Abstract
Background
Cardiotoxicity is a documented complication of Crotalinae envenomation. Reported cardiac complications following snake envenomation have included acute myocardial infarction, electrocardiogram abnormalities and arrhythmias. Few reports exist describing arrhythmia induced by viper envenomation and to our knowledge none describe arrhythmia induced by Crotalinae envenomation. This report concerns the first known case of atrial fibrillation precipitated by rattlesnake bite.
Case presentation
A 73-year-old Caucasian man with a past medical history of hypertension, hyperlipidemia, type 1 diabetes mellitus, and a baseline first-degree atrioventricular block presented to the emergency department following a rattlesnake bite to his left lower leg. He developed pain and swelling in his left leg two-hour post-envenomation and subsequently received four vials of Crotalidae polyvalent immune fab (ovine). At three-hour post-envenomation following transfer to the intensive care unit, an electrocardiogram revealed new-onset atrial fibrillation. An amiodarone drip was started and the patient successfully converted to normal sinus rhythm approximately six hours after he was found to be in atrial fibrillation. A transthoracic echocardiogram revealed mild concentric left ventricular hypertrophy and an ejection fraction of 72%. He was discharged the following day with no hematological abnormalities and a baseline first-degree atrioventricular block.
Conclusion
This is the first documented case of reversible atrial fibrillation precipitated by Crotalinae envenomation. In patients with pertinent risk factors for developing atrial fibrillation, physicians should be aware of the potential for this arrhythmia. Direct toxic effects of venom or structural and electrophysiological cardiovascular abnormalities may predispose snakebite patients to arrhythmia, warranting extended and attentive cardiac monitoring.
Crotalidae; Rattlesnake; Bite; Envenomation; Snakebite; Atrial fibrillation
Background
Endemic to Asia and the Americas, the Viperidae subfamily of snakes known as Crotalinae is comprised of rattlesnakes, cottonmouths, and copperheads in North America; Bothrops in Central and South America; and the Asiatic pit vipers [11. Gutiérrez JM. Current challenges for confronting the public health problem of snakebite envenoming in Central America. J Venom Anim Toxins incl Trop Dis. 2014;20:7. doi:10.1186/1678-9199-20-7.>, 22. Chippaux JP. Epidemiology of envenomations by terrestrial venomous animals in Brazil based on case reporting: from obvious facts to contingencies. J Venom Anim Toxins incl Trop Dis. 2015;21:13. doi:10.1186/s40409-015-0011-1.>
https://doi.org/10.1186/s40409-015-0011-...
]. Clinical manifestations of Crotalinae envenomation often include local tissue reaction with systemic effects such as nausea, vomiting, diarrhea, diaphoresis, and weakness. Severe cases are characterized by coagulopathy with hemorrhagic manifestations, as well as renal failure [33. Gold BS, Barish RA, Dart RC. North American snake envenomation: diagnosis, treatment, and management. Emerg Med Clin North Am. 2004;22(2):423–43.]. While the potential nephrotoxic, myotoxic, and neurotoxic effects of Viperidae family snake venom are well documented, cardiotoxicity is infrequently described in the literature. Reported cardiac complications following snake envenomation have included acute myocardial infarction, electrocardiogram (ECG) abnormalities, and arrhythmias [44. Niraj M, Jayaweera JL, Kumara IW, Tissera NW. Acute myocardial infarction following a Russell’s viper bite: a case report. Int Arch Med. 2013;6:7.>, 55. Saadeh AM. Case report: acute myocardial infarction complicating a viper bite. Am J Trop Med Hyg. 2001;64(5–6):280–2., 66. Blondheim DS, Plich M, Berman M, Khair G, Tzvig L, Ezri J, et al. Acute myocardial infarction complicating viper bite. Am J Cardiol. 1996;78(4):492–3., 77. Persson H, Irestedt B. A study of 136 cases of adder bite treated in Swedish hospitals during one year. Acta Med Scand. 1981;210(6):433–9., 88. Reid HA, Thean PC, Chan KE, Baharom AR. Clinical effects of bites by Malayan viper (Ancistrodon rhodostoma). Lancet. 1963;1(7282):617–21., 99. Gaballa M, Taher T, Brodin LA, Linden J van der, O’Reilly K, Hui W, et al. Myocardial infarction as a rare consequence of a snakebite: diagnosis with novel echocardiographic tissue doppler techniques. Circulation. 2005;112(11):140–2., 1010. Nayak KC, Jain AK, Sharda DP, Mishra SN. Profile of cardiac complications of snake bite. Indian Heart J. 1990;42(3):185–8., 1111. Thewjitcharoen Y, Poopitaya S. Ventricular tachycardia, a rare manifestation of Russell’s viper bite: case report. J Med Assoc Thai. 2005;88(12):1931–3., 1212. Moore RS. Second-degree heart block associated with envenomation byVipera berus. Arch Emerg Med. 1988;5(2):116–8.>, 1313. Agarwal A, Kumar T, Ravindranath KS, Bhat P, Manjunath CN, Agarwal N. Sinus node dysfunction complicating viper bite. Asian Cardiovasc Thorac Ann. 2015;23(2):212–4., 1414. Karaye KM, Mijinyawa MS, Yakasai AM, Kwaghe V, Joseph GA, Iliyasu G, et al. Cardiac and hemodynamic features following snakebite in Nigeria. Int J Cardiol. 2012;156(3):326–8., 1515. Lalloo DG, Trevett AJ, Korinhona A, Nwokolo N, Laurenson IF, Paul M, et al. Snake bites by thePapuan taipan(Oxyuranus scutellatus canni): paralysis, hemostatic and electrocardiographic abnormalities, and effects of antivenom. Am J Trop Med Hyg. 1995;52(6):525–31., 1616. Gupta OP, Mewar SH, Kalantri SP, Jain AP, Jajoo UN. Reversible atrial fibrillation following snake bite. J Assoc Physicians India. 1987;35(7):535–6.]. Few reports exist describing arrhythmia induced by viper envenomation, and to our knowledge none describe arrhythmia induced by Crotalinae envenomation. This report concerns a case of atrial fibrillation (AF) precipitated by rattlesnake bite.
Case presentation
A 73-year-old Caucasian man presented to the emergency department following a rattlesnake bite to his left lower leg. The envenomation occurred 30 min prior to his arrival by ambulance while he was retrieving a golf ball at a local golf course. On presentation, the patient was alert, complained of pain localized to the left lower extremity, and denied having chest pain, palpitations or dyspnea. His past medical history included hypertension, hyperlipidemia and type 1 diabetes mellitus. Current medications included lisinopril, hydrochlorothiazide, atorvastatin, fluoxetine and insulin. On examination, two puncture wounds and mild swelling were noted anteriorly on the patient’s left lower leg.
An ECG taken approximately one hour after envenomation showed him to be in sinus rhythm with a rate of 87 beats per minute. Additionally, a PR interval of 220 ms was indicative of a baseline first-degree atrioventricular block (AVB). Initial laboratory tests indicated a number of abnormal values: WBC 11,000/μL (H), neutrophils 75.2% (H), lymphocytes 19.7% (L), D-dimer 0.55 μg/mL (H), glucose 222 mg/dL (H), BUN 34 mg/dL (H). The following laboratory values were in the normal range: platelets 312 × 103/μL, prothrombin time 12.9 s and fibrinogen 305 mg/dL.
Two hours post-envenomation the patient developed moderate swelling in his left calf and leg, tachycardia, nausea and diaphoresis. At that time, he was started on an initial dose of four vials of Crotalidae polyvalent immune fab (ovine) infused over one hour.
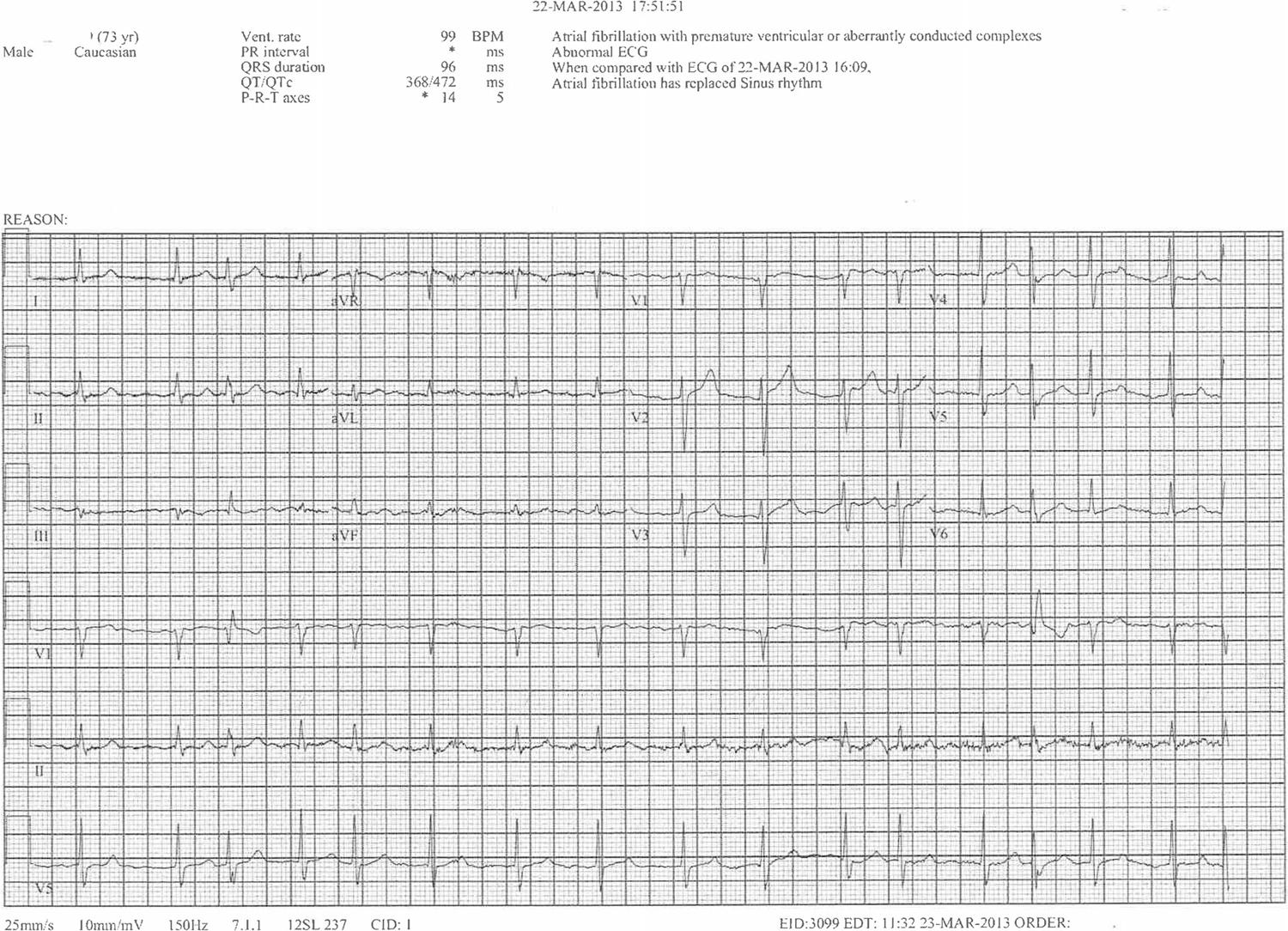
The patient was subsequently transferred to the ICU for monitoring, however an ECG taken three hours post-envenomation revealed new-onset AF (Fig. 1). Cardiology team was consulted and an amiodarone drip was started. The patient successfully converted to normal sinus rhythm approximately six hours after he was found to be in AF (Fig. 2). A first-degree AVB was still present at that time. A transthoracic echocardiogram was ordered by cardiology and revealed mild concentric left ventricular hypertrophy with normal systolic function and an ejection fraction of 72%. The patient denied use of any stimulants or sympathomimetic agents, as well as any family history of heart disease. TSH levels were within normal limits.
The patient’s blood sugar was markedly elevated during the first 24 h of hospitalization, and his insulin regimen was adjusted accordingly. No further antivenom was given as his swelling and laboratory tests were well controlled. Coagulation studies were monitored, and the patient continued to be stable for the rest of his hospitalization. His laboratory studies prior to discharge were stable. He was discharged the following day with ecchymosis around the ankle and wound site and instructions to have his blood work repeated at an outside laboratory.
Discussion
In 2014, over 3,000 Crotalinae envenomations were reported to the American Association of Poison Control Centers’ National Poison Data System. Of those envenomations, over 750 were attributed to rattlesnakes [1717. Mowry JB, Spyker DA, Brooks DE, McMillan N, Schauben JL. Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 32ndAnnual Report. Clin Toxicol. 2014;2015:962–1146.]. According to one Indian study assessing cardiac complications of snakebite, it is estimated that up to 25% of viper family envenomations result in cardiotoxicity [1010. Nayak KC, Jain AK, Sharda DP, Mishra SN. Profile of cardiac complications of snake bite. Indian Heart J. 1990;42(3):185–8.].
Cardiovascular manifestations of snakebite, particularly of the Viperidae family variety, are diverse. Reports of myocardial infarction and cardiac tamponade have been described in the literature, and ECG abnormalities such as T-wave inversion and QT prolongation have been seen in several cases [44. Niraj M, Jayaweera JL, Kumara IW, Tissera NW. Acute myocardial infarction following a Russell’s viper bite: a case report. Int Arch Med. 2013;6:7.>, 55. Saadeh AM. Case report: acute myocardial infarction complicating a viper bite. Am J Trop Med Hyg. 2001;64(5–6):280–2., 66. Blondheim DS, Plich M, Berman M, Khair G, Tzvig L, Ezri J, et al. Acute myocardial infarction complicating viper bite. Am J Cardiol. 1996;78(4):492–3., 77. Persson H, Irestedt B. A study of 136 cases of adder bite treated in Swedish hospitals during one year. Acta Med Scand. 1981;210(6):433–9., 88. Reid HA, Thean PC, Chan KE, Baharom AR. Clinical effects of bites by Malayan viper (Ancistrodon rhodostoma). Lancet. 1963;1(7282):617–21., 99. Gaballa M, Taher T, Brodin LA, Linden J van der, O’Reilly K, Hui W, et al. Myocardial infarction as a rare consequence of a snakebite: diagnosis with novel echocardiographic tissue doppler techniques. Circulation. 2005;112(11):140–2., 1010. Nayak KC, Jain AK, Sharda DP, Mishra SN. Profile of cardiac complications of snake bite. Indian Heart J. 1990;42(3):185–8., 1818. Senthikumaran S, Meenakshisundaram R, Thirumalaikolundusubramanian P. Cardiac tamponade in Russell viper (Daboia russelii) bite: case report with brief review. J Emerg Med. 2012;42(3):288–90.]. Arrhythmia is a rare complication of snakebite and has been described infrequently; reported arrhythmias following viper envenomation include ventricular tachycardia, torsades de pointes, second-degree AVB, and sinus arrest [99. Gaballa M, Taher T, Brodin LA, Linden J van der, O’Reilly K, Hui W, et al. Myocardial infarction as a rare consequence of a snakebite: diagnosis with novel echocardiographic tissue doppler techniques. Circulation. 2005;112(11):140–2., 1111. Thewjitcharoen Y, Poopitaya S. Ventricular tachycardia, a rare manifestation of Russell’s viper bite: case report. J Med Assoc Thai. 2005;88(12):1931–3., 1212. Moore RS. Second-degree heart block associated with envenomation byVipera berus. Arch Emerg Med. 1988;5(2):116–8.>, 1313. Agarwal A, Kumar T, Ravindranath KS, Bhat P, Manjunath CN, Agarwal N. Sinus node dysfunction complicating viper bite. Asian Cardiovasc Thorac Ann. 2015;23(2):212–4.]. In reports nonspecific to Crotalidae or Viperidae envenomation, cases of first-degree AVB, bundle branch block, atrial arrhythmias, complete heart block, sinus bradycardia or tachycardia, and various sinus arrhythmias have also been described [1010. Nayak KC, Jain AK, Sharda DP, Mishra SN. Profile of cardiac complications of snake bite. Indian Heart J. 1990;42(3):185–8., 1414. Karaye KM, Mijinyawa MS, Yakasai AM, Kwaghe V, Joseph GA, Iliyasu G, et al. Cardiac and hemodynamic features following snakebite in Nigeria. Int J Cardiol. 2012;156(3):326–8., 1515. Lalloo DG, Trevett AJ, Korinhona A, Nwokolo N, Laurenson IF, Paul M, et al. Snake bites by thePapuan taipan(Oxyuranus scutellatus canni): paralysis, hemostatic and electrocardiographic abnormalities, and effects of antivenom. Am J Trop Med Hyg. 1995;52(6):525–31.]. To our knowledge only one case of confirmed reversible AF following snakebite exists in the literature, however the species of snake was unknown [1616. Gupta OP, Mewar SH, Kalantri SP, Jain AP, Jajoo UN. Reversible atrial fibrillation following snake bite. J Assoc Physicians India. 1987;35(7):535–6.]. The exact mechanism responsible for snakebite-induced arrhythmia remains unclear.
Several theoretical factors may have contributed to the development of paroxysmal AF in our patient. Given his cardiovascular risk factors, a predisposition towards arrhythmia likely existed prior to envenomation. Advanced age, hyperlipidemia, long-standing type 1 diabetes mellitus and hypertension are established extracardiac predictors of AF [1919. Schnabel RB, Sullivan LM, Levy D, Pencina MJ, Massaro JM, D’AgostinoSrRB, et al. Development of a risk score for atrial fibrillation (Framingham Heart Study): a community-based cohort study. Lancet. 2009;373(9665):739–45.>]. Mild left ventricular hypertrophy, seen on this patient’s transthoracic echocardiogram and likely secondary to his underlying hypertension, is also associated with an increased risk [2020. Kannel WB, Abbott RD, Savage DD, McNamara PM. Epidemiologic features of chronic atrial fibrillation: the Framingham study. N Engl J Med. 1982;306(17):1018–22.].
Potential atrial electrical abnormalities may represent another mechanism behind this patient’s development of AF. In a 2014 retrospective study by Uhm et al. [2121. Uhm JS, Shim J, Wi J, Mun HS, Park J, Park SH, et al. First-degree atrioventricular block is associated with advanced atrioventricular block, atrial fibrillation and left ventricular dysfunction in patients with hypertension. J Hypertens. 2014;32(5):1115–20.], first-degree AVB was found to be an independent risk factor (hazard ratio 2.33) for development of AF. Autonomic nervous system activation and subsequent adrenergic stimulation following envenomation also could have triggered AF. Through several proposed electrophysiological mechanisms in the atrium, catecholamines have been shown to affect AF initiation and/or maintenance [2222. Workman AJ. Cardiac adrenergic control and atrial fibrillation. Naunyn Schmiedebergs Arch Pharmacol. 2010;381(3):235–49.].
Additionally, arrhythmia precipitated by direct toxicity to Crotalidae venom must be considered. Snake venom is believed to have a potential toxic effect on the myocardium, and may modify electrophysiological properties of the cardiac cell membrane [44. Niraj M, Jayaweera JL, Kumara IW, Tissera NW. Acute myocardial infarction following a Russell’s viper bite: a case report. Int Arch Med. 2013;6:7.>, 55. Saadeh AM. Case report: acute myocardial infarction complicating a viper bite. Am J Trop Med Hyg. 2001;64(5–6):280–2., 1111. Thewjitcharoen Y, Poopitaya S. Ventricular tachycardia, a rare manifestation of Russell’s viper bite: case report. J Med Assoc Thai. 2005;88(12):1931–3.]. This could potentially alter cardiac impulse generation and/or conduction; however, a mechanism remains to be determined.
Conclusion
This report describes the case of a 73-year-old man who developed reversible atrial fibrillation following Crotalinae envenomation. Although this is a rare presentation of snakebite, in patients with pertinent risk factors for developing AF, physicians should be aware of the potential for this arrhythmia. Direct toxic effects of venom or structural and electrophysiological abnormalities may predispose snakebite patients to arrhythmia, warranting extended and attentive cardiac monitoring.
Acknowledgments
Not applicable.
References
-
1Gutiérrez JM. Current challenges for confronting the public health problem of snakebite envenoming in Central America. J Venom Anim Toxins incl Trop Dis. 2014;20:7. doi:10.1186/1678-9199-20-7.>
-
2Chippaux JP. Epidemiology of envenomations by terrestrial venomous animals in Brazil based on case reporting: from obvious facts to contingencies. J Venom Anim Toxins incl Trop Dis. 2015;21:13. doi:10.1186/s40409-015-0011-1.>
» https://doi.org/10.1186/s40409-015-0011-1 -
3Gold BS, Barish RA, Dart RC. North American snake envenomation: diagnosis, treatment, and management. Emerg Med Clin North Am. 2004;22(2):423–43.
-
4Niraj M, Jayaweera JL, Kumara IW, Tissera NW. Acute myocardial infarction following a Russell’s viper bite: a case report. Int Arch Med. 2013;6:7.>
-
5Saadeh AM. Case report: acute myocardial infarction complicating a viper bite. Am J Trop Med Hyg. 2001;64(5–6):280–2.
-
6Blondheim DS, Plich M, Berman M, Khair G, Tzvig L, Ezri J, et al. Acute myocardial infarction complicating viper bite. Am J Cardiol. 1996;78(4):492–3.
-
7Persson H, Irestedt B. A study of 136 cases of adder bite treated in Swedish hospitals during one year. Acta Med Scand. 1981;210(6):433–9.
-
8Reid HA, Thean PC, Chan KE, Baharom AR. Clinical effects of bites by Malayan viper (Ancistrodon rhodostoma). Lancet. 1963;1(7282):617–21.
-
9Gaballa M, Taher T, Brodin LA, Linden J van der, O’Reilly K, Hui W, et al. Myocardial infarction as a rare consequence of a snakebite: diagnosis with novel echocardiographic tissue doppler techniques. Circulation. 2005;112(11):140–2.
-
10Nayak KC, Jain AK, Sharda DP, Mishra SN. Profile of cardiac complications of snake bite. Indian Heart J. 1990;42(3):185–8.
-
11Thewjitcharoen Y, Poopitaya S. Ventricular tachycardia, a rare manifestation of Russell’s viper bite: case report. J Med Assoc Thai. 2005;88(12):1931–3.
-
12Moore RS. Second-degree heart block associated with envenomation byVipera berus Arch Emerg Med. 1988;5(2):116–8.>
-
13Agarwal A, Kumar T, Ravindranath KS, Bhat P, Manjunath CN, Agarwal N. Sinus node dysfunction complicating viper bite. Asian Cardiovasc Thorac Ann. 2015;23(2):212–4.
-
14Karaye KM, Mijinyawa MS, Yakasai AM, Kwaghe V, Joseph GA, Iliyasu G, et al. Cardiac and hemodynamic features following snakebite in Nigeria. Int J Cardiol. 2012;156(3):326–8.
-
15Lalloo DG, Trevett AJ, Korinhona A, Nwokolo N, Laurenson IF, Paul M, et al. Snake bites by thePapuan taipan(Oxyuranus scutellatus canni): paralysis, hemostatic and electrocardiographic abnormalities, and effects of antivenom. Am J Trop Med Hyg. 1995;52(6):525–31.
-
16Gupta OP, Mewar SH, Kalantri SP, Jain AP, Jajoo UN. Reversible atrial fibrillation following snake bite. J Assoc Physicians India. 1987;35(7):535–6.
-
17Mowry JB, Spyker DA, Brooks DE, McMillan N, Schauben JL. Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 32ndAnnual Report. Clin Toxicol. 2014;2015:962–1146.
-
18Senthikumaran S, Meenakshisundaram R, Thirumalaikolundusubramanian P. Cardiac tamponade in Russell viper (Daboia russelii) bite: case report with brief review. J Emerg Med. 2012;42(3):288–90.
-
19Schnabel RB, Sullivan LM, Levy D, Pencina MJ, Massaro JM, D’AgostinoSrRB, et al. Development of a risk score for atrial fibrillation (Framingham Heart Study): a community-based cohort study. Lancet. 2009;373(9665):739–45.>
-
20Kannel WB, Abbott RD, Savage DD, McNamara PM. Epidemiologic features of chronic atrial fibrillation: the Framingham study. N Engl J Med. 1982;306(17):1018–22.
-
21Uhm JS, Shim J, Wi J, Mun HS, Park J, Park SH, et al. First-degree atrioventricular block is associated with advanced atrioventricular block, atrial fibrillation and left ventricular dysfunction in patients with hypertension. J Hypertens. 2014;32(5):1115–20.
-
22Workman AJ. Cardiac adrenergic control and atrial fibrillation. Naunyn Schmiedebergs Arch Pharmacol. 2010;381(3):235–49.
Abbreviations
- AF Atrial fibrillation
- AVB Atrioventricular block
- BUN Blood urea nitrogen
- ECG Electrocardiogram
- ICU Intensive care unit
- TSH Thyroid-stimulating hormone
- WBC White blood cell count
-
FundingNot applicable.
Publication Dates
-
Publication in this collection
2017
History
-
Received
8 Aug 2016 -
Reviewed
13 Mar 2017 -
Accepted
21 Mar 2017