Abstract
There is an ongoing discussion regarding abdominal muscle (AbM) and pelvic floor muscle (PFM) synergism. Therefore, this study aimed to investigate the cocontraction between AbMs and PFMs in women with or without pelvic floor dysfunction (PFD). The following databases were searched up to December 21, 2018: MEDLINE, EMBASE, LILACS, PEDro and CENTRAL. We included any study that assessed the cocontraction between PFMs and AbMs in women with and without PFD. Two reviewers independently screened eligible articles and extracted data. The outcomes were extracted and analyzed as continuous variables with random effect models. Twenty studies were included. A meta-analysis did not show differences in women with and without PFD. However, a sensitivity analysis suggested cocontraction of the transversus abdominis (TrA) during PFM contraction in healthy women (standardized mean difference (SMD) –1.02 [95% confidence interval (CI) −1.90 to −0.14], P=0.02; I2= not applicable; very low quality of evidence). Women with PFD during contraction of PFMs showed cocontraction of the obliquus internus (OI) (SMD 1.10 [95% CI 0.27 to 1.94], P=0.01; I2= not applicable; very low quality of evidence), and obliquus externus (OE) (SMD 2.08 [95% CI 1.10 to 3.06], P<0.0001; I2 = not applicable; very low quality of evidence). Increased cocontraction of the TrA may be associated with maximal contraction of PFMs in women without PFD. On the other hand, there is likely an increased cocontraction with the OI and OE in women with PFD.
Pelvic Floor Disorders; Abdominopelvic Muscles; Pelvic Floor Function; Synergism
INTRODUCTION
Pelvic floor dysfunction (PFD) refers to a group of disturbances in the pelvic floor muscles (PFM) or connective tissues usually associated with pelvic organ prolapse, urinary and/or anal incontinence, sexual dysfunction, and pelvic pain (11. Bo K, Frawley HC, Haylen BT, Abramov Y, Almeida FG, Berghmans B, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Int Urogynecol J. 2017;28(2):191-213. https://doi.org/10.1007/s00192-016-3123-4.
https://doi.org/10.1007/s00192-016-3123-...
). Treatment-related costs are estimated to correspond to an annual expenditure of 12 billion dollars and are projected to increase every year (22. Chong EC, Khan AA, Anger JT. The financial burden of stress urinary incontinence among women in the United States. Curr Urol Rep. 2011;12(5):358-62. https://doi.org/10.1007/s11934-011-0209-x.
https://doi.org/10.1007/s11934-011-0209-...
), with a considerable prevalence according to the population and definition used (33. Bump RC, Norton PA. Epidemiology and natural history of pelvic floor dysfunction. Obstet Gynecol Clin North Am. 1998;25(4):723-46. https://doi.org/10.1016/S0889-8545(05)70039-5.
https://doi.org/10.1016/S0889-8545(05)70...
). The estimated prevalence is reported to be 25% to 46% in high-income (44. Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, et al. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet Gynecol. 2014;123(1):141-8. https://doi.org/10.1097/AOG.0000000000000057.
https://doi.org/10.1097/AOG.000000000000...
), low-income and middle-income countries (55. Walker GJ, Gunasekera P. Pelvic organ prolapse and incontinence in developing countries: review of prevalence and risk factors. Int Urogynecol J. 2011;22(2):127-35. https://doi.org/10.1007/s00192-010-1215-0.
https://doi.org/10.1007/s00192-010-1215-...
). PFD is a common disease that affects women at all ages, exerting a severe impact on their lives and consuming considerable healthcare resources (44. Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, et al. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet Gynecol. 2014;123(1):141-8. https://doi.org/10.1097/AOG.0000000000000057.
https://doi.org/10.1097/AOG.000000000000...
).
Researchers have reported strategies, such as the use of a model of abdominal muscle (AbM) training to stimulate tonic PFM activity (66. Sapsford RR, Hodges PW. Contraction of the pelvic floor muscles during abdominal maneuvers. Arch Phys Med Rehabil. 2001;82(8):1081-8. https://doi.org/10.1053/apmr.2001.24297.
https://doi.org/10.1053/apmr.2001.24297...
). This scientific evidence is based on the idea of synergistic cocontraction of the PFMs and AbMs, which occurs during normal activities (77. Sapsford R. The Pelvic Floor: A clinical model for function and rehabilitation. Physiotherapy. 2001;87(12):620-30. https://doi.org/10.1016/S0031-9406(05)61107-8.
https://doi.org/10.1016/S0031-9406(05)61...
,88. Sapsford RR, Hodges PW, Richardson CA, Cooper DH, Markwell SJ, Jull GA. Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neurourol Urodyn. 2001;20(1):31-42. https://doi.org/10.1002/1520-6777(2001)20:1<31::AID-NAU5>3.0.CO;2-P.
https://doi.org/10.1002/1520-6777(2001)2...
). Although there is an established literature highlighting that PFM and AbM interaction is usually present in asymptomatic women (99. Madill SJ, McLean L. Relationship between abdominal and pelvic floor muscle activation and intravaginal pressure during pelvic floor muscle contractions in healthy continent women. Neurourol Urodyn. 2006;25(7):722-30. https://doi.org/10.1002/nau.20285.
https://doi.org/10.1002/nau.20285...
), clinical practice guidelines for conservative management of PFD (1010. Nambiar AK, Bosch R, Cruz F, Lemack GE, Thiruchelvam N, Tubaro A, et al. EAU Guidelines on Assessment and Nonsurgical Management of Urinary Incontinence. Eur Urol. 2018;73(4):596-609. https://doi.org/10.1016/j.eururo.2017.12.031.
https://doi.org/10.1016/j.eururo.2017.12...
,1111. Qaseem A, Dallas P, Forciea MA, Starkey M, Denberg TD, Shekelle P, et al. Nonsurgical management of urinary incontinence in women: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2014;161(6):429-40. https://doi.org/10.7326/M13-2410.
https://doi.org/10.7326/M13-2410...
) have demonstrated that the AbMs remain a neglected aspect of care. The addition of AbM training might improve clinical outcomes for patients with PFD (1212. Sapsford R. Rehabilitation of pelvic floor muscles utilizing trunk stabilization. Man Ther. 2004;9(1):3-12. https://doi.org/10.1016/S1356-689X(03)00131-0.
https://doi.org/10.1016/S1356-689X(03)00...
) and restore normal PFM function. The lack of establishment of coactivation between PFMs and AbMs in women with PFD might reflect the lack of robust evidence that exercise regimens other than PFM training would potentially add benefits to conservative management of PFD (1313. Bø K, Herbert RD. There is not yet strong evidence that exercise regimens other than pelvic floor muscle training can reduce stress urinary incontinence in women: a systematic review. J Physiother. 2013;59(3):159-68. https://doi.org/10.1016/S1836-9553(13)70180-2.
https://doi.org/10.1016/S1836-9553(13)70...
).
The understanding of cocontraction among AbMs and PFMs could be valuable for alternative strategies of PFM exercises to promote continence. In this systematic review, we investigate the coactivity of AbMs – transversus abdominis (TrA), rectus abdominis (RA), obliquus internus (OI), and obliquus externus (OE) – and PFMs in women with or without PFD. We hypothesized that women with PFD would show decreased coactivity of the AbMs or PFMs during maximal voluntary contraction (MVC) of the PFMs or AbMs, respectively, compared to women with no history of PFD.
MATERIALS AND METHODS
This review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-analyses - PRISMA (1414. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264-9, W64. https://doi.org/10.7326/0003-4819-151-4-200908180-00135.
https://doi.org/10.7326/0003-4819-151-4-...
) and Meta-analysis of Observational Studies in Epidemiology - MOOSE (1515. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008-12. https://doi.org/10.1001/jama.283.15.2008.
https://doi.org/10.1001/jama.283.15.2008...
) guidelines and was registered on PROSPERO (CRD42017055462).
Eligibility criteria
-
Study design: any observational study (cohort, cross-sectional, comparative cross-sectional) or any baseline subset of data provided by randomized controlled trials, to avoid interaction effects due to any applied interventions. Studies that aimed to assess the reliability of scoring systems for the investigation of cocontraction of the muscles under investigation in this review, as well as studies that provided information on our predefined outcomes, were also included;
-
Participants: women with or without PFD, with urinary incontinence (UI), pelvic organ prolapse (POP), and pelvic pain;
-
Interventions: any voluntary contraction of PFMs that recorded the cocontraction of AbMs (TrA, RA, OI, and OE) and vice versa;
-
Outcomes:
-
-
The cocontraction of AbMs (TrA, RA, OI, and OE) and PFMs was measured by surface electromyography (EMG), ultrasonography (US), a digital palpation scale, or a perineometer;
-
We also considered any indirect assessment of the muscle contraction.
We excluded full-text peer-review studies that evaluated AbMs and PFMs in resting activity.
Data source and searches
Using the Medical Subject Headings (MeSH), based on the combination of terms “female urinary incontinence,” “continent,” “pelvic floor,” “abdominopelvic musculature,” and “abdominal muscle,” we ran the search strategy in MEDLINE (1980 to December 21, 2018), EMBASE (1980 to December 21, 2018), PEDro (1999 to December 21, 2018), LILACS (1982 to December 21, 2018), and CENTRAL (1999 to December 21, 2018). No language restriction was applied. This strategy was similar for the other databases and was executed until December 21, 2018 (Appendix).
Selection of studies
Two reviewers (GV and LARR) independently screened all titles and abstracts identified by the literature search, obtained full-text articles of all potentially relevant records, and evaluated them. Disagreements were resolved through discussion or by consulting a third person (RED).
Data extraction
Data from included studies were summarized in a standardized data extraction with participant demographics, inclusion and exclusion criteria, cocontraction measurement methods, muscles studied and outcomes. Two reviewers (GV and LARR) extracted the sample size, means and standard deviations (SD). When SD data were unavailable, we estimated the SD using the standard error according to the recommendations of the Cochrane Handbook (1616. Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from: http://www.handbook.cochrane.org.
http://www.handbook.cochrane.org...
).
If data regarding methods or results were incomplete, we attempted to contact the authors for further information. Moreover, when we found figures without data, we used the WebPlotDigitizer® (v. 3.8) for Windows to extract an estimation of the data from the figures.
Risk of bias assessment
The risk of bias with a modified version of the Ottawa-Newcastle instrument was independently assessed by the reviewers (1717. Guyatt GH, Busse JW. Modification of Ottawa-Newcastle to assess risk of bias in nonrandomized trials. http://distillercer.com/resources/.
http://distillercer.com/resources/...
). This tool includes confidence in the assessment of exposure and outcome and an adjusted analysis for differences between groups in prognostic characteristics and missing data (1717. Guyatt GH, Busse JW. Modification of Ottawa-Newcastle to assess risk of bias in nonrandomized trials. http://distillercer.com/resources/.
http://distillercer.com/resources/...
). When information regarding risk of bias or other aspects of methods or results was unavailable, we attempted to contact the study authors for additional information.
Certainty of evidence
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) system was used to rate the certainty of the evidence for each outcome measure as high, moderate, low, or very low (1818. Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924-6. https://doi.org/10.1136/bmj.39489.470347.AD.
https://doi.org/10.1136/bmj.39489.470347...
). Detailed GRADE guidance was performed according to the following criteria: imprecision (1919. Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence--imprecision. J Clin Epidemiol. 2011;64(12):1283-93. https://doi.org/10.1016/j.jclinepi.2011.01.012.
https://doi.org/10.1016/j.jclinepi.2011....
), inconsistency (2020. Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 7. Rating the quality of evidence--inconsistency. J Clin Epidemiol. 2011;64(12):1294-302. https://doi.org/10.1016/j.jclinepi.2011.03.017.
https://doi.org/10.1016/j.jclinepi.2011....
), and indirectness (2121. Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 8. Rating the quality of evidence--indirectness. J Clin Epidemiol. 2011;64(12):1303-10. https://doi.org/10.1016/j.jclinepi.2011.04.014.
https://doi.org/10.1016/j.jclinepi.2011....
). The results are summarized in a table of evidence profile.
Data synthesis and statistical analysis
We analyzed the outcomes as continuous variables with random effect models on the results from the muscles investigated (TrA, RA, OI, and OE). Since the assessment of cocontraction in the included studies was measured in different ways (e.g., US and EMG), the individual scales were aligned to point in the same direction, and we calculated the standardized mean difference (SMD) along with the respective confidence interval (CI) of 95%, using the extracted means and SDs (1616. Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from: http://www.handbook.cochrane.org.
http://www.handbook.cochrane.org...
). Positive SMD values indicated higher cocontraction of the evaluated muscle in the PFD group compared to the asymptomatic group, and a negative SMD indicated higher cocontraction of the evaluated muscle in the asymptomatic group compared to the PFD group.
We also conducted sensitivity analyses to test the robustness of these results. When data were obtained from RCTs and the results were provided separately by intervention and control groups, we calculated the baseline mean and SD based on the mean and SD from the studies. Furthermore, when studies provided both the left and right sides of the AbMs, we also calculated the mean and SD based on the mean and SD provided for both sides.
We calculated the heterogeneity across studies using the I2 statistic and the p-value for the Chi-square test using Review Manager software (RevMan version 5.3; Nordic Cochrane Center, Cochrane).
RESULTS
Search results
Figure 1 presents the PRISMA flow diagram for identifying eligible studies based on title and abstract screening. After the assessment of 93 full texts, we included 20 studies included in the systematic review with a subset of data provided by one RCT (2222. Tajiri K, Huo M, Maruyama H. Effects of Co-contraction of Both Transverse Abdominal Muscle and Pelvic Floor Muscle Exercises for Stress Urinary Incontinence: A Randomized Controlled Trial. J Phys Ther Sci. 2014;26(8):1161-3. https://doi.org/10.1589/jpts.26.1161.
https://doi.org/10.1589/jpts.26.1161...
), one prospective (2323. Silva VR, Riccetto CL, Martinho NM, Marques J, Carvalho LC, Botelho S. Training through gametherapy promotes coactivation of the pelvic floor and abdominal muscles in young women, nulliparous and continents. Int Braz J Urol. 2016;42(4):779-86. https://doi.org/10.1590/S1677-5538.IBJU.2014.0580.
https://doi.org/10.1590/S1677-5538.IBJU....
) and 18 cross-sectional studies (88. Sapsford RR, Hodges PW, Richardson CA, Cooper DH, Markwell SJ, Jull GA. Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neurourol Urodyn. 2001;20(1):31-42. https://doi.org/10.1002/1520-6777(2001)20:1<31::AID-NAU5>3.0.CO;2-P.
https://doi.org/10.1002/1520-6777(2001)2...
,99. Madill SJ, McLean L. Relationship between abdominal and pelvic floor muscle activation and intravaginal pressure during pelvic floor muscle contractions in healthy continent women. Neurourol Urodyn. 2006;25(7):722-30. https://doi.org/10.1002/nau.20285.
https://doi.org/10.1002/nau.20285...
,2424. Arab AM, Chehrehrazi M. The response of the abdominal muscles to pelvic floor muscle contraction in women with and without stress urinary incontinence using ultrasound imaging. Neurourol Urodyn. 2011;30(1):117-20. https://doi.org/10.1002/nau.20959.
https://doi.org/10.1002/nau.20959...
25. Bø K, Stien R. Needle EMG registration of striated urethral wall and pelvic floor muscle activity patterns during cough, Valsalva, abdominal, hip adductor, and gluteal muscle contractions in nulliparous healthy females. Neurourol Urodyn. 1994;13(1):35-41. https://doi.org/10.1002/nau.1930130106.
https://doi.org/10.1002/nau.1930130106...
26. Bø K, Kvarstein B, Hagen RR, Larsen S. Pelvic floor muscle exercise for the treatment of female stress urinary incontinence: II. Validity of vaginal pressure measurements of pelvic floor muscle strength and the necessity of supplementary methods of control of correct contraction. Neurourol Urodyn. 1990;9:479-87. https://doi.org/10.1002/nau.1930090504.
https://doi.org/10.1002/nau.1930090504...
27. Bø K, Braekken IH, Majida M, Engh ME. Constriction of the levator hiatus during instruction of pelvic floor or transversus abdominis contraction: a 4D ultrasound study. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(1):27-32. https://doi.org/10.1007/s00192-008-0719-3.
https://doi.org/10.1007/s00192-008-0719-...
28. Chmielewska D, Stania M, Sobota G, Kwasna K, Blaszczak E, Taradaj J, et al. Impact of different body positions on bioelectrical activity of the pelvic floor muscles in nulliparous continent women. Biomed Res Int. 2015;2015:905897. https://doi.org/10.1155/2015/905897.
https://doi.org/10.1155/2015/905897...
29. Devreese A, Staes F, De Weerdt W, Feys H, Van Assche A, Penninckx F, et al. Clinical evaluation of pelvic floor muscle function in continent and incontinent women. Neurourol Urodyn. 2004;23(3):190-7. https://doi.org/10.1002/nau.20018.
https://doi.org/10.1002/nau.20018...
30. Junginger B, Baessler K, Sapsford R, Hodges PW. Effect of abdominal and pelvic floor tasks on muscle activity, abdominal pressure and bladder neck. Int Urogynecol J. 2010;21(1):69-77. https://doi.org/10.1007/s00192-009-0981-z.
https://doi.org/10.1007/s00192-009-0981-...
31. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
32. Madill SJ, McLean L. Quantification of abdominal and pelvic floor muscle synergies in response to voluntary pelvic floor muscle contractions. J Electromyogr Kinesiol. 2008;18(6):955-64. https://doi.org/10.1016/j.jelekin.2007.05.001.
https://doi.org/10.1016/j.jelekin.2007.0...
33. Neumann P, Gill V. Pelvic floor and abdominal muscle interaction: EMG activity and intra-abdominal pressure. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13(2):125-32. https://doi.org/10.1007/s001920200027.
https://doi.org/10.1007/s001920200027...
34. Ptaszkowski K, Paprocka-Borowicz M, Slupska L, Bartnicki J, Dymarek R, Rosinczuk J, et al. Assessment of bioelectrical activity of synergistic muscles during pelvic floor muscles activation in postmenopausal women with and without stress urinary incontinence: a preliminary observational study. Clin Interv Aging. 2015;10:1521-8. https://doi.org/10.2147/CIA.S89852.
https://doi.org/10.2147/CIA.S89852...
35. Stupp L, Resende AP, Petricelli CD, Nakamura MU, Alexandre SM, Zanetti MR. Pelvic floor muscle and transversus abdominis activation in abdominal hypopressive technique through surface electromyography. Neurourol Urodyn. 2011;30(8):1518-21. https://doi.org/10.1002/nau.21151.
https://doi.org/10.1002/nau.21151...
36. Tajiri K, Huo M, Yin K, Fujisawa S, Maruyama H. An approach to assessment of female urinary incontinence risk using the thickness of the transverse abdominal muscle during co-contraction of both the transverse abdominal muscle and the pelvic floor muscle. J Phys Ther Sci. 2011;23(1):45-8. https://doi.org/10.1589/jpts.23.45.
https://doi.org/10.1589/jpts.23.45...
37. Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Differences in muscle activation patterns during pelvic floor muscle contraction and Valsalva maneuver. Neurourol Urodyn. 2006;25(2):148-55. https://doi.org/10.1002/nau.20203.
https://doi.org/10.1002/nau.20203...
38. Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Altered muscle activation patterns in symptomatic women during pelvic floor muscle contraction and Valsalva manouevre. Neurourol Urodyn. 2006;25(3):268-76. https://doi.org/10.1002/nau.20183.
https://doi.org/10.1002/nau.20183...
-3939. Ithamar L, de Moura Filho AG, Benedetti Rodrigues MA, Duque Cortez KC, Machado VG, de Paiva Lima CRO, et al. Abdominal and pelvic floor electromyographic analysis during abdominal hypopressive gymnastics. J Bodyw Mov Ther. 2018;22(1):159-65. https://doi.org/10.1016/j.jbmt.2017.06.011.
https://doi.org/10.1016/j.jbmt.2017.06.0...
) with a total of 468 participants. The interobserver agreement for screening was substantial (kappa 0.82).
Study characteristics
The sample size of the studies ranged from three (2626. Bø K, Kvarstein B, Hagen RR, Larsen S. Pelvic floor muscle exercise for the treatment of female stress urinary incontinence: II. Validity of vaginal pressure measurements of pelvic floor muscle strength and the necessity of supplementary methods of control of correct contraction. Neurourol Urodyn. 1990;9:479-87. https://doi.org/10.1002/nau.1930090504.
https://doi.org/10.1002/nau.1930090504...
) to 44 (3131. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
) participants. Typical participants were aged from 19 (2525. Bø K, Stien R. Needle EMG registration of striated urethral wall and pelvic floor muscle activity patterns during cough, Valsalva, abdominal, hip adductor, and gluteal muscle contractions in nulliparous healthy females. Neurourol Urodyn. 1994;13(1):35-41. https://doi.org/10.1002/nau.1930130106.
https://doi.org/10.1002/nau.1930130106...
) to 66 (3434. Ptaszkowski K, Paprocka-Borowicz M, Slupska L, Bartnicki J, Dymarek R, Rosinczuk J, et al. Assessment of bioelectrical activity of synergistic muscles during pelvic floor muscles activation in postmenopausal women with and without stress urinary incontinence: a preliminary observational study. Clin Interv Aging. 2015;10:1521-8. https://doi.org/10.2147/CIA.S89852.
https://doi.org/10.2147/CIA.S89852...
) years old (Table 1). From a total of 20 included studies, four (88. Sapsford RR, Hodges PW, Richardson CA, Cooper DH, Markwell SJ, Jull GA. Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neurourol Urodyn. 2001;20(1):31-42. https://doi.org/10.1002/1520-6777(2001)20:1<31::AID-NAU5>3.0.CO;2-P.
https://doi.org/10.1002/1520-6777(2001)2...
,99. Madill SJ, McLean L. Relationship between abdominal and pelvic floor muscle activation and intravaginal pressure during pelvic floor muscle contractions in healthy continent women. Neurourol Urodyn. 2006;25(7):722-30. https://doi.org/10.1002/nau.20285.
https://doi.org/10.1002/nau.20285...
,3232. Madill SJ, McLean L. Quantification of abdominal and pelvic floor muscle synergies in response to voluntary pelvic floor muscle contractions. J Electromyogr Kinesiol. 2008;18(6):955-64. https://doi.org/10.1016/j.jelekin.2007.05.001.
https://doi.org/10.1016/j.jelekin.2007.0...
,3939. Ithamar L, de Moura Filho AG, Benedetti Rodrigues MA, Duque Cortez KC, Machado VG, de Paiva Lima CRO, et al. Abdominal and pelvic floor electromyographic analysis during abdominal hypopressive gymnastics. J Bodyw Mov Ther. 2018;22(1):159-65. https://doi.org/10.1016/j.jbmt.2017.06.011.
https://doi.org/10.1016/j.jbmt.2017.06.0...
) recorded the activity of all AbMs (TrA, RA, OI, and OE) during PFM contraction, and 19 studies provided instructions to contract the PFMs and recorded the AbM coactivity (88. Sapsford RR, Hodges PW, Richardson CA, Cooper DH, Markwell SJ, Jull GA. Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neurourol Urodyn. 2001;20(1):31-42. https://doi.org/10.1002/1520-6777(2001)20:1<31::AID-NAU5>3.0.CO;2-P.
https://doi.org/10.1002/1520-6777(2001)2...
,99. Madill SJ, McLean L. Relationship between abdominal and pelvic floor muscle activation and intravaginal pressure during pelvic floor muscle contractions in healthy continent women. Neurourol Urodyn. 2006;25(7):722-30. https://doi.org/10.1002/nau.20285.
https://doi.org/10.1002/nau.20285...
,2222. Tajiri K, Huo M, Maruyama H. Effects of Co-contraction of Both Transverse Abdominal Muscle and Pelvic Floor Muscle Exercises for Stress Urinary Incontinence: A Randomized Controlled Trial. J Phys Ther Sci. 2014;26(8):1161-3. https://doi.org/10.1589/jpts.26.1161.
https://doi.org/10.1589/jpts.26.1161...
23. Silva VR, Riccetto CL, Martinho NM, Marques J, Carvalho LC, Botelho S. Training through gametherapy promotes coactivation of the pelvic floor and abdominal muscles in young women, nulliparous and continents. Int Braz J Urol. 2016;42(4):779-86. https://doi.org/10.1590/S1677-5538.IBJU.2014.0580.
https://doi.org/10.1590/S1677-5538.IBJU....
24. Arab AM, Chehrehrazi M. The response of the abdominal muscles to pelvic floor muscle contraction in women with and without stress urinary incontinence using ultrasound imaging. Neurourol Urodyn. 2011;30(1):117-20. https://doi.org/10.1002/nau.20959.
https://doi.org/10.1002/nau.20959...
25. Bø K, Stien R. Needle EMG registration of striated urethral wall and pelvic floor muscle activity patterns during cough, Valsalva, abdominal, hip adductor, and gluteal muscle contractions in nulliparous healthy females. Neurourol Urodyn. 1994;13(1):35-41. https://doi.org/10.1002/nau.1930130106.
https://doi.org/10.1002/nau.1930130106...
26. Bø K, Kvarstein B, Hagen RR, Larsen S. Pelvic floor muscle exercise for the treatment of female stress urinary incontinence: II. Validity of vaginal pressure measurements of pelvic floor muscle strength and the necessity of supplementary methods of control of correct contraction. Neurourol Urodyn. 1990;9:479-87. https://doi.org/10.1002/nau.1930090504.
https://doi.org/10.1002/nau.1930090504...
27. Bø K, Braekken IH, Majida M, Engh ME. Constriction of the levator hiatus during instruction of pelvic floor or transversus abdominis contraction: a 4D ultrasound study. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(1):27-32. https://doi.org/10.1007/s00192-008-0719-3.
https://doi.org/10.1007/s00192-008-0719-...
28. Chmielewska D, Stania M, Sobota G, Kwasna K, Blaszczak E, Taradaj J, et al. Impact of different body positions on bioelectrical activity of the pelvic floor muscles in nulliparous continent women. Biomed Res Int. 2015;2015:905897. https://doi.org/10.1155/2015/905897.
https://doi.org/10.1155/2015/905897...
29. Devreese A, Staes F, De Weerdt W, Feys H, Van Assche A, Penninckx F, et al. Clinical evaluation of pelvic floor muscle function in continent and incontinent women. Neurourol Urodyn. 2004;23(3):190-7. https://doi.org/10.1002/nau.20018.
https://doi.org/10.1002/nau.20018...
30. Junginger B, Baessler K, Sapsford R, Hodges PW. Effect of abdominal and pelvic floor tasks on muscle activity, abdominal pressure and bladder neck. Int Urogynecol J. 2010;21(1):69-77. https://doi.org/10.1007/s00192-009-0981-z.
https://doi.org/10.1007/s00192-009-0981-...
31. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
32. Madill SJ, McLean L. Quantification of abdominal and pelvic floor muscle synergies in response to voluntary pelvic floor muscle contractions. J Electromyogr Kinesiol. 2008;18(6):955-64. https://doi.org/10.1016/j.jelekin.2007.05.001.
https://doi.org/10.1016/j.jelekin.2007.0...
33. Neumann P, Gill V. Pelvic floor and abdominal muscle interaction: EMG activity and intra-abdominal pressure. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13(2):125-32. https://doi.org/10.1007/s001920200027.
https://doi.org/10.1007/s001920200027...
34. Ptaszkowski K, Paprocka-Borowicz M, Slupska L, Bartnicki J, Dymarek R, Rosinczuk J, et al. Assessment of bioelectrical activity of synergistic muscles during pelvic floor muscles activation in postmenopausal women with and without stress urinary incontinence: a preliminary observational study. Clin Interv Aging. 2015;10:1521-8. https://doi.org/10.2147/CIA.S89852.
https://doi.org/10.2147/CIA.S89852...
-3535. Stupp L, Resende AP, Petricelli CD, Nakamura MU, Alexandre SM, Zanetti MR. Pelvic floor muscle and transversus abdominis activation in abdominal hypopressive technique through surface electromyography. Neurourol Urodyn. 2011;30(8):1518-21. https://doi.org/10.1002/nau.21151.
https://doi.org/10.1002/nau.21151...
,3737. Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Differences in muscle activation patterns during pelvic floor muscle contraction and Valsalva maneuver. Neurourol Urodyn. 2006;25(2):148-55. https://doi.org/10.1002/nau.20203.
https://doi.org/10.1002/nau.20203...
38. Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Altered muscle activation patterns in symptomatic women during pelvic floor muscle contraction and Valsalva manouevre. Neurourol Urodyn. 2006;25(3):268-76. https://doi.org/10.1002/nau.20183.
https://doi.org/10.1002/nau.20183...
-3939. Ithamar L, de Moura Filho AG, Benedetti Rodrigues MA, Duque Cortez KC, Machado VG, de Paiva Lima CRO, et al. Abdominal and pelvic floor electromyographic analysis during abdominal hypopressive gymnastics. J Bodyw Mov Ther. 2018;22(1):159-65. https://doi.org/10.1016/j.jbmt.2017.06.011.
https://doi.org/10.1016/j.jbmt.2017.06.0...
). Fifteen studies (88. Sapsford RR, Hodges PW, Richardson CA, Cooper DH, Markwell SJ, Jull GA. Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neurourol Urodyn. 2001;20(1):31-42. https://doi.org/10.1002/1520-6777(2001)20:1<31::AID-NAU5>3.0.CO;2-P.
https://doi.org/10.1002/1520-6777(2001)2...
,99. Madill SJ, McLean L. Relationship between abdominal and pelvic floor muscle activation and intravaginal pressure during pelvic floor muscle contractions in healthy continent women. Neurourol Urodyn. 2006;25(7):722-30. https://doi.org/10.1002/nau.20285.
https://doi.org/10.1002/nau.20285...
,2222. Tajiri K, Huo M, Maruyama H. Effects of Co-contraction of Both Transverse Abdominal Muscle and Pelvic Floor Muscle Exercises for Stress Urinary Incontinence: A Randomized Controlled Trial. J Phys Ther Sci. 2014;26(8):1161-3. https://doi.org/10.1589/jpts.26.1161.
https://doi.org/10.1589/jpts.26.1161...
23. Silva VR, Riccetto CL, Martinho NM, Marques J, Carvalho LC, Botelho S. Training through gametherapy promotes coactivation of the pelvic floor and abdominal muscles in young women, nulliparous and continents. Int Braz J Urol. 2016;42(4):779-86. https://doi.org/10.1590/S1677-5538.IBJU.2014.0580.
https://doi.org/10.1590/S1677-5538.IBJU....
-2424. Arab AM, Chehrehrazi M. The response of the abdominal muscles to pelvic floor muscle contraction in women with and without stress urinary incontinence using ultrasound imaging. Neurourol Urodyn. 2011;30(1):117-20. https://doi.org/10.1002/nau.20959.
https://doi.org/10.1002/nau.20959...
,2623. Silva VR, Riccetto CL, Martinho NM, Marques J, Carvalho LC, Botelho S. Training through gametherapy promotes coactivation of the pelvic floor and abdominal muscles in young women, nulliparous and continents. Int Braz J Urol. 2016;42(4):779-86. https://doi.org/10.1590/S1677-5538.IBJU.2014.0580.
https://doi.org/10.1590/S1677-5538.IBJU....
,2824. Arab AM, Chehrehrazi M. The response of the abdominal muscles to pelvic floor muscle contraction in women with and without stress urinary incontinence using ultrasound imaging. Neurourol Urodyn. 2011;30(1):117-20. https://doi.org/10.1002/nau.20959.
https://doi.org/10.1002/nau.20959...
,3131. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
32. Madill SJ, McLean L. Quantification of abdominal and pelvic floor muscle synergies in response to voluntary pelvic floor muscle contractions. J Electromyogr Kinesiol. 2008;18(6):955-64. https://doi.org/10.1016/j.jelekin.2007.05.001.
https://doi.org/10.1016/j.jelekin.2007.0...
33. Neumann P, Gill V. Pelvic floor and abdominal muscle interaction: EMG activity and intra-abdominal pressure. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13(2):125-32. https://doi.org/10.1007/s001920200027.
https://doi.org/10.1007/s001920200027...
34. Ptaszkowski K, Paprocka-Borowicz M, Slupska L, Bartnicki J, Dymarek R, Rosinczuk J, et al. Assessment of bioelectrical activity of synergistic muscles during pelvic floor muscles activation in postmenopausal women with and without stress urinary incontinence: a preliminary observational study. Clin Interv Aging. 2015;10:1521-8. https://doi.org/10.2147/CIA.S89852.
https://doi.org/10.2147/CIA.S89852...
35. Stupp L, Resende AP, Petricelli CD, Nakamura MU, Alexandre SM, Zanetti MR. Pelvic floor muscle and transversus abdominis activation in abdominal hypopressive technique through surface electromyography. Neurourol Urodyn. 2011;30(8):1518-21. https://doi.org/10.1002/nau.21151.
https://doi.org/10.1002/nau.21151...
36. Tajiri K, Huo M, Yin K, Fujisawa S, Maruyama H. An approach to assessment of female urinary incontinence risk using the thickness of the transverse abdominal muscle during co-contraction of both the transverse abdominal muscle and the pelvic floor muscle. J Phys Ther Sci. 2011;23(1):45-8. https://doi.org/10.1589/jpts.23.45.
https://doi.org/10.1589/jpts.23.45...
-3737. Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Differences in muscle activation patterns during pelvic floor muscle contraction and Valsalva maneuver. Neurourol Urodyn. 2006;25(2):148-55. https://doi.org/10.1002/nau.20203.
https://doi.org/10.1002/nau.20203...
,3939. Ithamar L, de Moura Filho AG, Benedetti Rodrigues MA, Duque Cortez KC, Machado VG, de Paiva Lima CRO, et al. Abdominal and pelvic floor electromyographic analysis during abdominal hypopressive gymnastics. J Bodyw Mov Ther. 2018;22(1):159-65. https://doi.org/10.1016/j.jbmt.2017.06.011.
https://doi.org/10.1016/j.jbmt.2017.06.0...
) reported the MVC of the PFMs. Three studies (2323. Silva VR, Riccetto CL, Martinho NM, Marques J, Carvalho LC, Botelho S. Training through gametherapy promotes coactivation of the pelvic floor and abdominal muscles in young women, nulliparous and continents. Int Braz J Urol. 2016;42(4):779-86. https://doi.org/10.1590/S1677-5538.IBJU.2014.0580.
https://doi.org/10.1590/S1677-5538.IBJU....
,2727. Bø K, Braekken IH, Majida M, Engh ME. Constriction of the levator hiatus during instruction of pelvic floor or transversus abdominis contraction: a 4D ultrasound study. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(1):27-32. https://doi.org/10.1007/s00192-008-0719-3.
https://doi.org/10.1007/s00192-008-0719-...
,3434. Ptaszkowski K, Paprocka-Borowicz M, Slupska L, Bartnicki J, Dymarek R, Rosinczuk J, et al. Assessment of bioelectrical activity of synergistic muscles during pelvic floor muscles activation in postmenopausal women with and without stress urinary incontinence: a preliminary observational study. Clin Interv Aging. 2015;10:1521-8. https://doi.org/10.2147/CIA.S89852.
https://doi.org/10.2147/CIA.S89852...
) considered the standing position for the assessment of the coactivity, and another eleven studies considered the supine position (88. Sapsford RR, Hodges PW, Richardson CA, Cooper DH, Markwell SJ, Jull GA. Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neurourol Urodyn. 2001;20(1):31-42. https://doi.org/10.1002/1520-6777(2001)20:1<31::AID-NAU5>3.0.CO;2-P.
https://doi.org/10.1002/1520-6777(2001)2...
,99. Madill SJ, McLean L. Relationship between abdominal and pelvic floor muscle activation and intravaginal pressure during pelvic floor muscle contractions in healthy continent women. Neurourol Urodyn. 2006;25(7):722-30. https://doi.org/10.1002/nau.20285.
https://doi.org/10.1002/nau.20285...
,2222. Tajiri K, Huo M, Maruyama H. Effects of Co-contraction of Both Transverse Abdominal Muscle and Pelvic Floor Muscle Exercises for Stress Urinary Incontinence: A Randomized Controlled Trial. J Phys Ther Sci. 2014;26(8):1161-3. https://doi.org/10.1589/jpts.26.1161.
https://doi.org/10.1589/jpts.26.1161...
,2525. Bø K, Stien R. Needle EMG registration of striated urethral wall and pelvic floor muscle activity patterns during cough, Valsalva, abdominal, hip adductor, and gluteal muscle contractions in nulliparous healthy females. Neurourol Urodyn. 1994;13(1):35-41. https://doi.org/10.1002/nau.1930130106.
https://doi.org/10.1002/nau.1930130106...
,2929. Devreese A, Staes F, De Weerdt W, Feys H, Van Assche A, Penninckx F, et al. Clinical evaluation of pelvic floor muscle function in continent and incontinent women. Neurourol Urodyn. 2004;23(3):190-7. https://doi.org/10.1002/nau.20018.
https://doi.org/10.1002/nau.20018...
30. Junginger B, Baessler K, Sapsford R, Hodges PW. Effect of abdominal and pelvic floor tasks on muscle activity, abdominal pressure and bladder neck. Int Urogynecol J. 2010;21(1):69-77. https://doi.org/10.1007/s00192-009-0981-z.
https://doi.org/10.1007/s00192-009-0981-...
-3131. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
,3535. Stupp L, Resende AP, Petricelli CD, Nakamura MU, Alexandre SM, Zanetti MR. Pelvic floor muscle and transversus abdominis activation in abdominal hypopressive technique through surface electromyography. Neurourol Urodyn. 2011;30(8):1518-21. https://doi.org/10.1002/nau.21151.
https://doi.org/10.1002/nau.21151...
36. Tajiri K, Huo M, Yin K, Fujisawa S, Maruyama H. An approach to assessment of female urinary incontinence risk using the thickness of the transverse abdominal muscle during co-contraction of both the transverse abdominal muscle and the pelvic floor muscle. J Phys Ther Sci. 2011;23(1):45-8. https://doi.org/10.1589/jpts.23.45.
https://doi.org/10.1589/jpts.23.45...
37. Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Differences in muscle activation patterns during pelvic floor muscle contraction and Valsalva maneuver. Neurourol Urodyn. 2006;25(2):148-55. https://doi.org/10.1002/nau.20203.
https://doi.org/10.1002/nau.20203...
-3838. Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Altered muscle activation patterns in symptomatic women during pelvic floor muscle contraction and Valsalva manouevre. Neurourol Urodyn. 2006;25(3):268-76. https://doi.org/10.1002/nau.20183.
https://doi.org/10.1002/nau.20183...
). Four studies (2828. Chmielewska D, Stania M, Sobota G, Kwasna K, Blaszczak E, Taradaj J, et al. Impact of different body positions on bioelectrical activity of the pelvic floor muscles in nulliparous continent women. Biomed Res Int. 2015;2015:905897. https://doi.org/10.1155/2015/905897.
https://doi.org/10.1155/2015/905897...
,3232. Madill SJ, McLean L. Quantification of abdominal and pelvic floor muscle synergies in response to voluntary pelvic floor muscle contractions. J Electromyogr Kinesiol. 2008;18(6):955-64. https://doi.org/10.1016/j.jelekin.2007.05.001.
https://doi.org/10.1016/j.jelekin.2007.0...
,3333. Neumann P, Gill V. Pelvic floor and abdominal muscle interaction: EMG activity and intra-abdominal pressure. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13(2):125-32. https://doi.org/10.1007/s001920200027.
https://doi.org/10.1007/s001920200027...
,3939. Ithamar L, de Moura Filho AG, Benedetti Rodrigues MA, Duque Cortez KC, Machado VG, de Paiva Lima CRO, et al. Abdominal and pelvic floor electromyographic analysis during abdominal hypopressive gymnastics. J Bodyw Mov Ther. 2018;22(1):159-65. https://doi.org/10.1016/j.jbmt.2017.06.011.
https://doi.org/10.1016/j.jbmt.2017.06.0...
) considered different positions – standing, sitting and supine, and one did not report the position for the assessment of coactivity (2626. Bø K, Kvarstein B, Hagen RR, Larsen S. Pelvic floor muscle exercise for the treatment of female stress urinary incontinence: II. Validity of vaginal pressure measurements of pelvic floor muscle strength and the necessity of supplementary methods of control of correct contraction. Neurourol Urodyn. 1990;9:479-87. https://doi.org/10.1002/nau.1930090504.
https://doi.org/10.1002/nau.1930090504...
). Fifteen studies (88. Sapsford RR, Hodges PW, Richardson CA, Cooper DH, Markwell SJ, Jull GA. Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neurourol Urodyn. 2001;20(1):31-42. https://doi.org/10.1002/1520-6777(2001)20:1<31::AID-NAU5>3.0.CO;2-P.
https://doi.org/10.1002/1520-6777(2001)2...
,99. Madill SJ, McLean L. Relationship between abdominal and pelvic floor muscle activation and intravaginal pressure during pelvic floor muscle contractions in healthy continent women. Neurourol Urodyn. 2006;25(7):722-30. https://doi.org/10.1002/nau.20285.
https://doi.org/10.1002/nau.20285...
,2323. Silva VR, Riccetto CL, Martinho NM, Marques J, Carvalho LC, Botelho S. Training through gametherapy promotes coactivation of the pelvic floor and abdominal muscles in young women, nulliparous and continents. Int Braz J Urol. 2016;42(4):779-86. https://doi.org/10.1590/S1677-5538.IBJU.2014.0580.
https://doi.org/10.1590/S1677-5538.IBJU....
,2525. Bø K, Stien R. Needle EMG registration of striated urethral wall and pelvic floor muscle activity patterns during cough, Valsalva, abdominal, hip adductor, and gluteal muscle contractions in nulliparous healthy females. Neurourol Urodyn. 1994;13(1):35-41. https://doi.org/10.1002/nau.1930130106.
https://doi.org/10.1002/nau.1930130106...
,2626. Bø K, Kvarstein B, Hagen RR, Larsen S. Pelvic floor muscle exercise for the treatment of female stress urinary incontinence: II. Validity of vaginal pressure measurements of pelvic floor muscle strength and the necessity of supplementary methods of control of correct contraction. Neurourol Urodyn. 1990;9:479-87. https://doi.org/10.1002/nau.1930090504.
https://doi.org/10.1002/nau.1930090504...
,2828. Chmielewska D, Stania M, Sobota G, Kwasna K, Blaszczak E, Taradaj J, et al. Impact of different body positions on bioelectrical activity of the pelvic floor muscles in nulliparous continent women. Biomed Res Int. 2015;2015:905897. https://doi.org/10.1155/2015/905897.
https://doi.org/10.1155/2015/905897...
,3030. Junginger B, Baessler K, Sapsford R, Hodges PW. Effect of abdominal and pelvic floor tasks on muscle activity, abdominal pressure and bladder neck. Int Urogynecol J. 2010;21(1):69-77. https://doi.org/10.1007/s00192-009-0981-z.
https://doi.org/10.1007/s00192-009-0981-...
31. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
32. Madill SJ, McLean L. Quantification of abdominal and pelvic floor muscle synergies in response to voluntary pelvic floor muscle contractions. J Electromyogr Kinesiol. 2008;18(6):955-64. https://doi.org/10.1016/j.jelekin.2007.05.001.
https://doi.org/10.1016/j.jelekin.2007.0...
33. Neumann P, Gill V. Pelvic floor and abdominal muscle interaction: EMG activity and intra-abdominal pressure. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13(2):125-32. https://doi.org/10.1007/s001920200027.
https://doi.org/10.1007/s001920200027...
34. Ptaszkowski K, Paprocka-Borowicz M, Slupska L, Bartnicki J, Dymarek R, Rosinczuk J, et al. Assessment of bioelectrical activity of synergistic muscles during pelvic floor muscles activation in postmenopausal women with and without stress urinary incontinence: a preliminary observational study. Clin Interv Aging. 2015;10:1521-8. https://doi.org/10.2147/CIA.S89852.
https://doi.org/10.2147/CIA.S89852...
-3535. Stupp L, Resende AP, Petricelli CD, Nakamura MU, Alexandre SM, Zanetti MR. Pelvic floor muscle and transversus abdominis activation in abdominal hypopressive technique through surface electromyography. Neurourol Urodyn. 2011;30(8):1518-21. https://doi.org/10.1002/nau.21151.
https://doi.org/10.1002/nau.21151...
,3737. Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Differences in muscle activation patterns during pelvic floor muscle contraction and Valsalva maneuver. Neurourol Urodyn. 2006;25(2):148-55. https://doi.org/10.1002/nau.20203.
https://doi.org/10.1002/nau.20203...
38. Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Altered muscle activation patterns in symptomatic women during pelvic floor muscle contraction and Valsalva manouevre. Neurourol Urodyn. 2006;25(3):268-76. https://doi.org/10.1002/nau.20183.
https://doi.org/10.1002/nau.20183...
-3939. Ithamar L, de Moura Filho AG, Benedetti Rodrigues MA, Duque Cortez KC, Machado VG, de Paiva Lima CRO, et al. Abdominal and pelvic floor electromyographic analysis during abdominal hypopressive gymnastics. J Bodyw Mov Ther. 2018;22(1):159-65. https://doi.org/10.1016/j.jbmt.2017.06.011.
https://doi.org/10.1016/j.jbmt.2017.06.0...
) measured the contraction by EMG, four studies (2222. Tajiri K, Huo M, Maruyama H. Effects of Co-contraction of Both Transverse Abdominal Muscle and Pelvic Floor Muscle Exercises for Stress Urinary Incontinence: A Randomized Controlled Trial. J Phys Ther Sci. 2014;26(8):1161-3. https://doi.org/10.1589/jpts.26.1161.
https://doi.org/10.1589/jpts.26.1161...
,2424. Arab AM, Chehrehrazi M. The response of the abdominal muscles to pelvic floor muscle contraction in women with and without stress urinary incontinence using ultrasound imaging. Neurourol Urodyn. 2011;30(1):117-20. https://doi.org/10.1002/nau.20959.
https://doi.org/10.1002/nau.20959...
,2727. Bø K, Braekken IH, Majida M, Engh ME. Constriction of the levator hiatus during instruction of pelvic floor or transversus abdominis contraction: a 4D ultrasound study. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(1):27-32. https://doi.org/10.1007/s00192-008-0719-3.
https://doi.org/10.1007/s00192-008-0719-...
,3636. Tajiri K, Huo M, Yin K, Fujisawa S, Maruyama H. An approach to assessment of female urinary incontinence risk using the thickness of the transverse abdominal muscle during co-contraction of both the transverse abdominal muscle and the pelvic floor muscle. J Phys Ther Sci. 2011;23(1):45-8. https://doi.org/10.1589/jpts.23.45.
https://doi.org/10.1589/jpts.23.45...
) measured the contraction by US, and one study (2929. Devreese A, Staes F, De Weerdt W, Feys H, Van Assche A, Penninckx F, et al. Clinical evaluation of pelvic floor muscle function in continent and incontinent women. Neurourol Urodyn. 2004;23(3):190-7. https://doi.org/10.1002/nau.20018.
https://doi.org/10.1002/nau.20018...
) measured the contraction by visual inspection and digital palpation scale (Table 2).
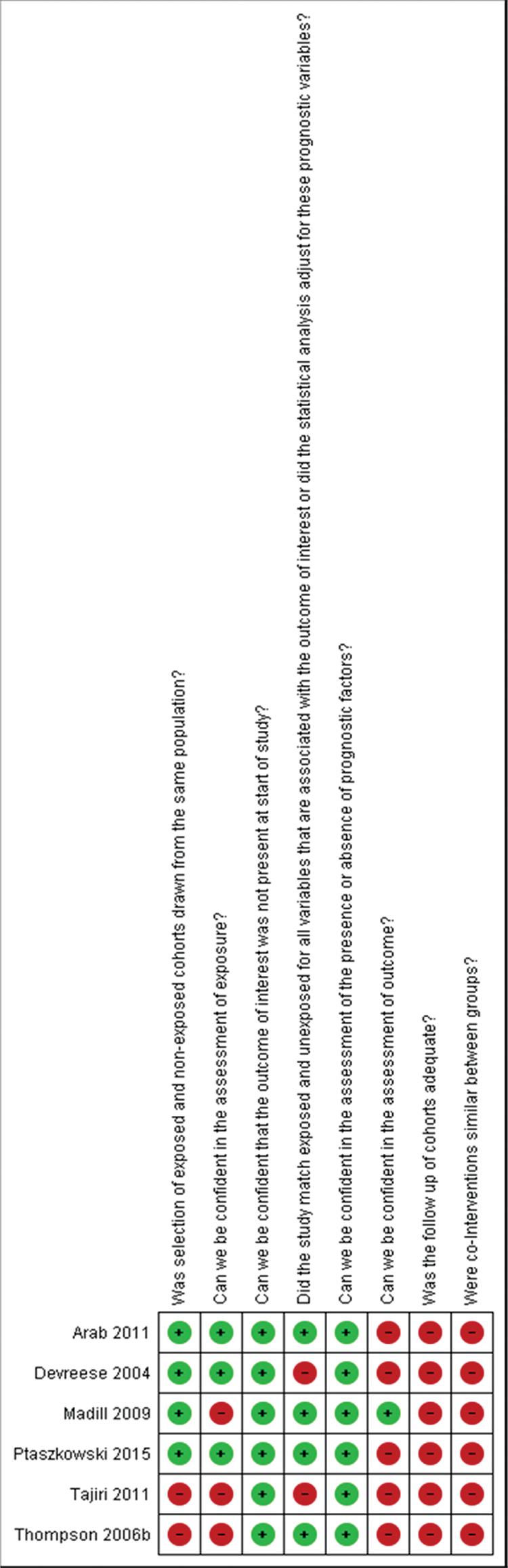
Risk of bias assessment
Figure 2 describes the risk of bias summary of the studies that compared two groups. Six observational studies compared women with and without PFD. The main problems with the studies were follow-up (2424. Arab AM, Chehrehrazi M. The response of the abdominal muscles to pelvic floor muscle contraction in women with and without stress urinary incontinence using ultrasound imaging. Neurourol Urodyn. 2011;30(1):117-20. https://doi.org/10.1002/nau.20959.
https://doi.org/10.1002/nau.20959...
,2929. Devreese A, Staes F, De Weerdt W, Feys H, Van Assche A, Penninckx F, et al. Clinical evaluation of pelvic floor muscle function in continent and incontinent women. Neurourol Urodyn. 2004;23(3):190-7. https://doi.org/10.1002/nau.20018.
https://doi.org/10.1002/nau.20018...
,3131. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
,3434. Ptaszkowski K, Paprocka-Borowicz M, Slupska L, Bartnicki J, Dymarek R, Rosinczuk J, et al. Assessment of bioelectrical activity of synergistic muscles during pelvic floor muscles activation in postmenopausal women with and without stress urinary incontinence: a preliminary observational study. Clin Interv Aging. 2015;10:1521-8. https://doi.org/10.2147/CIA.S89852.
https://doi.org/10.2147/CIA.S89852...
,3636. Tajiri K, Huo M, Yin K, Fujisawa S, Maruyama H. An approach to assessment of female urinary incontinence risk using the thickness of the transverse abdominal muscle during co-contraction of both the transverse abdominal muscle and the pelvic floor muscle. J Phys Ther Sci. 2011;23(1):45-8. https://doi.org/10.1589/jpts.23.45.
https://doi.org/10.1589/jpts.23.45...
,3838. Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Altered muscle activation patterns in symptomatic women during pelvic floor muscle contraction and Valsalva manouevre. Neurourol Urodyn. 2006;25(3):268-76. https://doi.org/10.1002/nau.20183.
https://doi.org/10.1002/nau.20183...
), information regarding cointerventions (2424. Arab AM, Chehrehrazi M. The response of the abdominal muscles to pelvic floor muscle contraction in women with and without stress urinary incontinence using ultrasound imaging. Neurourol Urodyn. 2011;30(1):117-20. https://doi.org/10.1002/nau.20959.
https://doi.org/10.1002/nau.20959...
,2929. Devreese A, Staes F, De Weerdt W, Feys H, Van Assche A, Penninckx F, et al. Clinical evaluation of pelvic floor muscle function in continent and incontinent women. Neurourol Urodyn. 2004;23(3):190-7. https://doi.org/10.1002/nau.20018.
https://doi.org/10.1002/nau.20018...
,3131. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
,3434. Ptaszkowski K, Paprocka-Borowicz M, Slupska L, Bartnicki J, Dymarek R, Rosinczuk J, et al. Assessment of bioelectrical activity of synergistic muscles during pelvic floor muscles activation in postmenopausal women with and without stress urinary incontinence: a preliminary observational study. Clin Interv Aging. 2015;10:1521-8. https://doi.org/10.2147/CIA.S89852.
https://doi.org/10.2147/CIA.S89852...
,3636. Tajiri K, Huo M, Yin K, Fujisawa S, Maruyama H. An approach to assessment of female urinary incontinence risk using the thickness of the transverse abdominal muscle during co-contraction of both the transverse abdominal muscle and the pelvic floor muscle. J Phys Ther Sci. 2011;23(1):45-8. https://doi.org/10.1589/jpts.23.45.
https://doi.org/10.1589/jpts.23.45...
,3838. Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Altered muscle activation patterns in symptomatic women during pelvic floor muscle contraction and Valsalva manouevre. Neurourol Urodyn. 2006;25(3):268-76. https://doi.org/10.1002/nau.20183.
https://doi.org/10.1002/nau.20183...
), assessment of outcome (2424. Arab AM, Chehrehrazi M. The response of the abdominal muscles to pelvic floor muscle contraction in women with and without stress urinary incontinence using ultrasound imaging. Neurourol Urodyn. 2011;30(1):117-20. https://doi.org/10.1002/nau.20959.
https://doi.org/10.1002/nau.20959...
,2929. Devreese A, Staes F, De Weerdt W, Feys H, Van Assche A, Penninckx F, et al. Clinical evaluation of pelvic floor muscle function in continent and incontinent women. Neurourol Urodyn. 2004;23(3):190-7. https://doi.org/10.1002/nau.20018.
https://doi.org/10.1002/nau.20018...
,3434. Ptaszkowski K, Paprocka-Borowicz M, Slupska L, Bartnicki J, Dymarek R, Rosinczuk J, et al. Assessment of bioelectrical activity of synergistic muscles during pelvic floor muscles activation in postmenopausal women with and without stress urinary incontinence: a preliminary observational study. Clin Interv Aging. 2015;10:1521-8. https://doi.org/10.2147/CIA.S89852.
https://doi.org/10.2147/CIA.S89852...
,3636. Tajiri K, Huo M, Yin K, Fujisawa S, Maruyama H. An approach to assessment of female urinary incontinence risk using the thickness of the transverse abdominal muscle during co-contraction of both the transverse abdominal muscle and the pelvic floor muscle. J Phys Ther Sci. 2011;23(1):45-8. https://doi.org/10.1589/jpts.23.45.
https://doi.org/10.1589/jpts.23.45...
,3838. Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Altered muscle activation patterns in symptomatic women during pelvic floor muscle contraction and Valsalva manouevre. Neurourol Urodyn. 2006;25(3):268-76. https://doi.org/10.1002/nau.20183.
https://doi.org/10.1002/nau.20183...
) and exposure (3131. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
,3636. Tajiri K, Huo M, Yin K, Fujisawa S, Maruyama H. An approach to assessment of female urinary incontinence risk using the thickness of the transverse abdominal muscle during co-contraction of both the transverse abdominal muscle and the pelvic floor muscle. J Phys Ther Sci. 2011;23(1):45-8. https://doi.org/10.1589/jpts.23.45.
https://doi.org/10.1589/jpts.23.45...
,3838. Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Altered muscle activation patterns in symptomatic women during pelvic floor muscle contraction and Valsalva manouevre. Neurourol Urodyn. 2006;25(3):268-76. https://doi.org/10.1002/nau.20183.
https://doi.org/10.1002/nau.20183...
). Table 3 details the description for each study.
Risk of bias assessment. We considered “probably high risk of bias” as “definitely high risk of bias” (red color) and “probably low risk of bias” as “definitely low risk of bias” (green color).
Outcomes
Meta-analysis of TrA muscle cocontraction when the PFMs contract
The results from two studies (2424. Arab AM, Chehrehrazi M. The response of the abdominal muscles to pelvic floor muscle contraction in women with and without stress urinary incontinence using ultrasound imaging. Neurourol Urodyn. 2011;30(1):117-20. https://doi.org/10.1002/nau.20959.
https://doi.org/10.1002/nau.20959...
,3636. Tajiri K, Huo M, Yin K, Fujisawa S, Maruyama H. An approach to assessment of female urinary incontinence risk using the thickness of the transverse abdominal muscle during co-contraction of both the transverse abdominal muscle and the pelvic floor muscle. J Phys Ther Sci. 2011;23(1):45-8. https://doi.org/10.1589/jpts.23.45.
https://doi.org/10.1589/jpts.23.45...
) with a total of 52 participants assessing cocontraction by US failed to show a difference in the cocontraction of the TrA in women with and without PFD (SMD −0.61 [95% CI −1.41 to 0.20], p=0.14; I2= 41%) (Figure 3). However, a plausible sensitivity analysis, excluding the study of Arab et al. (2424. Arab AM, Chehrehrazi M. The response of the abdominal muscles to pelvic floor muscle contraction in women with and without stress urinary incontinence using ultrasound imaging. Neurourol Urodyn. 2011;30(1):117-20. https://doi.org/10.1002/nau.20959.
https://doi.org/10.1002/nau.20959...
), yielded results that were inconsistent with the primary analysis, showing higher coactivity of the TrA during MVC of the PFMs in women without PFD (SMD −1.02 [95% CI −1.90 to −0.14], p=0.02; I2= not applicable) (Figure 4).
Forest plot showing the co-activity of the transversus abdominis, rectus abdominis, obliquus internus and obliquus externus muscles during maximal pelvic floor muscle contraction. CI = Confidence interval; PFD = Pelvic floor dysfunction.
Sensitivity analysis of co-activity of transversus abdominis (without the Arab et al. 2011 study), rectus abdominis (without the Madill et al. (31)), obliquus internus (without the Madill et al. (31)) and obliquus externus (without the Madill et al. (31)) muscles when the pelvic floor muscles contract. CI = Confidence interval; PFD = Pelvic floor dysfunction.
Certainty evidence was rated down to low because of serious limitations on the high risk of bias, indirectness due to the evaluation of only one PFD (UI) (Figure 3) and different ages, as well as imprecision (Table 4).
Meta-analysis of RA muscle cocontraction when the PFMs contract
The results from three studies (3131. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
,3434. Ptaszkowski K, Paprocka-Borowicz M, Slupska L, Bartnicki J, Dymarek R, Rosinczuk J, et al. Assessment of bioelectrical activity of synergistic muscles during pelvic floor muscles activation in postmenopausal women with and without stress urinary incontinence: a preliminary observational study. Clin Interv Aging. 2015;10:1521-8. https://doi.org/10.2147/CIA.S89852.
https://doi.org/10.2147/CIA.S89852...
,3838. Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Altered muscle activation patterns in symptomatic women during pelvic floor muscle contraction and Valsalva manouevre. Neurourol Urodyn. 2006;25(3):268-76. https://doi.org/10.1002/nau.20183.
https://doi.org/10.1002/nau.20183...
) with a total of 128 participants were unable to demonstrate a difference in the cocontraction of the RA between women with a normal pelvic floor and women with PFD (UI) (SMD −2.05 [95% CI −6.51 to 2.42], P=0.37; I2= 98%) (Figure 3). Furthermore, the sensitivity analysis, excluding the Madill et al. study (3131. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
), showed results that were inconsistent with the primary analysis, with higher cocontraction of the RA during MVC of the PFMs in women with PFD, however, with no statistical significance (SMD 0.89 [95% CI -0.03 to 1.82], P=0.06; I2= 63%) (Figure 4).
Certainty of evidence was rated down to very low because of serious limitations on the high risk of bias, inconsistency due to high heterogeneity (Figure 3), indirectness due to evaluation of only one PFD (UI), different assessments of UI and different ages, and imprecision (Table 4).
Meta-analysis of OI abdominis muscle cocontraction when the PFMs contract
The results from three studies (2424. Arab AM, Chehrehrazi M. The response of the abdominal muscles to pelvic floor muscle contraction in women with and without stress urinary incontinence using ultrasound imaging. Neurourol Urodyn. 2011;30(1):117-20. https://doi.org/10.1002/nau.20959.
https://doi.org/10.1002/nau.20959...
,3131. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
,3838. Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Altered muscle activation patterns in symptomatic women during pelvic floor muscle contraction and Valsalva manouevre. Neurourol Urodyn. 2006;25(3):268-76. https://doi.org/10.1002/nau.20183.
https://doi.org/10.1002/nau.20183...
) with a total of 118 participants showed no difference between women with a normal pelvic floor and women with PFD (UI) (SMD −0.47 [95% CI −2.38 to 1.44], I2= 95%; P=0.63) (Figure 3). However, a plausible sensitivity analysis, excluding the studies of Madill et al. (3131. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
) and Arab et al. (2424. Arab AM, Chehrehrazi M. The response of the abdominal muscles to pelvic floor muscle contraction in women with and without stress urinary incontinence using ultrasound imaging. Neurourol Urodyn. 2011;30(1):117-20. https://doi.org/10.1002/nau.20959.
https://doi.org/10.1002/nau.20959...
), presented results that were inconsistent with the primary analysis, showing a higher mean of cocontraction in women with PFD (UI) than in women with a normal pelvic floor (SMD 1.10 [95% CI 0.27 to 1.94], P=0.01; I2= not applicable) (Figure 4).
Certainty of evidence was rated down to very low because of serious limitations on inconsistency due to high risk of bias, high heterogeneity (Figure 3), indirectness due to the evaluation of only one PFD (UI), different assessments of UI and different ages, and imprecision (Table 4).
Meta-analysis of OE abdominis muscle cocontraction when the PFMs contract
The results from two studies (3131. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
,3838. Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Altered muscle activation patterns in symptomatic women during pelvic floor muscle contraction and Valsalva manouevre. Neurourol Urodyn. 2006;25(3):268-76. https://doi.org/10.1002/nau.20183.
https://doi.org/10.1002/nau.20183...
) with a total of 98 participants failed to show a difference between women with a normal pelvic floor and women with PFD (SMD 0.01 [95% CI −4.00 to 4.03], P=1.00; I2= 98%) (Figure 3). However, a plausible sensitivity analysis, excluding the study of Madill et al. (3131. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
), demonstrated results that were inconsistent with the primary analysis, showing a higher mean of cocontraction in women with PFD (UI) than in women with a normal pelvic floor (SMD 2.08 [95% CI 1.10 to 3.06], P<0.0001; I2= not applicable) (Figure 4).
Certainty of evidence was rated down to very low because of serious limitations on inconsistency due to high heterogeneity (Figure 3), indirectness due to high risk of bias, evaluation of only one PFD (UI), different assessments of UI and different ages, and imprecision (Table 4).
DISCUSSION
Main findings
This systematic review that investigated the cocontraction of AbMs and PFMs in women with or without PFD identified 20 studies. Therefore, it might provide evidence of synergism between PFMs and the TrA, RA, OI and OE, i.e., the cocontraction of PFMs and AbMs occurs during both voluntary contraction of the pelvic floor and abdominal muscle contractions. The studies showed a cocontraction of AbMs during the contraction of PFMs in women with no history of symptoms of PFD, with PFD, or both. Meta-analysis of data from five cross-sectional studies assessed the synergism of the TrA, RA, OI, and OE during MVC of PFMs. As the primary meta-analysis failed to show any difference between women with and without PFD, we performed a sensitivity analysis to minimize the heterogeneity of data. Our sensitivity analysis showed a different cocontraction pattern according to the four AbMs considered. The cocontraction between the TrA and PFMs in asymptomatic women showed a higher activation than that in symptomatic women. However, compared to women without PFD, women with PFD, such as UI, demonstrated an increased cocontraction of AbMs (RA, OI, and OE), suggesting an altered mechanism.
One study (2424. Arab AM, Chehrehrazi M. The response of the abdominal muscles to pelvic floor muscle contraction in women with and without stress urinary incontinence using ultrasound imaging. Neurourol Urodyn. 2011;30(1):117-20. https://doi.org/10.1002/nau.20959.
https://doi.org/10.1002/nau.20959...
) was excluded for a sensitivity analysis on the cocontraction of the TrA and OI because it did not report the position of women during the measurement. Additionally, as prior to the testing, the participants were trained until the correct performance of PFM contraction, we believe that such training before the measurement may have affected the data provided. Furthermore, another study (3131. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
) was not included in a sensitivity analysis of RA, OI, and OE. Although this study had the highest sample size, women with PFD were classified as having mild or severe UI, according to the severity of urine leakage. Moreover, the EMG data provided were smoothed by computing the root mean square. In this sensitivity analysis of RA, the I2 value, previously at 100%, was reduced to 0% when this study (3131. Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y.
https://doi.org/10.1007/s00192-008-0800-...
) was removed. Moreover, the results from the sensitivity analysis in OI and OE reached statistical significance favoring the PFD group.
Strengths and limitations
The strengths of our study include our unique analysis of the influence of each of the four muscles from the abdominal wall during maximal and submaximal contraction of PFMs. Additionally, we have provided evidence of a different synergism between AbMs and PFMs in women with and without PFD.
The primary limitation of our review is the low evidence because of study limitations. We identified a small number of studies with a small number of participants, resulting in high CIs; therefore, these findings should be carefully interpreted. EMG results should be cautiously interpreted because most studies used surface electrodes, which may contaminate data and distort their interpretation because of the surrounding muscles (4040. Kong YK, Hallbeck MS, Jung MC. Crosstalk effect on surface electromyogram of the forearm flexors during a static grip task. J Electromyogr Kinesiol. 2010;20(6):1223-9. https://doi.org/10.1016/j.jelekin.2010.08.001.
https://doi.org/10.1016/j.jelekin.2010.0...
). Additionally, the data processing of EMG studies widely differs, mostly in the position of the electrodes, the position of evaluation, and the type of data normalization.
Another limitation of this review was the insufficient number of included studies; we were not able to perform the complete statistical analysis. Furthermore, publication bias was not assessed because there were <10 eligible studies for each outcome in the meta-analysis (1616. Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from: http://www.handbook.cochrane.org.
http://www.handbook.cochrane.org...
).
Relation to prior work
Although previous systematic reviews have shown evidence of cocontraction between PFMs and AbMs (4141. Bo K, Morkved S, Frawley H, Sherburn M. Evidence for benefit of transversus abdominis training alone or in combination with pelvic floor muscle training to treat female urinary incontinence: A systematic review. Neurourol Urodyn. 2009;28(5):368-73. https://doi.org/10.1002/nau.20700.
https://doi.org/10.1002/nau.20700...
,4242. Ferla L, Darski C, Paiva LL, Sbruzzi G, Vieira A. Synergism between abdominal and pelvic floor muscles in healthy women: a systematic review of observational studies. Fisioter Mov. 2016;29(2):399-410. https://doi.org/10.1590/0103-5150.029.002.AO19.
https://doi.org/10.1590/0103-5150.029.00...
), investigators had not previously conducted a comparison between women with a normal pelvic floor and those with PFD involving all four muscles of the abdominal wall (TrA, RA, OI, and OE). Furthermore, to our knowledge, there is no published meta-analysis of the cocontraction between PFMs and the four AbMs.
The first systematic review related to this theme focused only on the combined training of the TrA and PFMs to treat UI and included five studies (4141. Bo K, Morkved S, Frawley H, Sherburn M. Evidence for benefit of transversus abdominis training alone or in combination with pelvic floor muscle training to treat female urinary incontinence: A systematic review. Neurourol Urodyn. 2009;28(5):368-73. https://doi.org/10.1002/nau.20700.
https://doi.org/10.1002/nau.20700...
). Another previous systematic review focused only on healthy women and included ten studies (4242. Ferla L, Darski C, Paiva LL, Sbruzzi G, Vieira A. Synergism between abdominal and pelvic floor muscles in healthy women: a systematic review of observational studies. Fisioter Mov. 2016;29(2):399-410. https://doi.org/10.1590/0103-5150.029.002.AO19.
https://doi.org/10.1590/0103-5150.029.00...
). In contrast, our search found 20 studies, and only five could be included in the meta-analyses. Our much larger analyses, including 468 women, more precisely elucidated the biomechanics of the communication between the abdominopelvic muscles in both the normal pelvic floor and PFD. Furthermore, we have also been able to detect the influence of each of the four muscles of the abdominal wall in PFM contraction.
Implications
PFD is very common among women worldwide and has become an increasing socioeconomic problem with prejudicial public health consequences, including symptoms that could lead to a significant decrease in quality of life and disability (4343. Abrams P, Smith AP, Cotterill N. The impact of urinary incontinence on health-related quality of life (HRQoL) in a real-world population of women aged 45-60 years: results from a survey in France, Germany, the UK and the USA. BJU Int. 2015;115(1):143-52. https://doi.org/10.1111/bju.12852.
https://doi.org/10.1111/bju.12852...
). While the prevalence of PFD is high, many factors involved in PFD are often poorly recognized or understood. Knowing the pathways related to PFD in detail is a main goal facilitating the identification of tools to prevent or correct these disorders (4444. Berghmans B, Nieman F, Leue C, Weemhoff M, Breukink S, van Koeveringe G. Prevalence and triage of first-contact complaints on pelvic floor dysfunctions in female patients at a Pelvic Care Centre. Neurourol Urodyn. 2016;35(4):503-8. https://doi.org/10.1002/nau.22739.
https://doi.org/10.1002/nau.22739...
). Our findings suggest a mechanism of PFD that is related to changes in the biomechanics caused by the increased AbM activation strength or by recruitment timing activation associated with different coactivity mechanisms according to the AbMs and PFMs.
In our view, there is a plausible biomechanical explanation to support higher coactivation levels of AbMs during MVC of PFMs. The coactivation between the TrA and PFMs showed a higher activation in asymptomatic women than in symptomatic women. However, the pattern of activation of the other AbMs differs with respect to time and strength in symptomatic women. During muscle contraction in PFD, there is a rapid and stronger coactivity of the RA, OI, and OE. The stronger coactivity of these AbMs could cause an increase in intra-abdominal pressure that, added to the insufficient PFM contraction, would increase the PFD.
Pereira et al. (4545. Pereira LC, Botelho S, Marques J, Amorim CF, Lanza AH, Palma P, et al. Are transversus abdominis/oblique internal and pelvic floor muscles coactivated during pregnancy and postpartum? Neurourol Urodyn. 2013;32(5):416-9. https://doi.org/10.1002/nau.22315.
https://doi.org/10.1002/nau.22315...
) proposed a theory explaining the synergism between the TrA and PFM. The abdominopelvic cavity has a static function of containment of the viscera and interacts with the PFMs. The fibers from the TrA are prolonged by the transverse perineal muscle because these muscles belong to the same muscle chain. This is an important conclusion for rehabilitation therapy, since numerous studies focus only on TrA strengthening to induce greater contractile strength of PFMs (2222. Tajiri K, Huo M, Maruyama H. Effects of Co-contraction of Both Transverse Abdominal Muscle and Pelvic Floor Muscle Exercises for Stress Urinary Incontinence: A Randomized Controlled Trial. J Phys Ther Sci. 2014;26(8):1161-3. https://doi.org/10.1589/jpts.26.1161.
https://doi.org/10.1589/jpts.26.1161...
,2727. Bø K, Braekken IH, Majida M, Engh ME. Constriction of the levator hiatus during instruction of pelvic floor or transversus abdominis contraction: a 4D ultrasound study. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(1):27-32. https://doi.org/10.1007/s00192-008-0719-3.
https://doi.org/10.1007/s00192-008-0719-...
,3535. Stupp L, Resende AP, Petricelli CD, Nakamura MU, Alexandre SM, Zanetti MR. Pelvic floor muscle and transversus abdominis activation in abdominal hypopressive technique through surface electromyography. Neurourol Urodyn. 2011;30(8):1518-21. https://doi.org/10.1002/nau.21151.
https://doi.org/10.1002/nau.21151...
,3636. Tajiri K, Huo M, Yin K, Fujisawa S, Maruyama H. An approach to assessment of female urinary incontinence risk using the thickness of the transverse abdominal muscle during co-contraction of both the transverse abdominal muscle and the pelvic floor muscle. J Phys Ther Sci. 2011;23(1):45-8. https://doi.org/10.1589/jpts.23.45.
https://doi.org/10.1589/jpts.23.45...
). Knowledge of the synergism among PFMs and AbMs may be useful for assessing PFMs and teaching women how to perform PFM exercises.
Our results show a synergism between AbMs and PFMs in women with and without PFD in different positions of evaluation. However, the studies included in this review had no standardized methods for selecting the participants, sample size, EMG, and US measurement, which limits the reliability of the findings. Very low-quality evidence suggests an association between the cocontraction of the AbMs when PFMs contract either in women with a normal pelvic floor or in women with PFD and should be interpreted with caution. Further research is needed to provide a better understanding of the cocontraction between the PFMs and AbMs.
APPENDIX
ACKNOWLEDGMENTS
This study was supported by grants from FAPESP/Brazil (#2016/09710-9). Giovana Vesentini received a Brazilian Research Council (FAPESP) scholarship (#2014/26852-6). Regina El Dib received a Brazilian Research Council (CNPq) scholarship (#310953/2015-4). Marilza Vieira Cunha Rudge received a Brazilian Research Council (CNPq) scholarship (#302284/2014-1). We thank Vinicius Sepúlveda for his help with the WebPlotDigitizer® (v. 3.8) for Windows.
REFERENCES
-
1Bo K, Frawley HC, Haylen BT, Abramov Y, Almeida FG, Berghmans B, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Int Urogynecol J. 2017;28(2):191-213. https://doi.org/10.1007/s00192-016-3123-4
» https://doi.org/10.1007/s00192-016-3123-4 -
2Chong EC, Khan AA, Anger JT. The financial burden of stress urinary incontinence among women in the United States. Curr Urol Rep. 2011;12(5):358-62. https://doi.org/10.1007/s11934-011-0209-x
» https://doi.org/10.1007/s11934-011-0209-x -
3Bump RC, Norton PA. Epidemiology and natural history of pelvic floor dysfunction. Obstet Gynecol Clin North Am. 1998;25(4):723-46. https://doi.org/10.1016/S0889-8545(05)70039-5
» https://doi.org/10.1016/S0889-8545(05)70039-5 -
4Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, et al. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet Gynecol. 2014;123(1):141-8. https://doi.org/10.1097/AOG.0000000000000057
» https://doi.org/10.1097/AOG.0000000000000057 -
5Walker GJ, Gunasekera P. Pelvic organ prolapse and incontinence in developing countries: review of prevalence and risk factors. Int Urogynecol J. 2011;22(2):127-35. https://doi.org/10.1007/s00192-010-1215-0
» https://doi.org/10.1007/s00192-010-1215-0 -
6Sapsford RR, Hodges PW. Contraction of the pelvic floor muscles during abdominal maneuvers. Arch Phys Med Rehabil. 2001;82(8):1081-8. https://doi.org/10.1053/apmr.2001.24297
» https://doi.org/10.1053/apmr.2001.24297 -
7Sapsford R. The Pelvic Floor: A clinical model for function and rehabilitation. Physiotherapy. 2001;87(12):620-30. https://doi.org/10.1016/S0031-9406(05)61107-8
» https://doi.org/10.1016/S0031-9406(05)61107-8 -
8Sapsford RR, Hodges PW, Richardson CA, Cooper DH, Markwell SJ, Jull GA. Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neurourol Urodyn. 2001;20(1):31-42. https://doi.org/10.1002/1520-6777(2001)20:1<31::AID-NAU5>3.0.CO;2-P
» https://doi.org/10.1002/1520-6777(2001)20:1<31::AID-NAU5>3.0.CO;2-P -
9Madill SJ, McLean L. Relationship between abdominal and pelvic floor muscle activation and intravaginal pressure during pelvic floor muscle contractions in healthy continent women. Neurourol Urodyn. 2006;25(7):722-30. https://doi.org/10.1002/nau.20285
» https://doi.org/10.1002/nau.20285 -
10Nambiar AK, Bosch R, Cruz F, Lemack GE, Thiruchelvam N, Tubaro A, et al. EAU Guidelines on Assessment and Nonsurgical Management of Urinary Incontinence. Eur Urol. 2018;73(4):596-609. https://doi.org/10.1016/j.eururo.2017.12.031
» https://doi.org/10.1016/j.eururo.2017.12.031 -
11Qaseem A, Dallas P, Forciea MA, Starkey M, Denberg TD, Shekelle P, et al. Nonsurgical management of urinary incontinence in women: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2014;161(6):429-40. https://doi.org/10.7326/M13-2410
» https://doi.org/10.7326/M13-2410 -
12Sapsford R. Rehabilitation of pelvic floor muscles utilizing trunk stabilization. Man Ther. 2004;9(1):3-12. https://doi.org/10.1016/S1356-689X(03)00131-0
» https://doi.org/10.1016/S1356-689X(03)00131-0 -
13Bø K, Herbert RD. There is not yet strong evidence that exercise regimens other than pelvic floor muscle training can reduce stress urinary incontinence in women: a systematic review. J Physiother. 2013;59(3):159-68. https://doi.org/10.1016/S1836-9553(13)70180-2
» https://doi.org/10.1016/S1836-9553(13)70180-2 -
14Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264-9, W64. https://doi.org/10.7326/0003-4819-151-4-200908180-00135
» https://doi.org/10.7326/0003-4819-151-4-200908180-00135 -
15Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008-12. https://doi.org/10.1001/jama.283.15.2008
» https://doi.org/10.1001/jama.283.15.2008 -
16Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from: http://www.handbook.cochrane.org
» http://www.handbook.cochrane.org -
17Guyatt GH, Busse JW. Modification of Ottawa-Newcastle to assess risk of bias in nonrandomized trials. http://distillercer.com/resources/
» http://distillercer.com/resources/ -
18Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924-6. https://doi.org/10.1136/bmj.39489.470347.AD
» https://doi.org/10.1136/bmj.39489.470347.AD -
19Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence--imprecision. J Clin Epidemiol. 2011;64(12):1283-93. https://doi.org/10.1016/j.jclinepi.2011.01.012
» https://doi.org/10.1016/j.jclinepi.2011.01.012 -
20Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 7. Rating the quality of evidence--inconsistency. J Clin Epidemiol. 2011;64(12):1294-302. https://doi.org/10.1016/j.jclinepi.2011.03.017
» https://doi.org/10.1016/j.jclinepi.2011.03.017 -
21Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 8. Rating the quality of evidence--indirectness. J Clin Epidemiol. 2011;64(12):1303-10. https://doi.org/10.1016/j.jclinepi.2011.04.014
» https://doi.org/10.1016/j.jclinepi.2011.04.014 -
22Tajiri K, Huo M, Maruyama H. Effects of Co-contraction of Both Transverse Abdominal Muscle and Pelvic Floor Muscle Exercises for Stress Urinary Incontinence: A Randomized Controlled Trial. J Phys Ther Sci. 2014;26(8):1161-3. https://doi.org/10.1589/jpts.26.1161
» https://doi.org/10.1589/jpts.26.1161 -
23Silva VR, Riccetto CL, Martinho NM, Marques J, Carvalho LC, Botelho S. Training through gametherapy promotes coactivation of the pelvic floor and abdominal muscles in young women, nulliparous and continents. Int Braz J Urol. 2016;42(4):779-86. https://doi.org/10.1590/S1677-5538.IBJU.2014.0580
» https://doi.org/10.1590/S1677-5538.IBJU.2014.0580 -
24Arab AM, Chehrehrazi M. The response of the abdominal muscles to pelvic floor muscle contraction in women with and without stress urinary incontinence using ultrasound imaging. Neurourol Urodyn. 2011;30(1):117-20. https://doi.org/10.1002/nau.20959
» https://doi.org/10.1002/nau.20959 -
25Bø K, Stien R. Needle EMG registration of striated urethral wall and pelvic floor muscle activity patterns during cough, Valsalva, abdominal, hip adductor, and gluteal muscle contractions in nulliparous healthy females. Neurourol Urodyn. 1994;13(1):35-41. https://doi.org/10.1002/nau.1930130106
» https://doi.org/10.1002/nau.1930130106 -
26Bø K, Kvarstein B, Hagen RR, Larsen S. Pelvic floor muscle exercise for the treatment of female stress urinary incontinence: II. Validity of vaginal pressure measurements of pelvic floor muscle strength and the necessity of supplementary methods of control of correct contraction. Neurourol Urodyn. 1990;9:479-87. https://doi.org/10.1002/nau.1930090504
» https://doi.org/10.1002/nau.1930090504 -
27Bø K, Braekken IH, Majida M, Engh ME. Constriction of the levator hiatus during instruction of pelvic floor or transversus abdominis contraction: a 4D ultrasound study. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(1):27-32. https://doi.org/10.1007/s00192-008-0719-3
» https://doi.org/10.1007/s00192-008-0719-3 -
28Chmielewska D, Stania M, Sobota G, Kwasna K, Blaszczak E, Taradaj J, et al. Impact of different body positions on bioelectrical activity of the pelvic floor muscles in nulliparous continent women. Biomed Res Int. 2015;2015:905897. https://doi.org/10.1155/2015/905897
» https://doi.org/10.1155/2015/905897 -
29Devreese A, Staes F, De Weerdt W, Feys H, Van Assche A, Penninckx F, et al. Clinical evaluation of pelvic floor muscle function in continent and incontinent women. Neurourol Urodyn. 2004;23(3):190-7. https://doi.org/10.1002/nau.20018
» https://doi.org/10.1002/nau.20018 -
30Junginger B, Baessler K, Sapsford R, Hodges PW. Effect of abdominal and pelvic floor tasks on muscle activity, abdominal pressure and bladder neck. Int Urogynecol J. 2010;21(1):69-77. https://doi.org/10.1007/s00192-009-0981-z
» https://doi.org/10.1007/s00192-009-0981-z -
31Madill SJ, Harvey MA, McLean L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4):447-59. https://doi.org/10.1007/s00192-008-0800-y
» https://doi.org/10.1007/s00192-008-0800-y -
32Madill SJ, McLean L. Quantification of abdominal and pelvic floor muscle synergies in response to voluntary pelvic floor muscle contractions. J Electromyogr Kinesiol. 2008;18(6):955-64. https://doi.org/10.1016/j.jelekin.2007.05.001
» https://doi.org/10.1016/j.jelekin.2007.05.001 -
33Neumann P, Gill V. Pelvic floor and abdominal muscle interaction: EMG activity and intra-abdominal pressure. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13(2):125-32. https://doi.org/10.1007/s001920200027
» https://doi.org/10.1007/s001920200027 -
34Ptaszkowski K, Paprocka-Borowicz M, Slupska L, Bartnicki J, Dymarek R, Rosinczuk J, et al. Assessment of bioelectrical activity of synergistic muscles during pelvic floor muscles activation in postmenopausal women with and without stress urinary incontinence: a preliminary observational study. Clin Interv Aging. 2015;10:1521-8. https://doi.org/10.2147/CIA.S89852
» https://doi.org/10.2147/CIA.S89852 -
35Stupp L, Resende AP, Petricelli CD, Nakamura MU, Alexandre SM, Zanetti MR. Pelvic floor muscle and transversus abdominis activation in abdominal hypopressive technique through surface electromyography. Neurourol Urodyn. 2011;30(8):1518-21. https://doi.org/10.1002/nau.21151
» https://doi.org/10.1002/nau.21151 -
36Tajiri K, Huo M, Yin K, Fujisawa S, Maruyama H. An approach to assessment of female urinary incontinence risk using the thickness of the transverse abdominal muscle during co-contraction of both the transverse abdominal muscle and the pelvic floor muscle. J Phys Ther Sci. 2011;23(1):45-8. https://doi.org/10.1589/jpts.23.45
» https://doi.org/10.1589/jpts.23.45 -
37Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Differences in muscle activation patterns during pelvic floor muscle contraction and Valsalva maneuver. Neurourol Urodyn. 2006;25(2):148-55. https://doi.org/10.1002/nau.20203
» https://doi.org/10.1002/nau.20203 -
38Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Altered muscle activation patterns in symptomatic women during pelvic floor muscle contraction and Valsalva manouevre. Neurourol Urodyn. 2006;25(3):268-76. https://doi.org/10.1002/nau.20183
» https://doi.org/10.1002/nau.20183 -
39Ithamar L, de Moura Filho AG, Benedetti Rodrigues MA, Duque Cortez KC, Machado VG, de Paiva Lima CRO, et al. Abdominal and pelvic floor electromyographic analysis during abdominal hypopressive gymnastics. J Bodyw Mov Ther. 2018;22(1):159-65. https://doi.org/10.1016/j.jbmt.2017.06.011
» https://doi.org/10.1016/j.jbmt.2017.06.011 -
40Kong YK, Hallbeck MS, Jung MC. Crosstalk effect on surface electromyogram of the forearm flexors during a static grip task. J Electromyogr Kinesiol. 2010;20(6):1223-9. https://doi.org/10.1016/j.jelekin.2010.08.001
» https://doi.org/10.1016/j.jelekin.2010.08.001 -
41Bo K, Morkved S, Frawley H, Sherburn M. Evidence for benefit of transversus abdominis training alone or in combination with pelvic floor muscle training to treat female urinary incontinence: A systematic review. Neurourol Urodyn. 2009;28(5):368-73. https://doi.org/10.1002/nau.20700
» https://doi.org/10.1002/nau.20700 -
42Ferla L, Darski C, Paiva LL, Sbruzzi G, Vieira A. Synergism between abdominal and pelvic floor muscles in healthy women: a systematic review of observational studies. Fisioter Mov. 2016;29(2):399-410. https://doi.org/10.1590/0103-5150.029.002.AO19
» https://doi.org/10.1590/0103-5150.029.002.AO19 -
43Abrams P, Smith AP, Cotterill N. The impact of urinary incontinence on health-related quality of life (HRQoL) in a real-world population of women aged 45-60 years: results from a survey in France, Germany, the UK and the USA. BJU Int. 2015;115(1):143-52. https://doi.org/10.1111/bju.12852
» https://doi.org/10.1111/bju.12852 -
44Berghmans B, Nieman F, Leue C, Weemhoff M, Breukink S, van Koeveringe G. Prevalence and triage of first-contact complaints on pelvic floor dysfunctions in female patients at a Pelvic Care Centre. Neurourol Urodyn. 2016;35(4):503-8. https://doi.org/10.1002/nau.22739
» https://doi.org/10.1002/nau.22739 -
45Pereira LC, Botelho S, Marques J, Amorim CF, Lanza AH, Palma P, et al. Are transversus abdominis/oblique internal and pelvic floor muscles coactivated during pregnancy and postpartum? Neurourol Urodyn. 2013;32(5):416-9. https://doi.org/10.1002/nau.22315
» https://doi.org/10.1002/nau.22315
Publication Dates
-
Publication in this collection
25 Nov 2019 -
Date of issue
2019
History
-
Received
30 Apr 2019 -
Accepted
4 Oct 2019