Dear Editor,
Lichen planus follicularis tumidus (LPFT) is an extremely rare variant of lichen planus (LP). Clinically, it is characterized by white-to-yellow milia-like cysts and comedones, and reddish-to-violaceous plaques. Although it is usually asymptomatic, it may be slightly itchy.11 Belaïch S, Bonvalet D, Civatte J. Follicular tumidus retro-auricular lichen planus (authors transl). Ann Dermatol Venereol. 1977;104:147-50. Its most common location is the retroauricular region, but it has also been rarely described in the bilateral retroauricular area and on the cheeks and neck.22 Grupper Ch, Bensoussan L, Beltzer-Garelly E. Lichen plan folliculaire tumidus rétro-auriculaire bilateral associé a un lichen plan buccal banal leucokératosique et erosif. Ann Dermatol Venereol 1977;104:151.
3 Baptista AP, Rodrigues JB, Cortesão J. Follicular lichen planus tumidus. Ann Dermatol Venereol. 1980;107:1057-9.-44 Jiménez-Gallo D, Albarrán-Planelles C, Linares-Barrios M, Martínez-Rodríguez A, Báez-Perea JM, González-Fernández JA. Facial follicular cysts: a case of lichen planus follicularis tumidus? J Cutan Pathol. 2013;40:818-22. Histopathology of LPFT shows slightly hyperkeratotic or normal epidermis, which is accompanied by follicles and cysts, filled with orthokeratotic keratin, surrounded by dense lichenoid band-like lymphocytic infiltrate, wedge-shaped hypergranulosis, vacuolar degeneration of the basal zone, pigment incontinence and rare colloid bodies in the papillary dermis.44 Jiménez-Gallo D, Albarrán-Planelles C, Linares-Barrios M, Martínez-Rodríguez A, Báez-Perea JM, González-Fernández JA. Facial follicular cysts: a case of lichen planus follicularis tumidus? J Cutan Pathol. 2013;40:818-22. This characteristic morphology and histopathology of LPFT clearly resembles lichen planopilaris. Here we report a rare case of LPFT concomitant with Hashimoto's thyroiditis.
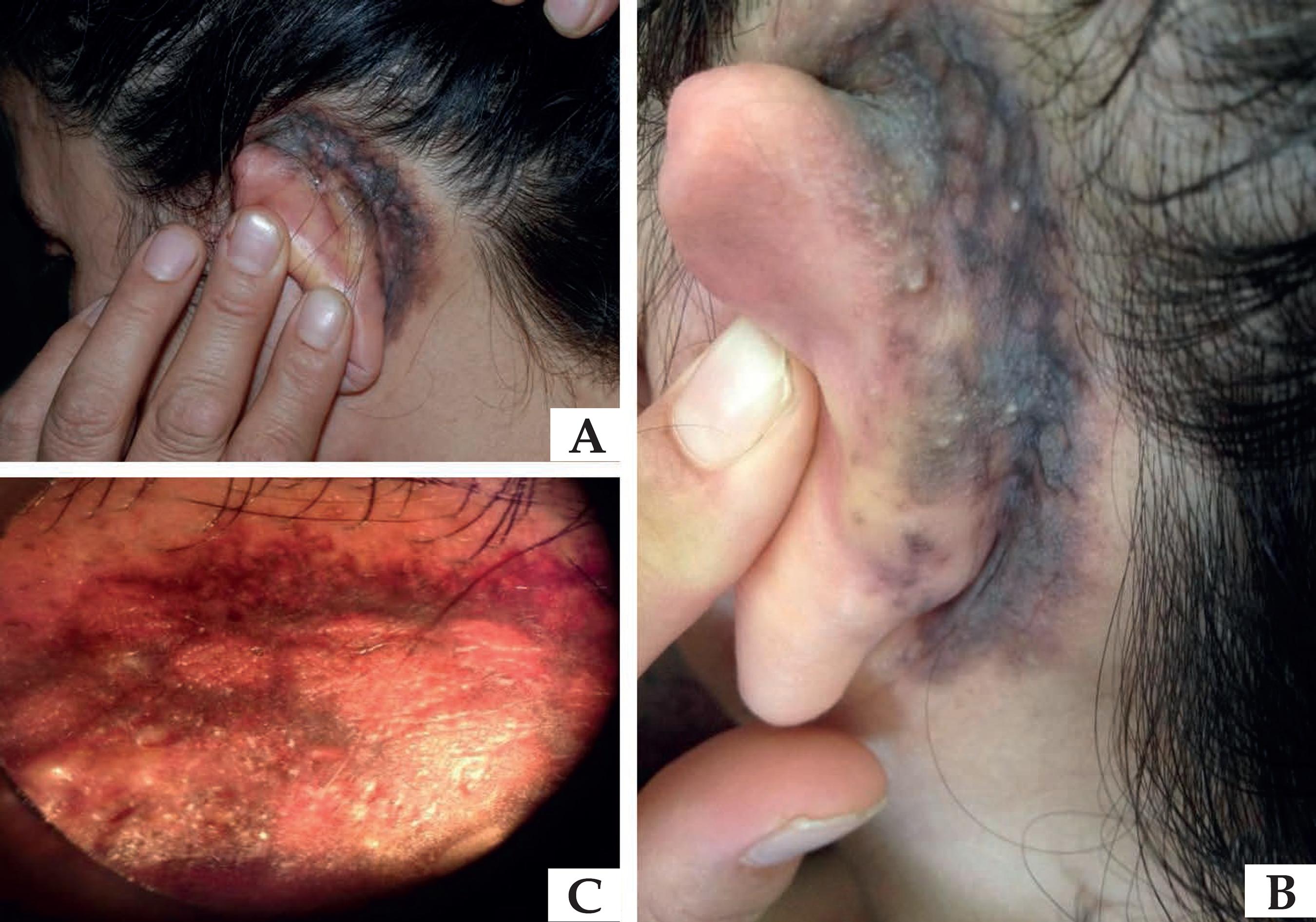
A 54-year-old female patient presented to our clinic with a pruritic, dark-brown pigmented lesion in the left retroauricular region. The patient noticed the lesion 2 years before but observed no changes in appearance to date. Her medical history was unremarkable. She denied using any topical treatment, cosmetic products, or hearing aids. Physical examination revealed a reticular erythematous hyperpigmented tumid violaceous plaque and 1-2 mm milia-like white-to-yellow papules (Figure 1). Dermoscopy of the lesion revealed irregular brownish-blue pigment network, milia-like cysts, and comedo-like openings (Figure 1). We observed no hair, nail, or mucous membrane alterations.
A: Tumid reddish/violaceous plaque with white-to-yellow milia-like papules. B: Close-up of the lesion. 1C: Dermoscopic features of the lesion: irregular brownish-blue pigment network, milia-like cysts and comedo-like openings
Histopathological examination of biopsy specimen taken from the tumid pigmented plaque with milia-like cysts revealed hyperkeratosis, wedge-shaped areas of hypergranulosis, irregular acanthosis, and destruction of the basal layer. The upper dermis showed a band-like lymphohistiocytic infiltrate and prominent pigment incontinence. The papillary dermis revealed some rare areas of eosinophilic colloid bodies (Figure 2). Also, this lymphohistiocytic inflammatory infiltrate surrounded hair follicules and cysts in the dermis. The cysts that were surrounded by stratified squamous epithelium were filled with orthokeratotic keratin (Figure 2). Direct immunofluorescence (DIF) examination was negative. Routine laboratory tests and serological tests were within normal range, but anti-thyroglobulin antibody (130.8 IU/ml) and anti-thyroid peroxidase antibody (230.2 IU/ml) were very high. The patient consulted with an endocrinologist who performed a thyroid ultrasonography. Her thyroid gland was normal size and nodular formation was not detected. Doppler ultrasonography demonstrated a slight increase in blood flow. She was diagnosed with the subclinical stage of Hashimoto's thyroiditis without any symptoms. Based on the clinical and histological course of the disease, we diagnosed LPFT.
A: Hyperkeratosis, wedge-shaped hypergranulosis, irregular acanthosis, and destruction of basal layer (Hematoxylin & eosin X20). B: The upper dermis had a band-like infiltration of lymphohistiocytes and prominent pigmentary incontinence (Hematoxylin & eosin X40). C: The papillary dermis reveals colloid bodies (arrow). D: Presence of lichenoid infiltrate surrounding hair follicles and cysts filled with orthokeratin (Hematoxylin & eosin X20)
LPFT is characterized by tumid violaceous plaques with multiple white-to-yellow cysts and comedones. It is usually asymptomatic and most commonly affects the postauricular region. Although LPFT has been reported in association with other diseases such as hepatitis B and C,44 Jiménez-Gallo D, Albarrán-Planelles C, Linares-Barrios M, Martínez-Rodríguez A, Báez-Perea JM, González-Fernández JA. Facial follicular cysts: a case of lichen planus follicularis tumidus? J Cutan Pathol. 2013;40:818-22. it has not been reported in association with autoimmune diseases yet.
LPFT can be easily differentiated from other cutaneous diseases. Histopathologically, it can be differentiated from nevus comedonicus by its evolution. Follicular mucinosis is ruled out by the lack of mucin in the follicles. Discoid lupus erythematosus is excluded by DIF and follicular mycosis fungoides with folliculotropism and the presence of perifollicular infiltrate of atypical T lymphocytes.44 Jiménez-Gallo D, Albarrán-Planelles C, Linares-Barrios M, Martínez-Rodríguez A, Báez-Perea JM, González-Fernández JA. Facial follicular cysts: a case of lichen planus follicularis tumidus? J Cutan Pathol. 2013;40:818-22. However, differentiating LPFT from milia en plaque (MP) and lichen planopilaris may be challenging. Histologically, no lichenoid reaction is found in MP, but it has been speculated that MP is the sequel to previous LPFT.44 Jiménez-Gallo D, Albarrán-Planelles C, Linares-Barrios M, Martínez-Rodríguez A, Báez-Perea JM, González-Fernández JA. Facial follicular cysts: a case of lichen planus follicularis tumidus? J Cutan Pathol. 2013;40:818-22. Lichen planopilaris (also called follicular LP) is a clinical variant of LP and these entities are generally associated with T-cell-mediated autoimmune disorders.55 Assouly P, Reygagne P. Lichen planopilaris: update on diagnosis and treatment. Semin Cutan Med Surg. 2009;28:3-10. Therefore, patients with LPFT should be thoroughly investigated in terms of autoimmune diseases, as we did with our patient.
We observed a slightly itchy, tumid, violaceous plaque in our patient only in the left retroauricular region and classic lichen planus lesions or systemic symptoms of hypothyroidism were not present. Histopathological examination, besides the pathognomonic findings of lichen planus, revealed band-like lichenoid infiltrate surrounding the follicles and cysts. Therefore, identifying this entity was critical to reach the LPFT diagnosis and to detect the underlying autoimmune disease.
LPFT tends to be chronic, relapsing, and hard to treat. Consequently, all current treatments available are generally disappointing. In our patient, as LPFT is hard to cure and was localized in a small area, clobetasol propionate cream 0.05% therapy is recommended despite the retroauricular localization of the lesion. Additionally, we warned our patient to come to our endocrinology department for control as soon as she noticed symptoms of hypothyroidism or every 6-12 months.
We decided to report on this case not only because LPFT is a very rare clinical variant, but also because it was observed for the first time with autoimmune thyroiditis in the present case.
-
*
Work performed at the Abant Izzet Baysal University - Bolu, Turquia.
-
Financial support: None.
REFERENCES
-
1Belaïch S, Bonvalet D, Civatte J. Follicular tumidus retro-auricular lichen planus (authors transl). Ann Dermatol Venereol. 1977;104:147-50.
-
2Grupper Ch, Bensoussan L, Beltzer-Garelly E. Lichen plan folliculaire tumidus rétro-auriculaire bilateral associé a un lichen plan buccal banal leucokératosique et erosif. Ann Dermatol Venereol 1977;104:151.
-
3Baptista AP, Rodrigues JB, Cortesão J. Follicular lichen planus tumidus. Ann Dermatol Venereol. 1980;107:1057-9.
-
4Jiménez-Gallo D, Albarrán-Planelles C, Linares-Barrios M, Martínez-Rodríguez A, Báez-Perea JM, González-Fernández JA. Facial follicular cysts: a case of lichen planus follicularis tumidus? J Cutan Pathol. 2013;40:818-22.
-
5Assouly P, Reygagne P. Lichen planopilaris: update on diagnosis and treatment. Semin Cutan Med Surg. 2009;28:3-10.
Publication Dates
-
Publication in this collection
Jul-Aug 2017
History
-
Received
05 June 2016 -
Accepted
18 Jan 2017