Abstract
Introduction:
Chronic kidney disease (CKD) is defined as loss of kidney function, but its progression leads to systemic changes that compromise the quality of life of patients on dialysis. As such, the decline in lung capacity in this population may be one of the factors related to reduced peripheral muscle strength.
Objective:
Assess the relationship between handgrip strength (HGS), pulmonary function and respiratory muscle strength in patients with CKD on hemodialysis.
Method:
Thirty patients with CKD were assessed in terms of anthropometric data, pulmonary function, respiratory muscle strength and HGS.
Results:
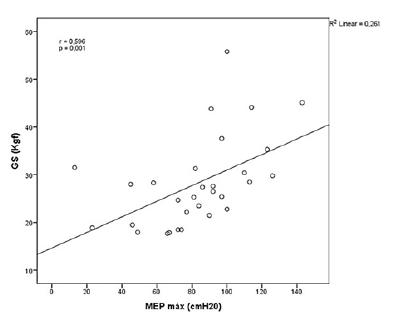
A moderate association was observed between HGS and the variables forced vital capacity (r=0.54; p=0.002), maximum voluntary ventilation (r=0.51; p=0.004) and maximum expiratory pressure (r=0.59; p=0.001), and a weak association with forced expiratory volume in 1 second (FEV1) (r=0.46; p=0.009) and maximum inspiratory pressure (r=0.38; p=0.03). Additionally, about 67% of the sample (n=20) exhibited some degree of restrictive ventilatory defect in the pulmonary function test. With respect to muscle strength, 40% of the sample (n=12) displayed below-normal handgrip strength, as well as low mean MIP and MEP.
Conclusion:
Decreased lung capacity may be related to a decline in HGS in patients with chronic kidney disease on hemodialysis. Thus, therapeutic strategies aimed at lung expansion and respiratory muscle training may contribute to facilitating and favoring rehabilitation in this population.
Keywords:
Chronic Kidney Disease; Hemodialysis; Spirometry; Muscle Strength
Resumo
Introdução:
A doença renal crônica (DRC) é definida pela perda da função renal, contudo a sua progressão leva ao surgimento de alterações sistêmicas que comprometem a qualidade de vida dos pacientes em hemodiálise. Consequentemente, a redução da capacidade pulmonar nessa população pode ser um dos fatores que esteja relacionado ao declínio da força muscular periférica.
Objetivo:
Avaliar a relação entre a força de preensão manual (FPM) com a função pulmonar e a força muscular respiratória de pacientes com DRC em hemodiálise.
Método:
30 pacientes com DRC foram avaliados quanto aos dados antropométricos, função pulmonar, força muscular respiratória e FPM.
Resultados:
Observou-se uma relação moderada da FPM com as variáveis capacidade vital forçada (r=0,54; p=0,002), ventilação voluntária máxima (r=0,51; p=0,004) e pressão expiratória máxima (r=0,59; p=0,001). Já as correlações entre a FPM com o volume expiratório forçado no primeiro segundo (r=0,46; p=0,009) e a pressão inspiratória máxima (r=0,38; p=0,03) foram fracas. Além disso, aproximadamente 67% da amostra (n=20) apresentou algum grau de restrição ventilatória na prova de função pulmonar. Em relação à força muscular, 40% da amostra (n=12) apresentou FPM abaixo do previsto de normalidade, e as médias da pressão inspiratória máxima e da pressão expiratória máxima em porcentagem também se encontraram reduzidas.
Conclusão:
A redução da capacidade pulmonar pode estar relacionada com o declínio da FPM nos pacientes com DRC em hemodiálise. Sendo assim, recursos terapêuticos visando à expansão pulmonar e o treinamento muscular respiratório podem ser estratégias para facilitar e favorecer a reabilitação dessa população.
Palavras-chave:
Doença Renal Crônica; Diálise Renal; Espirometria; Força Muscular
Introduction
Chronic kidney disease (CKD) is defined as loss of kidney function, but its progression leads to systemic changes that compromise the quality of life of patients on hemodialysis [11 Stevens PE, Levin A; Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013; 4;158(11):825-30.
2 Kovelis, D, Pitta F, Probst VS, Peres CPA, Delfino VDA, Mocelin AJ, et al. Pulmonary function and respiratory muscle strength in chronic renal failure patients on hemodialysis. J Bras Pneumol. 2008; 34(11):907-12.
3 Cury JL, Brunetto AF, Aydos RD. Efeitos negativos da insuficiência renal crônica sobre a função pulmonar e a capacidade funcional. Rev Bras Fisioter. 2010;14(2).
4 Pereira RA, Cordeiro AC, Avesani CM, Carrero JJ, Lindholm B, Amparo FC. Sarcopenia in chronic kidney disease on conservative therapy: prevalence and association with mortality. Nephrol Dial Transplant. 2015; 30(10):1718-25. - 55 Rogan A, McCarthy K, McGregor G, Hamborg T, Evans G, Hewins S, et al. Quality of life measures predict cardiovascular health and physical performance in chronic renal failure patients. PLoS One. 2017 Sep 14;12(9):e0183926.]. These include sarcopenia [44 Pereira RA, Cordeiro AC, Avesani CM, Carrero JJ, Lindholm B, Amparo FC. Sarcopenia in chronic kidney disease on conservative therapy: prevalence and association with mortality. Nephrol Dial Transplant. 2015; 30(10):1718-25., 6 6 Musso CG, Jauregui JR, Núñez JFM. Frailty phenotype and chronic kidney disease: a review of the literature. Int Urol Nephrol. 2015; 47(11):1801-07.
7 Souza VA, Oliveira D, Mansur HN, Fernandes NMS, Bastos, MG. Sarcopenia in chronic kidney disease. J Bras Nefrol. 2015;37(1):98-105. doi: 10.5935/0101-2800.20150014.
https://doi.org/10.5935/0101-2800.201500...
8 Barata NE. Dyadic relationship and quality of life patients with chronic kidney disease. J Bras Nefrol. 2015; 37(3):315-22. doi: 10.5935/0101-2800.20150051.
https://doi.org/10.5935/0101-2800.201500...
9 Morishita S, Tsubaki A, Shirai N. Physical function was related to mortality in patients with chronic kidney disease and dialysis. Hemodial Int. 2017; 21(4):483-89. doi: 10.1111/hdi.12564.
https://doi.org/10.1111/hdi.12564...
- 1010 Martini A, Ammirati A, Garcia C, Andrade C, Portela O, Cendoroglo MS, et al. Evaluation of quality of life, physical, and mental aspects in longevous patients with chronic kidney disease. Int Urol Nephrol. 2018;50(4):725-31.], which leads to a decline in muscle mass and strength. Given its high prevalence and association with mortality in CKD [44 Pereira RA, Cordeiro AC, Avesani CM, Carrero JJ, Lindholm B, Amparo FC. Sarcopenia in chronic kidney disease on conservative therapy: prevalence and association with mortality. Nephrol Dial Transplant. 2015; 30(10):1718-25., 66 Musso CG, Jauregui JR, Núñez JFM. Frailty phenotype and chronic kidney disease: a review of the literature. Int Urol Nephrol. 2015; 47(11):1801-07.], recent years have seen a growing interest in its evaluation and early diagnosis. Several different measurement techniques are used in clinical practice, particularly handgrip strength (HGS) assessment, an easy low-cost method [1111 Leal VO, Mafra D, Fouque D, Anjos LA. Use of handgrip strength in the assessment of the muscle function of chronic kidney disease patients on dialysis: a systematic review. Nephrol Dial Transplant. 2011; 26(4):1354-360.
12 Vogt BP, Borges MCC, Goés CR, Caramori JCT. Handgrip strength is an independent predictor of all-cause mortality in maintenance dialysis patients. Clin Nutr. 2016; 35(6):1429-1433. - 1313 Tsai YC, Chen HM, Hsiao SM, Chen CS, Lin MY, Chiu YW, et al. Association of physical activity with cardiovascular and renal outcomes and quality of life in chronic kidney disease. PLoS One. 2017; 12(8):e0183642.]. However, systems other than the muscle can also be compromised as CKD progresses.
Previous studies have demonstrated that patients with CKD experience respiratory impairments such as dyspnea, pulmonary dysfunction and reduced respiratory muscle strength [22 Kovelis, D, Pitta F, Probst VS, Peres CPA, Delfino VDA, Mocelin AJ, et al. Pulmonary function and respiratory muscle strength in chronic renal failure patients on hemodialysis. J Bras Pneumol. 2008; 34(11):907-12., 33 Cury JL, Brunetto AF, Aydos RD. Efeitos negativos da insuficiência renal crônica sobre a função pulmonar e a capacidade funcional. Rev Bras Fisioter. 2010;14(2)., 1414 Palamidas AF, Gennimata SA, Karakontaki F, Kaltsakas G, Papantoniou I, Koutsoukou A, et al. Impact of Hemodialysis on Dyspnea and Lung Function in End Stage Kidney Disease Patients. Biomed Res Int. 2014; 2014:212751., 1515 Salerno FR, Parraga G, McIntyre CW. Why Is Your Patient Still Short of Breath? Understanding the Complex Pathophysiology of Dyspnea in Chronic Kidney Disease. Semin Dial. 2017; 30(1):50-7.]. Additionally, Enia et al. [1616 Enia G, Torino C, Panuccio V, Tripepi R, Postorino M, Aliotta R, et al. Asymptomatic Pulmonary Congestion and Physical Functioning in Hemodialysis Patients. Clin J Am Soc Nephrol. 2013; 8(8):1343-48.] reported that patients on hemodialysis with moderate to severe pulmonary edema, even when asymptomatic, showed a decline in physical function. As such, the decline in lung capacity in this population may be one of the factors related to reduced peripheral muscle strength.
Although studies have been conducted to investigate respiratory and physical function outcomes in these individuals, the relationship between lung capacity and functionality in CKD remains unclear. It is vital to elucidate this relationship because if the muscular system is affected by the patient’s worsening respiratory condition, the use of therapeutic intervention aimed at improving ventilation during hemodialysis should be considered. Thus, the aim of this study was to assess the relationship between HGS, pulmonary function and respiratory muscle strength in patients with CKD on hemodialysis.
Method
The study was approved by the Research Ethics Committee of the Universidade do Estado de Santa Catarina (CAAE: 34247814.9.0000.0118). Patients undergoing hemodialysis at Associação Renal Vida in Blumenau, Santa Catarina (SC) state, Brazil, were recruited by convenience sampling and provided written informed consent.
Inclusion criteria were: 1) clinical diagnosis of CKD and undergoing hemodialysis for at least 6 months; 2) under medical supervision and not exhibiting any other acute disease; 3) no recent (3 months or less) coronary artery disease, unstable angina, severe heart arrhythmia, respiratory, orthopedic or neurological diseases; and 4) not participating in any physical activity programs in the last 6 months. Patients were excluded from the study when they were unable to perform any of the assessment tasks due to lack of understanding or cooperation.
Data were collected in one day, before the hemodialysis session. Patients were submitted to anthropometric assessment, pulmonary function testing, and respiratory muscle strength and HGS analysis.
Anthropometric assessment
Weight and height were measured with a digital balance (Actlife Balmak®) and stadiometer (Welmy®), respectively. Body mass index (BMI) was then determined and patients were classified as: underweight (<18.5Kg/m2), normal weight (18.5-24.9 Kg/m2), overweight (25-29.9 Kg/m2) and obese (=30Kg/m2) [1717 World Health Organization. WHO Obesity Technical Report Series. Obesity: preventing and managing the global epidemic. Report of a World Health Organization Consultation. Geneva: World Health Organization; 2000.].
Pulmonary function test
Lung function was evaluated using a previously calibrated portable digital spirometer (EasyOne®; NDD), in accordance with the recommendations of the American Thoracic Society and European Respiratory Society [1818 Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319-38.]. The following variables were analyzed: forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1) and the FEV1/FVC ratio, expressed as absolute values and percentages of predicted normal values [1919 Pereira CADC, Sato T, Rodrigues SC. New reference values for forced spirometry in white adults in Brazil. J Bras Pneumol. 2007; 33(4):397-406.]. Maximum voluntary ventilation (MVV) was also expressed in absolute values and percentages of predicted normal values [2020 Neder JA, Andreoni S, Lerario MC, Nery LE. Reference values for lung function tests II. Maximal respiratory pressures and voluntary ventilation. Braz J Med Biol Res. 1999; 32(6):719-27.]. Patients with FEV1/FVC ≥ 0.7, FVC and FEV1 ≥ 80% were deemed to have normal pulmonary function. Those who exhibited a decline in the variables studied were submitted to another assessment after inhaling a bronchodilator.
Respiratory muscle strength assessment
Respiratory muscle strength was analyzed using a digital manometer (MVD500®), with maneuvers performed according to the Brazilian Pulmonology and Thoracic Society [2121 Souza RB. Pressões respiratórias estáticas máximas. Sociedade Brasileira de Pneumologia e Tisiologia. Diretrizes para testes de função pulmonar. J Pneumol. 2002; 28(Suppl 3):S155-65.]. The highest value obtained during maximal inspiratory (MIP) and expiratory pressure (MEP) maneuvers was considered for analysis, expressed as an absolute value and percentage of the predicted normal value [2020 Neder JA, Andreoni S, Lerario MC, Nery LE. Reference values for lung function tests II. Maximal respiratory pressures and voluntary ventilation. Braz J Med Biol Res. 1999; 32(6):719-27.].
HGS assessment
HGS was evaluated with a hand dynamometer (SAEHAN®), on the upper limb without an arteriovenous fistula. Patients were seated on a chair with no arm rests and instructed to keep their elbows flexed at their side, with the wrists in a neutral position [2222 Fess EE. Grip strength. In: Casanova JS, editor. Clinical assessment recommendations. 2nd ed. Chicago: American Society of Hand Therapists; 1992. p. 41-5.]. Three measurements were taken and the highest was used for analysis. The values described by Novaes et al. were used as reference [2323 Novaes, RD, Miranda AS, Silva JO, Tavares BVF, Dourado VZ. Reference equations for predicting of handgrip strength in Brazilian middle-aged and elderly subjects. Fisioter Pesqui. 2009;16(3):217-22.].
Statistical Analysis
Statistical Package for the Social Sciences software (SPSS version 20.0) was used for all analyses. Data normality was evaluated applying the Shapiro-Wilk test. The relationship between HGS and the variables pulmonary function and respiratory muscle strength were determined by Spearman’s correlation coefficient. Reliability was established based on the magnitude of the coefficient of reliability described by Portney and Watkins [2424 Portney GL, Watkins PM. Reliability. In: Portney GL, Watkins PM, editors. Foundations of Clinical Research Application to Practice. New Jersey: Pearson Prentice Hall; 2008. p. 61-75.]: “weak” for coefficients below 0.50, “moderate” between 0.50 and 0.75 and “good” for those above 0.75. Significance was set at p<0.05.
Results
The sample consisted of 30 patients who underwent three hemodialysis sessions a week. Most were women (56.6%) classified as overweight according to their BMI. In regard to pulmonary function, 10 participants (33.3%) presented with normal function and 20 (66.7%) some form of restrictive ventilatory defect. For HGS, 12 patients (40%) obtained below normal values. Table 1 presents the data on patient characteristics and variables.
Analysis of the correlation between HGS and the remaining study variables shows a moderate correlation with the spirometry variables FVC and MVV (Figures 1 and 2) as well as MEP (Figure 3), and a weak correlation with FEV1 and MIP (Table 2).
Correlation between handgrip strength (HGS) and vital forced capacity (FVC) in the study sample.
Correlation between handgrip strength (HGS) and maximum voluntary ventilation (MVV) in the study sample.
Correlation between handgrip strength (HGS) and maximum expiratory pressure (MEP) in the study sample.
Discussion
The results obtained indicated that HGS was moderately correlated with FVC, MVV and MEP and weakly correlated with FEV1 and MIP, suggesting that reduced peripheral muscle strength may be related to the decline in lung capacity in these patients. This may be due to respiratory dysfunctions caused by the progression of CKD, such as the emergence of pulmonary edema, decreased lung compliance, and reduced lung capacities and volumes [22 Kovelis, D, Pitta F, Probst VS, Peres CPA, Delfino VDA, Mocelin AJ, et al. Pulmonary function and respiratory muscle strength in chronic renal failure patients on hemodialysis. J Bras Pneumol. 2008; 34(11):907-12., 33 Cury JL, Brunetto AF, Aydos RD. Efeitos negativos da insuficiência renal crônica sobre a função pulmonar e a capacidade funcional. Rev Bras Fisioter. 2010;14(2)., 25 25 Coelho CC, Aquino ES, Lara KL, Peres TM, Barja PR, Lima EM. Repercussões da insuficiência renal crônica na capacidade de exercício, estado nutricional, função pulmonar e musculatura respiratória de crianças e adolescentes. Rev Bras Fisioter. 2008;12(1):1-6.
26 Mallamaci F, Benedetto FA, Tripepi R, Rastelli S, Castellino P, Tripepi G, et al. Detection of pulmonary congestion by chest ultrasound in dialysis patients. JACC Cardiovasc Imaging. 2010; 3(6):586-94.- 2727 Yilmaz S, Yildirim Y, Yilmaz Z, Kara AV, Taylan M, Demir M, et al. Pulmonary Function in Patients with End-Stage Renal Disease: Effects of Hemodialysis and Fluid Overload. Med Sci Monit. 2016;22:2779-84.]. These dysfunctions in conjunction with the effects of sarcopenia on the muscles may result in clinical symptoms such as dyspnea [1515 Salerno FR, Parraga G, McIntyre CW. Why Is Your Patient Still Short of Breath? Understanding the Complex Pathophysiology of Dyspnea in Chronic Kidney Disease. Semin Dial. 2017; 30(1):50-7.], favoring an increase in sedentary behavior in this population.
Enia et al. [1616 Enia G, Torino C, Panuccio V, Tripepi R, Postorino M, Aliotta R, et al. Asymptomatic Pulmonary Congestion and Physical Functioning in Hemodialysis Patients. Clin J Am Soc Nephrol. 2013; 8(8):1343-48.] reported that patients on hemodialysis with moderate to severe pulmonary edema, even when asymptomatic, showed a decline in physical function. As such, our findings highlight the need to pay greater attention to lung capacity in patients with CKD, since excessive fluid buildup, especially between hemodialysis sessions, associated with weak respiratory muscles appear to be contributing factors in decreased ventilatory function and may compromise muscle function.
Additionally, the mean values for spirometry variables in our sample were below predicted normal values, corroborating the findings of previous studies [33 Cury JL, Brunetto AF, Aydos RD. Efeitos negativos da insuficiência renal crônica sobre a função pulmonar e a capacidade funcional. Rev Bras Fisioter. 2010;14(2)., 2525 Coelho CC, Aquino ES, Lara KL, Peres TM, Barja PR, Lima EM. Repercussões da insuficiência renal crônica na capacidade de exercício, estado nutricional, função pulmonar e musculatura respiratória de crianças e adolescentes. Rev Bras Fisioter. 2008;12(1):1-6., 2727 Yilmaz S, Yildirim Y, Yilmaz Z, Kara AV, Taylan M, Demir M, et al. Pulmonary Function in Patients with End-Stage Renal Disease: Effects of Hemodialysis and Fluid Overload. Med Sci Monit. 2016;22:2779-84.]. This decline seems to be related to fluid buildup between hemodialysis sessions, which reduces lung compliance, restricts lung parenchyma and obstructs small airways, favoring a decline in lung volumes and capacities [33 Cury JL, Brunetto AF, Aydos RD. Efeitos negativos da insuficiência renal crônica sobre a função pulmonar e a capacidade funcional. Rev Bras Fisioter. 2010;14(2)., 1515 Salerno FR, Parraga G, McIntyre CW. Why Is Your Patient Still Short of Breath? Understanding the Complex Pathophysiology of Dyspnea in Chronic Kidney Disease. Semin Dial. 2017; 30(1):50-7., 2525 Coelho CC, Aquino ES, Lara KL, Peres TM, Barja PR, Lima EM. Repercussões da insuficiência renal crônica na capacidade de exercício, estado nutricional, função pulmonar e musculatura respiratória de crianças e adolescentes. Rev Bras Fisioter. 2008;12(1):1-6., 2727 Yilmaz S, Yildirim Y, Yilmaz Z, Kara AV, Taylan M, Demir M, et al. Pulmonary Function in Patients with End-Stage Renal Disease: Effects of Hemodialysis and Fluid Overload. Med Sci Monit. 2016;22:2779-84.]. Moreover, about 67% of patients displayed some form of restrictive ventilatory defect in the pulmonary function test, indicating the need for therapeutic intervention to improve ventilation in this population.
With respect to muscle strength, 40% of the sample (n=12) displayed HGS below normal values, as well as low mean MIP and MEP. In addition, mean MVV, a marker of respiratory muscle strength, was almost 50% below predicted normal values. These findings confirm those reported in previous studies [33 Cury JL, Brunetto AF, Aydos RD. Efeitos negativos da insuficiência renal crônica sobre a função pulmonar e a capacidade funcional. Rev Bras Fisioter. 2010;14(2)., 2525 Coelho CC, Aquino ES, Lara KL, Peres TM, Barja PR, Lima EM. Repercussões da insuficiência renal crônica na capacidade de exercício, estado nutricional, função pulmonar e musculatura respiratória de crianças e adolescentes. Rev Bras Fisioter. 2008;12(1):1-6., 2828 Broers NJH, Martens RJH, Cornelis T, van der Sande FM, Diederen NMP, Hermans MMH, et al. Physical Activity in End-Stage Renal Disease Patients: The Effects of Starting Dialysis in the First 6 Months after the Transition Period. Nephron. 2017;137(1):47-56., 2929 Kittiskulnam P, Carrero JJ, Chertow GM, Kaysen GA, Delgado C, Johansen KL. Sarcopenia among patients receiving hemodialysis: weighing the evidence. J Cachexia Sarcopenia Muscle. 2017;8(1):57-68.]. These data highlight the damage caused to the muscular system as CKD progresses, resulting in loss of muscle mass, strength and endurance. The imbalance caused by increased catabolism and a decline in anabolism, known as sarcopenia, leads to anatomical and functional changes in the peripheral muscles of these patients, favoring sedentary behavior and low exercise tolerance [33 Cury JL, Brunetto AF, Aydos RD. Efeitos negativos da insuficiência renal crônica sobre a função pulmonar e a capacidade funcional. Rev Bras Fisioter. 2010;14(2)., 66 Musso CG, Jauregui JR, Núñez JFM. Frailty phenotype and chronic kidney disease: a review of the literature. Int Urol Nephrol. 2015; 47(11):1801-07., 77 Souza VA, Oliveira D, Mansur HN, Fernandes NMS, Bastos, MG. Sarcopenia in chronic kidney disease. J Bras Nefrol. 2015;37(1):98-105. doi: 10.5935/0101-2800.20150014.
https://doi.org/10.5935/0101-2800.201500...
].
A limitation of the present study was the failure to use whole body plethysmography to provide a more comprehensive assessment of lung capacity, since this method is considered the gold standard, but we were able to satisfactorily assess lung function via spirometry. Another limitation was that bioelectrical impedance analysis was not applied in order to detect the presence of sarcopenia in this population as opposed to only reduced peripheral muscle strength. However, handgrip strength assessment is an easy low-cost method for application in clinical practice and helps guide professionals who work with these patients, even when hemodialysis clinics do not have the specific tools needed to assess all the aspects required for a sarcopenia diagnosis.
In general, our results emphasize the need for physiotherapists to pay special attention to the dysfunctions in different systems caused by the progression of CKD. Reduced lung capacity seems to be one of the factors that favors decreased peripheral muscle strength in patients on hemodialysis. As such, it is important for patients with CKD to be monitored by a physiotherapist with a view to diagnosing kinetic and functional disorders and ensuring early inclusion of respiratory and peripheral muscle training programs [3030 Pellizzaro CO, Thomé FS, Veronese FV. Effect of peripheral and respiratory muscle training on the functional capacity of hemodialysis patients. Ren Fail. 2013;35(2):189-97.]. Additionally, further research is needed to identify the effects of therapies aimed at increasing lung capacity in patients with chronic kidney disease.
Conclusion
Decreased lung capacity may be related to a decline in HGS in patients with CKD on hemodialysis. Thus, therapeutic strategies aimed at lung expansion and respiratory muscle training may contribute to facilitating and favoring rehabilitation in this population.
Acknowledgments
This study was conducted with the support of Fundação de Amparo à Pesquisa e Inovação do Estado de Santa Catarina, FAPESC / Brazil (PAP UDESC, Public Call No. 04/2018, Granting Term 2019TR658).
References
-
1Stevens PE, Levin A; Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013; 4;158(11):825-30.
-
2Kovelis, D, Pitta F, Probst VS, Peres CPA, Delfino VDA, Mocelin AJ, et al. Pulmonary function and respiratory muscle strength in chronic renal failure patients on hemodialysis. J Bras Pneumol. 2008; 34(11):907-12.
-
3Cury JL, Brunetto AF, Aydos RD. Efeitos negativos da insuficiência renal crônica sobre a função pulmonar e a capacidade funcional. Rev Bras Fisioter. 2010;14(2).
-
4Pereira RA, Cordeiro AC, Avesani CM, Carrero JJ, Lindholm B, Amparo FC. Sarcopenia in chronic kidney disease on conservative therapy: prevalence and association with mortality. Nephrol Dial Transplant. 2015; 30(10):1718-25.
-
5Rogan A, McCarthy K, McGregor G, Hamborg T, Evans G, Hewins S, et al. Quality of life measures predict cardiovascular health and physical performance in chronic renal failure patients. PLoS One. 2017 Sep 14;12(9):e0183926.
-
6Musso CG, Jauregui JR, Núñez JFM. Frailty phenotype and chronic kidney disease: a review of the literature. Int Urol Nephrol. 2015; 47(11):1801-07.
-
7Souza VA, Oliveira D, Mansur HN, Fernandes NMS, Bastos, MG. Sarcopenia in chronic kidney disease. J Bras Nefrol. 2015;37(1):98-105. doi: 10.5935/0101-2800.20150014.
» https://doi.org/10.5935/0101-2800.20150014 -
8Barata NE. Dyadic relationship and quality of life patients with chronic kidney disease. J Bras Nefrol. 2015; 37(3):315-22. doi: 10.5935/0101-2800.20150051.
» https://doi.org/10.5935/0101-2800.20150051 -
9Morishita S, Tsubaki A, Shirai N. Physical function was related to mortality in patients with chronic kidney disease and dialysis. Hemodial Int. 2017; 21(4):483-89. doi: 10.1111/hdi.12564.
» https://doi.org/10.1111/hdi.12564 -
10Martini A, Ammirati A, Garcia C, Andrade C, Portela O, Cendoroglo MS, et al. Evaluation of quality of life, physical, and mental aspects in longevous patients with chronic kidney disease. Int Urol Nephrol. 2018;50(4):725-31.
-
11Leal VO, Mafra D, Fouque D, Anjos LA. Use of handgrip strength in the assessment of the muscle function of chronic kidney disease patients on dialysis: a systematic review. Nephrol Dial Transplant. 2011; 26(4):1354-360.
-
12Vogt BP, Borges MCC, Goés CR, Caramori JCT. Handgrip strength is an independent predictor of all-cause mortality in maintenance dialysis patients. Clin Nutr. 2016; 35(6):1429-1433.
-
13Tsai YC, Chen HM, Hsiao SM, Chen CS, Lin MY, Chiu YW, et al. Association of physical activity with cardiovascular and renal outcomes and quality of life in chronic kidney disease. PLoS One. 2017; 12(8):e0183642.
-
14Palamidas AF, Gennimata SA, Karakontaki F, Kaltsakas G, Papantoniou I, Koutsoukou A, et al. Impact of Hemodialysis on Dyspnea and Lung Function in End Stage Kidney Disease Patients. Biomed Res Int. 2014; 2014:212751.
-
15Salerno FR, Parraga G, McIntyre CW. Why Is Your Patient Still Short of Breath? Understanding the Complex Pathophysiology of Dyspnea in Chronic Kidney Disease. Semin Dial. 2017; 30(1):50-7.
-
16Enia G, Torino C, Panuccio V, Tripepi R, Postorino M, Aliotta R, et al. Asymptomatic Pulmonary Congestion and Physical Functioning in Hemodialysis Patients. Clin J Am Soc Nephrol. 2013; 8(8):1343-48.
-
17World Health Organization. WHO Obesity Technical Report Series. Obesity: preventing and managing the global epidemic. Report of a World Health Organization Consultation. Geneva: World Health Organization; 2000.
-
18Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319-38.
-
19Pereira CADC, Sato T, Rodrigues SC. New reference values for forced spirometry in white adults in Brazil. J Bras Pneumol. 2007; 33(4):397-406.
-
20Neder JA, Andreoni S, Lerario MC, Nery LE. Reference values for lung function tests II. Maximal respiratory pressures and voluntary ventilation. Braz J Med Biol Res. 1999; 32(6):719-27.
-
21Souza RB. Pressões respiratórias estáticas máximas. Sociedade Brasileira de Pneumologia e Tisiologia. Diretrizes para testes de função pulmonar. J Pneumol. 2002; 28(Suppl 3):S155-65.
-
22Fess EE. Grip strength. In: Casanova JS, editor. Clinical assessment recommendations. 2nd ed. Chicago: American Society of Hand Therapists; 1992. p. 41-5.
-
23Novaes, RD, Miranda AS, Silva JO, Tavares BVF, Dourado VZ. Reference equations for predicting of handgrip strength in Brazilian middle-aged and elderly subjects. Fisioter Pesqui. 2009;16(3):217-22.
-
24Portney GL, Watkins PM. Reliability. In: Portney GL, Watkins PM, editors. Foundations of Clinical Research Application to Practice. New Jersey: Pearson Prentice Hall; 2008. p. 61-75.
-
25Coelho CC, Aquino ES, Lara KL, Peres TM, Barja PR, Lima EM. Repercussões da insuficiência renal crônica na capacidade de exercício, estado nutricional, função pulmonar e musculatura respiratória de crianças e adolescentes. Rev Bras Fisioter. 2008;12(1):1-6.
-
26Mallamaci F, Benedetto FA, Tripepi R, Rastelli S, Castellino P, Tripepi G, et al. Detection of pulmonary congestion by chest ultrasound in dialysis patients. JACC Cardiovasc Imaging. 2010; 3(6):586-94.
-
27Yilmaz S, Yildirim Y, Yilmaz Z, Kara AV, Taylan M, Demir M, et al. Pulmonary Function in Patients with End-Stage Renal Disease: Effects of Hemodialysis and Fluid Overload. Med Sci Monit. 2016;22:2779-84.
-
28Broers NJH, Martens RJH, Cornelis T, van der Sande FM, Diederen NMP, Hermans MMH, et al. Physical Activity in End-Stage Renal Disease Patients: The Effects of Starting Dialysis in the First 6 Months after the Transition Period. Nephron. 2017;137(1):47-56.
-
29Kittiskulnam P, Carrero JJ, Chertow GM, Kaysen GA, Delgado C, Johansen KL. Sarcopenia among patients receiving hemodialysis: weighing the evidence. J Cachexia Sarcopenia Muscle. 2017;8(1):57-68.
-
30Pellizzaro CO, Thomé FS, Veronese FV. Effect of peripheral and respiratory muscle training on the functional capacity of hemodialysis patients. Ren Fail. 2013;35(2):189-97.
Publication Dates
-
Publication in this collection
24 July 2020 -
Date of issue
2020
History
-
Received
07 June 2018 -
Accepted
22 July 2019