Araújo DMD, et al. Impacto de um programa para profilaxia de tromboembolismo venoso em pacientes clínicos em quatro hospitais de Salvador. Rev Assoc Med Bras. 2010;56(2):197-203. http://dx.doi.org/10.1590/S0104-42302010000200019.
» http://dx.doi.org/10.1590/S0104-42302010000200019 -
17Sociedade Brasileira de Angiologia e de Cirurgia Vascular – SBACV. Normas de orientação clínica para a prevenção, o diagnóstico e o tratamento da trombose venosa profunda. J Vasc Bras. 2005;2005:S185-94.
-
18Engelhorn ALV, Garcia ACF, Cassou MF, Birckholz L, Engelhorn CA. Profilaxia da trombose venosa profunda-estudo epidemiológico em um hospital escola. J Vasc Bras. 2002;1:97-102.
-
19Garcia ACF, Souza BVD, Volpato DE, et al. Realidade do uso da profilaxia para trombose venosa profunda: da teoria à prática. J Vasc Bras. 2005;4:35-41.
-
20Pereira CA, Brito SSD, Martins AS, Almeida CM. Profilaxia da trombose venosa profunda: aplicação prática e conhecimento teórico em um hospital geral. J Vasc Bras. 2008;7(1):18-27. http://dx.doi.org/10.1590/S1677-54492008000100005.
» http://dx.doi.org/10.1590/S1677-54492008000100005 -
21Geerts WH, Heit JA, Clagett GP, et al. Prevention of venous thromboembolism. Chest. 2001;119(1, Suppl):132S-75S. http://dx.doi.org/10.1378/chest.119.1_suppl.132S.
» http://dx.doi.org/10.1378/chest.119.1_suppl.132S -
22House of Commons Health Committee. The prevention of venous thromboembolism in hospitalised patients. Second report of session 2005. London: The Stationery OYce Limited; 2005. Ordered by The House of Commons to be printed 23 February 2005.
Publication Dates
-
Publication in this collection
11 Mar 2019 -
Date of issue
2019
History
-
Received
01 Aug 2018 -
Accepted
16 Oct 2018