Abstract
Mortality from penetrating traumas involving the subclavian vessels can be as high as 60% in pre-hospital settings. Operating room mortality is in the range of 5-30%. This paper presents a case in which a strategy for damage control was employed for a patient with an injury to the origin of the left subclavian artery, using subclavian ligation, with no need for any other intervention, and maintaining viability of the left upper limb via collateral circulation. The authors also review surgical approaches and treatment strategies with a focus on damage control in subclavian vessel injuries.
Keywords:
chest traumas; subclavian artery; subclavian steal syndrome; vascular system injuries
Resumo
Os traumas penetrantes de vasos subclávios atingem mortalidade de até 60% em um cenário pré-hospitalar. A mortalidade no intraoperatório varia de 5-30%. Apresenta-se um caso de estratégia de controle de danos para um paciente com lesão na origem da artéria subclávia esquerda, através de ligadura, sem necessidade de outra intervenção, mantendo a viabilidade do membro superior esquerdo por meio de circulação colateral. Os autores fazem uma revisão sobre vias de acesso e estratégias de tratamento com ênfase em controle de danos para lesões de vasos subclávios.
Palavras-chave:
traumatismos torácicos; artéria subclávia; síndrome do roubo subclávio; lesão do sistema vascular
INTRODUCTION
Mortality from penetrating traumas involving subclavian vessels can reach 60% in prehospital settings, making speedy transportation to a trauma center a decisive factor. Intraoperative mortality is in the range of 5-30%.11 Carlos SF, Góis CC, Machado GF, et al. Traumatismo penetrante dos vasos subclávios: revisão da literatura a propósito de um caso clínico. Rev Port Cir. 2015;32:35-41.
2 Kou HW, Liao CH, Huang JF, et al. Eighteen years’ experience of traumatic subclavian vascular injury in a tertiary referral trauma center. Eur J Trauma Emerg Surg. 2018;45(6):973-978. PMid:30627733.
3 Waller CJ, Cogbill TH, Kallies KJ, et al. Contemporary management of subclavian and axillary artery Injuries: A Western Trauma Association multicenter review. J Trauma Acute Care Surg. 2017;83(6):1023-31. http://dx.doi.org/10.1097/TA.0000000000001645. PMid:28715360.
http://dx.doi.org/10.1097/TA.00000000000...
-44 Maués Filho J, Hauter H. Tratamento endovascular de fístula traumática de vasos subclávios: relato de caso. J Vasc Bras. 2018;17(3):248-51. http://dx.doi.org/10.1590/1677-5449.010317.
http://dx.doi.org/10.1590/1677-5449.0103...
The proximity of neurovascular structures, hematoma, anatomic abnormalities and the need for adequate exposure make surgery to treat such traumas challenging.33 Waller CJ, Cogbill TH, Kallies KJ, et al. Contemporary management of subclavian and axillary artery Injuries: A Western Trauma Association multicenter review. J Trauma Acute Care Surg. 2017;83(6):1023-31. http://dx.doi.org/10.1097/TA.0000000000001645. PMid:28715360.
http://dx.doi.org/10.1097/TA.00000000000...
4 Maués Filho J, Hauter H. Tratamento endovascular de fístula traumática de vasos subclávios: relato de caso. J Vasc Bras. 2018;17(3):248-51. http://dx.doi.org/10.1590/1677-5449.010317.
http://dx.doi.org/10.1590/1677-5449.0103...
-55 Elkbuli A, Shaikh S, McKenney M, Boneva D. Subclavian artery avulsion following blunt trauma: A case report and literature review. Int J Surg Case Rep. 2019;61:157-60. http://dx.doi.org/10.1016/j.ijscr.2019.07.061. PMid:31376736.
http://dx.doi.org/10.1016/j.ijscr.2019.0...
Postoperative mortality varies from 5 to 40%,22 Kou HW, Liao CH, Huang JF, et al. Eighteen years’ experience of traumatic subclavian vascular injury in a tertiary referral trauma center. Eur J Trauma Emerg Surg. 2018;45(6):973-978. PMid:30627733.,33 Waller CJ, Cogbill TH, Kallies KJ, et al. Contemporary management of subclavian and axillary artery Injuries: A Western Trauma Association multicenter review. J Trauma Acute Care Surg. 2017;83(6):1023-31. http://dx.doi.org/10.1097/TA.0000000000001645. PMid:28715360.
http://dx.doi.org/10.1097/TA.00000000000...
and postoperative complications affect 24%.44 Maués Filho J, Hauter H. Tratamento endovascular de fístula traumática de vasos subclávios: relato de caso. J Vasc Bras. 2018;17(3):248-51. http://dx.doi.org/10.1590/1677-5449.010317.
http://dx.doi.org/10.1590/1677-5449.0103...
The correct surgical approach is of paramount importance. An incision over the clavicle, extended to the deltopectoral groove, may be sufficient for more distal injuries, but injuries to the intrathoracic segment demand a thoracotomy.11 Carlos SF, Góis CC, Machado GF, et al. Traumatismo penetrante dos vasos subclávios: revisão da literatura a propósito de um caso clínico. Rev Port Cir. 2015;32:35-41.
Right-side injuries can be approached via a median sternotomy, with anterior cervical and/or right supraclavicular extension if necessary. Left-side injuries are better explored via an anterolateral thoracotomy between the third and fifth intercostal spaces, which can be expanded with a median sternotomy and, if necessary, extended with a supraclavicular incision (open book/trapdoor access).11 Carlos SF, Góis CC, Machado GF, et al. Traumatismo penetrante dos vasos subclávios: revisão da literatura a propósito de um caso clínico. Rev Port Cir. 2015;32:35-41.,33 Waller CJ, Cogbill TH, Kallies KJ, et al. Contemporary management of subclavian and axillary artery Injuries: A Western Trauma Association multicenter review. J Trauma Acute Care Surg. 2017;83(6):1023-31. http://dx.doi.org/10.1097/TA.0000000000001645. PMid:28715360.
http://dx.doi.org/10.1097/TA.00000000000...
,55 Elkbuli A, Shaikh S, McKenney M, Boneva D. Subclavian artery avulsion following blunt trauma: A case report and literature review. Int J Surg Case Rep. 2019;61:157-60. http://dx.doi.org/10.1016/j.ijscr.2019.07.061. PMid:31376736.
http://dx.doi.org/10.1016/j.ijscr.2019.0...
Arterial injuries can be corrected with sutures, end-to-end anastomosis or grafting (autologous or prosthetic).11 Carlos SF, Góis CC, Machado GF, et al. Traumatismo penetrante dos vasos subclávios: revisão da literatura a propósito de um caso clínico. Rev Port Cir. 2015;32:35-41.,55 Elkbuli A, Shaikh S, McKenney M, Boneva D. Subclavian artery avulsion following blunt trauma: A case report and literature review. Int J Surg Case Rep. 2019;61:157-60. http://dx.doi.org/10.1016/j.ijscr.2019.07.061. PMid:31376736.
http://dx.doi.org/10.1016/j.ijscr.2019.0...
,66 Rotondo M, Bard M. Damage control surgery for thoracic injuries. Injury. Int. J. Care Injured. 2004;34(7):649-54. http://dx.doi.org/10.1016/j.injury.2004.03.002.
http://dx.doi.org/10.1016/j.injury.2004....
In serious cases, a temporary intravascular shunt can be used for damage control until stabilization is achieved66 Rotondo M, Bard M. Damage control surgery for thoracic injuries. Injury. Int. J. Care Injured. 2004;34(7):649-54. http://dx.doi.org/10.1016/j.injury.2004.03.002.
http://dx.doi.org/10.1016/j.injury.2004....
,77 Inaba K, Aksoy H, Seamon M, et al. Multicenter evaluation of temporary intravascular shunt use in vascular trauma. J Trauma Acute Care Surg. 2015;80(3):359-63. http://dx.doi.org/10.1097/TA.0000000000000949. PMid:26713968.
http://dx.doi.org/10.1097/TA.00000000000...
and, in extreme cases, the subclavian artery can be ligated with little risk of ischemia.66 Rotondo M, Bard M. Damage control surgery for thoracic injuries. Injury. Int. J. Care Injured. 2004;34(7):649-54. http://dx.doi.org/10.1016/j.injury.2004.03.002.
http://dx.doi.org/10.1016/j.injury.2004....
,88 Cheema M, Kirton O, Lukose B, Gallagher J. Ligation of the Subclavian Artery After Blunt Trauma Presenting as Massive Hemothorax. J Trauma. 2008;64(4):1126-30. http://dx.doi.org/10.1097/01.ta.0000195726.14064.0f. PMid:17413525.
http://dx.doi.org/10.1097/01.ta.00001957...
,99 Ferreira M, Souza A. Síndrome do roubo da subclávia: um relato de caso. Rev Med Saude Brasilia. 2017;6(2):220-7.
This article describes a damage control strategy employed in a patient with an injury to the origin of the left subclavian artery.
Part I – Clinical situation
The case described is of a 24-year-old male patient, victim of a gunshot wound to the left infraclavicular region at the parasternal line. He arrived at the hospital with patent airways, an asymmetrical thorax, thoracic wound with air leak, absent vesicular murmur in the left hemithorax, heart rate (HR) of 135 bpm, sweating profusely, with cold skin, and blood pressure (BP) of 80 x 50 mm Hg. Pleural drainage revealed a large volume hemothorax (1,400 mL).
After initial treatment, BP of 110 x 80 mm Hg and HR of 122 bpm were achieved, but the patient developed respiratory distress and his level of consciousness reduced. He was subjected to oral endotracheal intubation and transferred to the operating room for thoracotomy.
Part II – What was done
A left anterolateral thoracotomy was performed at the fifth intercostal space. After removal of a large clot from the pleural cavity, a through-and-through wound was identified in the superior pulmonary lobe (without active bleeding) and a large hematoma involving the upper mediastinum, which could not be explored because of the operating field obtained. The decision was taken to expand the access with a transverse sternotomy and extension to a right anterolateral thoracotomy from the fifth intercostal space to the parasternal line.
Proximal control of the supra-aortic trunks was obtained by performing a longitudinal pericardiotomy, before manipulating the hematoma. During this phase of surgery, intense bleeding from the injury started spontaneously. This was partially controlled by “en masse” application of a Satinsky clamp to the structures adjacent to the source of bleeding.
At this point, the patient suffered cardiac arrest with ventricular fibrillation, and resuscitation maneuvers were initiated, including descending aorta cross-clamping, internal cardiac compressions and defibrillation and intravenous adrenaline. Sinusoidal rhythm was reestablished after 4 minutes.
Dissection was resumed and a partial avulsion of the left subclavian artery close to its origin was identified. In view of the severity of the patient’s condition, the decision was taken to ligate the artery. Hemostasis was reviewed and bilateral thoracic drains were installed, followed by closure. The patient was transferred to the intensive care unit (ICU) in a critical state, on vasoactive drugs. He spent 20 days in the ICU and was discharged from hospital on the 35th day after the operation.
The patient has been in outpatients follow-up for 10 months; is free from neurological sequelae associated with the cardiac arrest, and left arm function has recovered well, with systolic blood pressure at 80% of the value measured in the contralateral limb and a palpable radial pulse, although with reduced amplitude (Figure 1). Angiotomography conducted 3 months after surgery showed that vascularization of the left upper limb is via retrograde filling of the left vertebral artery (Figure 2).
Photographs taken 3 months after surgery, showing functional recovery of the left upper limb. The arrow indicates the site of the gunshot wound.
Angiotomography conducted 3 months after surgery. The reconstructions in 1.A, 1.B, and 1.C, show: A: aorta; *left vertebral artery; arrows indicate the left subclavian artery ligated at the origin and the point at which it becomes opaque again.
DISCUSSION
Vascular injuries in the cervico-thoracic outlet are rare and up 90% of cases are caused by penetrating injuries; 2 to 4% of these have subclavian vessels involvement.11 Carlos SF, Góis CC, Machado GF, et al. Traumatismo penetrante dos vasos subclávios: revisão da literatura a propósito de um caso clínico. Rev Port Cir. 2015;32:35-41.,44 Maués Filho J, Hauter H. Tratamento endovascular de fístula traumática de vasos subclávios: relato de caso. J Vasc Bras. 2018;17(3):248-51. http://dx.doi.org/10.1590/1677-5449.010317.
http://dx.doi.org/10.1590/1677-5449.0103...
,1010 Ostovan M, Kojuri J, Dehghani P. Endovascular Repair of the Traumatic Dissection of the Subclavian–Axillary Artery: Report of Four Cases. J Teh Univ Heart Ctr. 2017;12(2):88-91. PMid:28828025.
In stable patients, surgical access can be planned taking into consideration the results of imaging exams such as angiotomography and, occasionally, angiography and Doppler ultrasonography. However, patients whose physiological parameters are in decline should undergo surgery immediately, choosing the approach on the basis of the mechanism of trauma.11 Carlos SF, Góis CC, Machado GF, et al. Traumatismo penetrante dos vasos subclávios: revisão da literatura a propósito de um caso clínico. Rev Port Cir. 2015;32:35-41.
2 Kou HW, Liao CH, Huang JF, et al. Eighteen years’ experience of traumatic subclavian vascular injury in a tertiary referral trauma center. Eur J Trauma Emerg Surg. 2018;45(6):973-978. PMid:30627733.-33 Waller CJ, Cogbill TH, Kallies KJ, et al. Contemporary management of subclavian and axillary artery Injuries: A Western Trauma Association multicenter review. J Trauma Acute Care Surg. 2017;83(6):1023-31. http://dx.doi.org/10.1097/TA.0000000000001645. PMid:28715360.
http://dx.doi.org/10.1097/TA.00000000000...
,1111 Potter B, Pinto D. Subclavian Steal Syndrome. Circulation Journal of AHA. 2014;129(22):2320-3. http://dx.doi.org/10.1161/CIRCULATIONAHA.113.006653. PMid:24891625.
http://dx.doi.org/10.1161/CIRCULATIONAHA...
Proximal injuries to the left subclavian artery are classically approached via an anterolateral thoracotomy incision through the third intercostal space, but in this case the wound was within the “cardiac box” and so the possibility of heart injuries had to be considered.1212 Papaiordanou F, Lourenço A, Ribeiro M Jr. Trauma na Zona Perigosa de Ziedler. Emergência Clínica. 2009;04(17):85-91.
Anterolateral thoracotomy through the fifth space is the classic approach for penetrating chest injuries in unstable patients and extension across to the contralateral thoracic cavity provides access to both pleural cavities and the mediastinum.1313 Stranch E, Zarzaur B, Savage SA. Thinking outside the box: Re-evaluating the approach to penetrating cardiac injuries. Eur J Trauma Emerg Surg. 2017;43(5):617-22. http://dx.doi.org/10.1007/s00068-016-0680-7. PMid:27194248.
http://dx.doi.org/10.1007/s00068-016-068...
14 D’Souza RS, Law L. Open Heart Massage. StatPearls. Treasure Island, FL: StatPearls Publishing; 2020. [citado 2019 nov 26]. https://www.ncbi.nlm.nih.gov/books/NBK537230/
https://www.ncbi.nlm.nih.gov/books/NBK53...
-1515 Teixeira P, DuBose J. Surgical management of vascular trauma. Surg Clin North Am. 2017;97(5):1133-55. http://dx.doi.org/10.1016/j.suc.2017.05.001. PMid:28958362.
http://dx.doi.org/10.1016/j.suc.2017.05....
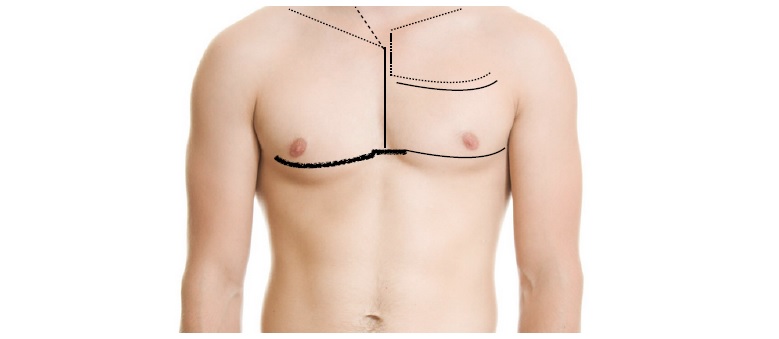
Surgical approaches for traumatic vascular injuries are illustrated in Figure 3.
Approaches for treatment of thoracic vascular injuries. Longitudinal continuous line: median sternotomy, the broken and dotted straight lines indicate possible cervical or right supraclavicular extensions. Solid curved lines indicate left anterolateral thoracotomy incisions over the fifth or third intercostal spaces; the dotted lines on the left hemithorax illustrate extension to a longitudinal sternotomy and supraclavicular incision (open book); while the thicker line indicates extension to a bilateral thoracotomy with transverse sternotomy.
In stable patients, in some cases with a preoperative radiological diagnosis and endovascular resources available, an angioplasty balloon can be inflated in the subclavian artery to achieve proximal vascular control.1616 Branco BC, DuBose JJ. Endovascular solutions for the management of penetrating trauma: an update on REBOA and axillo-subclavian injuries. Eur J Trauma Emerg Surg. 2016;42(6):687-94. http://dx.doi.org/10.1007/s00068-016-0739-5. PMid:27853843.
http://dx.doi.org/10.1007/s00068-016-073...
,1717 Branco B, Boutrous L, DuBose J, et al. Outcome comparison between open and endovascular management of axillosubclavian arterial injuries. J Vasc Surg. 2016;63(3):702-9. http://dx.doi.org/10.1016/j.jvs.2015.08.117. PMid:26506937.
http://dx.doi.org/10.1016/j.jvs.2015.08....
However, in the case described, with near-total avulsion of the left subclavian artery at its origin, any attempt to cross the lesion with a guidewire would have been very unlikely to succeed and there would probably not have been enough space to inflate the balloon proximally to the injury. During surgical exploration, the safest technique for avoiding hemorrhage is to obtain proximal vascular control before dealing with the injury, which was exactly the objective of dissection of the intrapericardial segments of the supra-aortic trunks. Unfortunately, bleeding started while the attempt to achieve proximal control was still underway.
A damage control strategy comprises operating tactics that shorten the duration of surgery, remaining within physiological limits and increasing the patient’s chances of survival.1818 Roberts D, Bobrovitz N, Zygun D, et al. Indications for use of damage control surgery and damage control interventions in civilian trauma patients: A scoping review. J Trauma Acute Care Surg. 2015;78(6):1187-96. http://dx.doi.org/10.1097/TA.0000000000000647. PMid:26151522.
http://dx.doi.org/10.1097/TA.00000000000...
,1919 Engelhardt M, Hinck D. Damage Control bei Gefäßverletzungen. Berlin: Springer Reference Medizin; 2018. p. 1-8. The strategy is generally conducted in three stages: 1) surgical control of life-threatening injuries, achieving hemostasis and preventing contamination of cavities; 2) resuscitation and ICU care, and 3) definitive surgical treatment.1818 Roberts D, Bobrovitz N, Zygun D, et al. Indications for use of damage control surgery and damage control interventions in civilian trauma patients: A scoping review. J Trauma Acute Care Surg. 2015;78(6):1187-96. http://dx.doi.org/10.1097/TA.0000000000000647. PMid:26151522.
http://dx.doi.org/10.1097/TA.00000000000...
,1919 Engelhardt M, Hinck D. Damage Control bei Gefäßverletzungen. Berlin: Springer Reference Medizin; 2018. p. 1-8. In the case described, revascularization was unnecessary because perfusion of the limb was adequate.
Another damage control strategy is to use a vascular shunt, which can be made using a segment of tubular material with a compatible diameter, such as a nasogastric tube,77 Inaba K, Aksoy H, Seamon M, et al. Multicenter evaluation of temporary intravascular shunt use in vascular trauma. J Trauma Acute Care Surg. 2015;80(3):359-63. http://dx.doi.org/10.1097/TA.0000000000000949. PMid:26713968.
http://dx.doi.org/10.1097/TA.00000000000...
,2020 De Ayala-Hillman R, Crespo-Martínez NA, García-Rodríguez O, Ramos-Meléndez EO, Rodriguez-Ortiz P. Traumatic vascular injury and its management with temporary intravascular shunts: A Puerto Rico Trauma Hospital’s Experience. P R Health Sci J. 2018;37(4):220-3. PMid:30548058. providing temporary perfusion of the limb/organ. However, the very small neck at the origin from the aortic arch would have made insertion extremely difficult. In view of the imminent risk of death, ligature of the subclavian artery was chosen, since, when proximal to the origin of the vertebral artery, this rarely provokes decompensated ischemia of the limb.66 Rotondo M, Bard M. Damage control surgery for thoracic injuries. Injury. Int. J. Care Injured. 2004;34(7):649-54. http://dx.doi.org/10.1016/j.injury.2004.03.002.
http://dx.doi.org/10.1016/j.injury.2004....
,88 Cheema M, Kirton O, Lukose B, Gallagher J. Ligation of the Subclavian Artery After Blunt Trauma Presenting as Massive Hemothorax. J Trauma. 2008;64(4):1126-30. http://dx.doi.org/10.1097/01.ta.0000195726.14064.0f. PMid:17413525.
http://dx.doi.org/10.1097/01.ta.00001957...
,99 Ferreira M, Souza A. Síndrome do roubo da subclávia: um relato de caso. Rev Med Saude Brasilia. 2017;6(2):220-7.
A review comparing management of penetrating arterial injuries caused by cervical-thoracic traumas in two distinct periods in the same hospital (modern, 2000-2013, and previous, 1974-1988) concluded that endovascular treatment was only used in the modern period, in stable patients with pseudoaneurysms. Ligature was rarely employed in either period, only used when there was a risk of death, and shunts were only used in the modern period, as an alternative to vessel ligation, when possible.2121 Weinberg JA, Moore A, Magnotti L, et al. Contemporary management of civilian penetrating cervicothoracic arterial injuries. J Trauma Acute Care Surg. 2016;81(2):302-6. http://dx.doi.org/10.1097/TA.0000000000001103. PMid:27192470.
http://dx.doi.org/10.1097/TA.00000000000...
In a different patient sample, of twenty cases of subclavian artery injury, an association with brachial plexus injury was observed in 55% of cases. Additionally, in that study just one patient underwent arterial ligature, and the outcome was death.2222 Lederman A, Paiva F, Saes G, Aun R. Ferimentos da artéria subclávia: Estudo retrospectivo de 20 casos. J Vasc Bras. 2005;4(2):149-54.
Another study, with 38 cases of subclavian/axillary arteries injuries, analyzed types of treatment and outcomes: in 5 cases, ligature of the artery was performed because of the clinical conditions at the time of surgery. There were two deaths, but no signs of ischemia of the limb in the three survivors.2323 Aksoy M, Tunca F, Yanar H, Guloglu R, Ertekin C, Kurtoglu M. Traumatic Injuries to the Subclavian and Axillary Arteries: A 13-Year Review. Surg Today. 2005;35(7):561-5. http://dx.doi.org/10.1007/s00595-005-2990-y. PMid:15976953.
http://dx.doi.org/10.1007/s00595-005-299...
Ligature is reserved for critical cases, when cardiac arrest secondary to hypovolemia may occur in the operating room. If this does occur, thoracotomy resuscitation maneuvers are required, such as clamping the descending aorta, longitudinal pericardiotomy, to enable internal cardiac compressions, at 60-100 bpm, and direct defibrillation, which should be performed with a charge of 10-30 Joules.88 Cheema M, Kirton O, Lukose B, Gallagher J. Ligation of the Subclavian Artery After Blunt Trauma Presenting as Massive Hemothorax. J Trauma. 2008;64(4):1126-30. http://dx.doi.org/10.1097/01.ta.0000195726.14064.0f. PMid:17413525.
http://dx.doi.org/10.1097/01.ta.00001957...
,1414 D’Souza RS, Law L. Open Heart Massage. StatPearls. Treasure Island, FL: StatPearls Publishing; 2020. [citado 2019 nov 26]. https://www.ncbi.nlm.nih.gov/books/NBK537230/
https://www.ncbi.nlm.nih.gov/books/NBK53...
,2424 Wise D, Davies G, Coats T, Lockey D, Hyde J, Good A. Emergency thoracotomy: “how to do it”. Emerg Med J. 2005;22(1):22-4. http://dx.doi.org/10.1136/emj.2003.012963. PMid:15611536.
http://dx.doi.org/10.1136/emj.2003.01296...
,2525 Molnar TF. Thoracic damage control surgery. J Thorac Dis. 2019;11(2, Suppl. 2):S158-66. http://dx.doi.org/10.21037/jtd.2018.11.32. PMid:30906580.
http://dx.doi.org/10.21037/jtd.2018.11.3...
All of these maneuvers were performed in the case described here.
In this case, the absence of limb ischemia is because of subclavian steal syndrome, originally described when there is stenosis in the proximal artery. The syndrome demonstrates a protective effect between the subclavian artery and the vertebrobasilar system.99 Ferreira M, Souza A. Síndrome do roubo da subclávia: um relato de caso. Rev Med Saude Brasilia. 2017;6(2):220-7.,1111 Potter B, Pinto D. Subclavian Steal Syndrome. Circulation Journal of AHA. 2014;129(22):2320-3. http://dx.doi.org/10.1161/CIRCULATIONAHA.113.006653. PMid:24891625.
http://dx.doi.org/10.1161/CIRCULATIONAHA...
In this situation, retrograde blood flow though the vertebral artery occurs if the blood pressure distally to the injury reaches a lower level than the pressure at the basilar artery, via the contralateral vertebral artery and the circle of Willis. This reverse flow through the vertebral artery may be intermittent or continuous, depending on the degree of stenosis, supplying hypoperfused vascular beds.99 Ferreira M, Souza A. Síndrome do roubo da subclávia: um relato de caso. Rev Med Saude Brasilia. 2017;6(2):220-7.,1111 Potter B, Pinto D. Subclavian Steal Syndrome. Circulation Journal of AHA. 2014;129(22):2320-3. http://dx.doi.org/10.1161/CIRCULATIONAHA.113.006653. PMid:24891625.
http://dx.doi.org/10.1161/CIRCULATIONAHA...
Although revascularization of the patient’s arm could be scheduled, the trend is to keep the patient in follow-up and maintain conservative management, since he remains asymptomatic.
Endovascular treatment eliminates risks inherent to surgical dissection. Although the literature reports success rates of up to 95% of cases, the majority are pseudoaneurysm and arteriovenous fistula cases and not acute phase treatments; in such cases, it is recommended that the stent should be deployed without covering the origin of the vertebral artery, thereby reducing the risk of stroke.1616 Branco BC, DuBose JJ. Endovascular solutions for the management of penetrating trauma: an update on REBOA and axillo-subclavian injuries. Eur J Trauma Emerg Surg. 2016;42(6):687-94. http://dx.doi.org/10.1007/s00068-016-0739-5. PMid:27853843.
http://dx.doi.org/10.1007/s00068-016-073...
,1717 Branco B, Boutrous L, DuBose J, et al. Outcome comparison between open and endovascular management of axillosubclavian arterial injuries. J Vasc Surg. 2016;63(3):702-9. http://dx.doi.org/10.1016/j.jvs.2015.08.117. PMid:26506937.
http://dx.doi.org/10.1016/j.jvs.2015.08....
The hemodynamic instability and the anatomic characteristics of the injury already described mean that in such situations, endovascular techniques are not the first option. Moreover, endovascular resources were not available.
Surgeons should be familiar with damage control strategies, which are not only useful in trauma cases, but also when faced with complications during elective surgery. In this context, ligature of the subclavian artery, proximal to the origin of the vertebral artery, is a viable option involving a relatively low risk of insufficient upper limb perfusion.
-
How to cite: Góes Junior AMO, Maurity MP, Amaral CAC. Damage control for subclavian artery injury. J Vasc Bras. 2020;19:e20200007. https://doi.org/10.1590/1677-5449.200007.
-
Financial support: None.
-
The study was carried out at Hospital Metropolitano de Urgência e Emergência, Ananindeua, PA, Brazil.
REFERÊNCIAS
-
1Carlos SF, Góis CC, Machado GF, et al. Traumatismo penetrante dos vasos subclávios: revisão da literatura a propósito de um caso clínico. Rev Port Cir. 2015;32:35-41.
-
2Kou HW, Liao CH, Huang JF, et al. Eighteen years’ experience of traumatic subclavian vascular injury in a tertiary referral trauma center. Eur J Trauma Emerg Surg. 2018;45(6):973-978. PMid:30627733.
-
3Waller CJ, Cogbill TH, Kallies KJ, et al. Contemporary management of subclavian and axillary artery Injuries: A Western Trauma Association multicenter review. J Trauma Acute Care Surg. 2017;83(6):1023-31. http://dx.doi.org/10.1097/TA.0000000000001645 PMid:28715360.
» http://dx.doi.org/10.1097/TA.0000000000001645 -
4Maués Filho J, Hauter H. Tratamento endovascular de fístula traumática de vasos subclávios: relato de caso. J Vasc Bras. 2018;17(3):248-51. http://dx.doi.org/10.1590/1677-5449.010317
» http://dx.doi.org/10.1590/1677-5449.010317 -
5Elkbuli A, Shaikh S, McKenney M, Boneva D. Subclavian artery avulsion following blunt trauma: A case report and literature review. Int J Surg Case Rep. 2019;61:157-60. http://dx.doi.org/10.1016/j.ijscr.2019.07.061 PMid:31376736.
» http://dx.doi.org/10.1016/j.ijscr.2019.07.061 -
6Rotondo M, Bard M. Damage control surgery for thoracic injuries. Injury. Int. J. Care Injured. 2004;34(7):649-54. http://dx.doi.org/10.1016/j.injury.2004.03.002
» http://dx.doi.org/10.1016/j.injury.2004.03.002 -
7Inaba K, Aksoy H, Seamon M, et al. Multicenter evaluation of temporary intravascular shunt use in vascular trauma. J Trauma Acute Care Surg. 2015;80(3):359-63. http://dx.doi.org/10.1097/TA.0000000000000949 PMid:26713968.
» http://dx.doi.org/10.1097/TA.0000000000000949 -
8Cheema M, Kirton O, Lukose B, Gallagher J. Ligation of the Subclavian Artery After Blunt Trauma Presenting as Massive Hemothorax. J Trauma. 2008;64(4):1126-30. http://dx.doi.org/10.1097/01.ta.0000195726.14064.0f PMid:17413525.
» http://dx.doi.org/10.1097/01.ta.0000195726.14064.0f -
9Ferreira M, Souza A. Síndrome do roubo da subclávia: um relato de caso. Rev Med Saude Brasilia. 2017;6(2):220-7.
-
10Ostovan M, Kojuri J, Dehghani P. Endovascular Repair of the Traumatic Dissection of the Subclavian–Axillary Artery: Report of Four Cases. J Teh Univ Heart Ctr. 2017;12(2):88-91. PMid:28828025.
-
11Potter B, Pinto D. Subclavian Steal Syndrome. Circulation Journal of AHA. 2014;129(22):2320-3. http://dx.doi.org/10.1161/CIRCULATIONAHA.113.006653 PMid:24891625.
» http://dx.doi.org/10.1161/CIRCULATIONAHA.113.006653 -
12Papaiordanou F, Lourenço A, Ribeiro M Jr. Trauma na Zona Perigosa de Ziedler. Emergência Clínica. 2009;04(17):85-91.
-
13Stranch E, Zarzaur B, Savage SA. Thinking outside the box: Re-evaluating the approach to penetrating cardiac injuries. Eur J Trauma Emerg Surg. 2017;43(5):617-22. http://dx.doi.org/10.1007/s00068-016-0680-7 PMid:27194248.
» http://dx.doi.org/10.1007/s00068-016-0680-7 -
14D’Souza RS, Law L. Open Heart Massage. StatPearls. Treasure Island, FL: StatPearls Publishing; 2020. [citado 2019 nov 26]. https://www.ncbi.nlm.nih.gov/books/NBK537230/
» https://www.ncbi.nlm.nih.gov/books/NBK537230/ -
15Teixeira P, DuBose J. Surgical management of vascular trauma. Surg Clin North Am. 2017;97(5):1133-55. http://dx.doi.org/10.1016/j.suc.2017.05.001 PMid:28958362.
» http://dx.doi.org/10.1016/j.suc.2017.05.001 -
16Branco BC, DuBose JJ. Endovascular solutions for the management of penetrating trauma: an update on REBOA and axillo-subclavian injuries. Eur J Trauma Emerg Surg. 2016;42(6):687-94. http://dx.doi.org/10.1007/s00068-016-0739-5 PMid:27853843.
» http://dx.doi.org/10.1007/s00068-016-0739-5 -
17Branco B, Boutrous L, DuBose J, et al. Outcome comparison between open and endovascular management of axillosubclavian arterial injuries. J Vasc Surg. 2016;63(3):702-9. http://dx.doi.org/10.1016/j.jvs.2015.08.117 PMid:26506937.
» http://dx.doi.org/10.1016/j.jvs.2015.08.117 -
18Roberts D, Bobrovitz N, Zygun D, et al. Indications for use of damage control surgery and damage control interventions in civilian trauma patients: A scoping review. J Trauma Acute Care Surg. 2015;78(6):1187-96. http://dx.doi.org/10.1097/TA.0000000000000647 PMid:26151522.
» http://dx.doi.org/10.1097/TA.0000000000000647 -
19Engelhardt M, Hinck D. Damage Control bei Gefäßverletzungen. Berlin: Springer Reference Medizin; 2018. p. 1-8.
-
20De Ayala-Hillman R, Crespo-Martínez NA, García-Rodríguez O, Ramos-Meléndez EO, Rodriguez-Ortiz P. Traumatic vascular injury and its management with temporary intravascular shunts: A Puerto Rico Trauma Hospital’s Experience. P R Health Sci J. 2018;37(4):220-3. PMid:30548058.
-
21Weinberg JA, Moore A, Magnotti L, et al. Contemporary management of civilian penetrating cervicothoracic arterial injuries. J Trauma Acute Care Surg. 2016;81(2):302-6. http://dx.doi.org/10.1097/TA.0000000000001103 PMid:27192470.
» http://dx.doi.org/10.1097/TA.0000000000001103 -
22Lederman A, Paiva F, Saes G, Aun R. Ferimentos da artéria subclávia: Estudo retrospectivo de 20 casos. J Vasc Bras. 2005;4(2):149-54.
-
23Aksoy M, Tunca F, Yanar H, Guloglu R, Ertekin C, Kurtoglu M. Traumatic Injuries to the Subclavian and Axillary Arteries: A 13-Year Review. Surg Today. 2005;35(7):561-5. http://dx.doi.org/10.1007/s00595-005-2990-y PMid:15976953.
» http://dx.doi.org/10.1007/s00595-005-2990-y -
24Wise D, Davies G, Coats T, Lockey D, Hyde J, Good A. Emergency thoracotomy: “how to do it”. Emerg Med J. 2005;22(1):22-4. http://dx.doi.org/10.1136/emj.2003.012963 PMid:15611536.
» http://dx.doi.org/10.1136/emj.2003.012963 -
25Molnar TF. Thoracic damage control surgery. J Thorac Dis. 2019;11(2, Suppl. 2):S158-66. http://dx.doi.org/10.21037/jtd.2018.11.32 PMid:30906580.
» http://dx.doi.org/10.21037/jtd.2018.11.32
Publication Dates
-
Publication in this collection
14 Sept 2020 -
Date of issue
2020
History
-
Received
20 Jan 2020 -
Accepted
18 May 2020