Abstract
Antibiotic resistance is a growing public health concern. Antibiotics continue to be prescribed by some clinicians to resolve dental pain even though research indicates that antibiotics are not effective for treating conditions such as irreversible pulpitis. The objective of this study was to determine the extent to which current research and evidence around irreversible pulpitis has been translated into dental practice and the gaps in dentists’ knowledge. An on-line clinical vignette format survey questionnaire about treatment of irreversible pulpitis was distributed to the members of the Academy of Operative Dentistry and Academy of General Dentistry (US based international dental bodies). Their responses were recorded and evaluated. A total of 403 dentists participated in the survey. Over a third (39.3%) indicated they would prescribe antibiotics for symptomatic irreversible pulpitis in a permanent tooth occurring without any signs of systemic infection. The rest indicated they would not prescribe antibiotics; most of them would prescribe an analgesic combined with pulpectomy. Those who had undertaken advanced education training achieved a significantly higher mean knowledge score compared to those with just a primary dental degree (p=0.011). Similarly, full or part time academicians had a higher mean knowledge score than the clinicians who work only in private practice (p=0.014). Some dentists continue to prescribe antibiotics inappropriately for alleviating pain due to irreversible pulpitis. Antibiotic prescribing practices of dentists with advanced education or academic engagement were better as compared to the other participants. There is clear evidence of antibiotic over-prescribing for irreversible pulpitis which needs to be addressed urgently.
Key Words:
antibiotics; endodontics; survey; dentists; pain; prescriptions
Resumo
A resistência aos antibióticos é uma preocupação crescente para a saúde pública. Os antibióticos continuam a ser prescritos por alguns dentistas para resolver a dor dentária, embora pesquisas indiquem que os antibióticos não são eficazes no tratamento de condições como a pulpite irreversível. O objetivo deste estudo foi determinar em que medida as pesquisas atuais e as evidências em torno da pulpite irreversível foram traduzidas em prática odontológica e as lacunas existentes no conhecimento dos dentistas. Um questionário de pesquisa em formato de vinheta clínica on-line sobre o tratamento da pulpite irreversível foi distribuído para os membros da Academia de Odontologia Operatória e da Academia de Odontologia Geral (órgãos dentários internacionais dos EUA). Suas respostas foram registradas e avaliadas. Um total de 403 dentistas participou da pesquisa. Mais de um terço (39,3%) indicaram que prescreveriam antibióticos para pulpite irreversível sintomática em um dente permanente sem qualquer sinal de infecção sistêmica. O restante respondeu que eles não prescreveriam antibióticos; a maioria deles prescreveria um analgésico combinado com pulpectomia. Aqueles que realizaram o treinamento de educação avançada obtiveram uma pontuação de conhecimento médio significativamente maior em comparação com aqueles com apenas um grau primário de conhecimento odontológico (p=0,011). Da mesma forma, acadêmicos em tempo integral ou parcial tiveram uma pontuação média de conhecimento maior do que os clínicos que trabalham apenas em consultório particular (p=0,014). Alguns dentistas continuam a prescrever antibióticos inadequadamente para aliviar a dor decorrente de pulpite irreversível. Práticas de prescrição de antibióticos por dentistas com educação avançada ou envolvimento acadêmico foram melhores em comparação com os outros participantes. Há evidências claras de excesso de prescrição de antibiótico para pulpite irreversível que precisa ser tratada com urgência.
Introduction
There is growing concern that the unnecessary prescribing of antibiotics by healthcare providers is contributing to the development of drug-resistant bacteria 11 Dellit, TH, Owens, RC; McGowan, JE Jr; Gerding, DN; Weinstein, RA; Burke, JP; et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 2007;44:159-177.. Each year around two million drug-resistant infections cause 23,000 fatalities in the United States 22 Centers Centers for Disease Control and Prevention. Antibiotic/Antimicrobial Resistance. Available at:Available at:https://www.cdc.gov/drugresistance/index.html
. (Latest access May 2, 2019).
https://www.cdc.gov/drugresistance/index...
. It is estimated that the economic burden of antibiotic resistant infections (ARI) will increase beyond the burden of cancer and could result in significant mortality figures 33 TacklingTackling drug resistance globally: the review on antimicrobial resistance. Chaired by O’Neill May2016. Available at: Available at: https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf
(Latest access May 2, 2019).
https://amr-review.org/sites/default/fil...
. A steadily increasing trend of excessive antibiotic prescription by dentists for treating endodontic and orofacial infections has been reported to show that bacterial isolates from these infections are getting resistant to commonly used antibiotics 44 Rôças, IN; Siqueira, JF. Detection of antibiotic resistance genes in samples from acute and chronic endodontic infections and after treatment. Arch Oral Biol2013;58:1123-1128.. In 2014, dentists in the United States wrote 25.7 million antibiotic prescriptions, according to data released by the Centers for Disease Control 55 Centers Centers for Disease Control and Prevention. Outpatient antibiotic prescriptions - United States, 2014. Available at: Available at: http://www.cdc.gov/getsmart/community/pdfs/annual-reportsummary_2014.pdf
(Latest access May 2, 2019).
http://www.cdc.gov/getsmart/community/pd...
. It is imperative for patient safety that antibiotics are prescribed only when necessary to avoid exposing patients to the unnecessary risk from drug-resistant infections.
Evidence-based guidelines for the appropriate use of antibiotics in endodontic infections have been developed by the American Association of Endodontics and European Society of Endodontology 66 American Association of Endodontics. Publications and Research. Available at Available at https://www.aae.org/uploadedfiles/publications_and_research/endodontics_colleagues_for_excellence_newsletter/summer06ecfe.pdf
(Latest access May 2, 2019).
https://www.aae.org/uploadedfiles/public...
,77 Segura-Egea, JJ; Gould, K; Sen ,BH; Jonasson, P; Cotti, E; Mazzoni, A; et al. European Society of Endodontology position statement: the use of antibiotics in endodontics. Int Endod J 2018;51:20-25.. Clinical situations that require antibiotic therapy on an empirical basis are limited and include oral infection with evidence of systemic spread such as lymphadenopathy and trismus. Although, there is sufficient evidence to support the consensus that antibiotic use does not alleviate pain in symptomatic irreversible pulpitis, it appears that a considerable number of dentists could still be prescribing antibiotics for this purpose 88 Agnihotry, A; Fedorowicz, Z; Van Zuuren, EJ; Farman, AG; Al-Langawi, JH. Antibiotic use for irreversible pulpitis. Cochrane Database Syst Rev 2016;2:CD004969.,99 Agnihotry, A; Fedorowicz, Z; Al-Langawi, JH; Moghadam, S; Kochhar, R; Cohen, S. Improving the “Implications for Practice/Research” section of a Cochrane Review using a survey questionnaire. Cochrane Colloquium 2014; 09/2014. doi: 10.13140/2.1.4116.9925
https://doi.org/10.13140/2.1.4116.9925...
. In non-traumatic dental emergencies, irreversible pulpitis has been documented as the main reason patients present with pain 1010 Lipton, JA; Ship, JA; Larach-Robinson, D. Estimated prevalence and distribution of reported orofacial pain in the United States. J Am Dent Assoc 1993;124:115-121.. Substandard prescribing practices by dentists, are reported to be associated with several factors ranging from inadequate knowledge to social factors (which are described as convenience and patients demanding antibiotic prescriptions) 1111 Dar-Odeh, NS; Abu-Hammad, OA; Al-Omiri, MK; Khraisat, AS; Shehabi, AA. Antibiotic prescribing practices by dentists: a review. Ther Clin Risk Manag 2010;6:301-306..
The key objective of this study was to determine the extent to which the current evidence around irreversible pulpitis has been translated into practice. An online survey was conducted to understand the prescribing habits reported by general dentists and to identify gaps in their knowledge.
Material and Methods
An on-line clinical vignette style survey (Fig. 1) was developed and the study was certified exempt by the Institutional Review Board at the University of California, Los Angeles (IRB #16-000500). The survey consisted of a single question with six possible treatment options, two of which provided a preference for prescribing of antibiotics for irreversible pulpitis. Survey participants consisted of members of the Academy of General Dentistry (AGD) and the Academy of Operative Dentistry (AOD). The participants were a sample of: general dentists (predominantly from United States but a global sample); dentists in military/public health services, Indian Health Service (for American Indians and Alaska Natives) and other health services; dentists not currently practicing clinical dentistry; prosthodontists from private practice; postdoctoral residents in Prosthodontics, Advanced Education in General Dentistry, and General Practice residency who are members of the Academy of Operative Dentistry (AOD) or Academy of General Dentistry (AGD); academics (full or part-time, with or without clinical practice). All the participants were asked to indicate their highest level of dental training and their number of years of experience in the field of dentistry, but their identities were kept anonymous.
A link to the survey questionnaire was distributed via direct email for AOD members and via the weekly online newsletter, “AGDinAction” sent through ‘news@agd.org’ for AGD members: https://docs.google.com/forms/d/e/1FAIpQLSf0n_NNDqqOHWlvYrJRD8x-PsZR3_buPGH6VDV2vuAl7r9wbA/viewform. It was circulated to AGD participants on two occasions (June 15th, 2016 and July 13th, 2016) using the web resources of AGD. The responses were registered, imported into Microsoft Excel and further analyzed.
Results
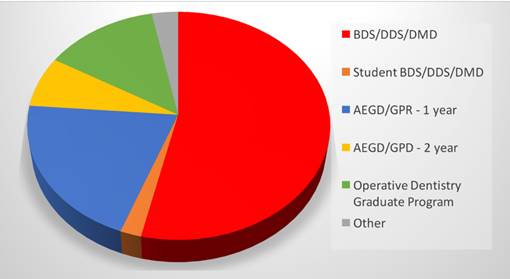
A total of 403 participants contributed to the survey. Among these, 388 (96.3%) were general dentists and 15 (3.7%) were prosthodontists. Just over half of the participants (54.5%) were working towards or had only achieved a primary dental degree (BDS/DDS/DMD); the rest were in or had achieved some form of advanced training program [Advanced Education in General Dentistry (AEGD), General Practice Residency (GPR), Operative Dentistry Graduate Program or Prosthodontics Residency] (Fig. 2). A total of 262 (65%) worked in private practice followed by 64 (15.9%), who were full-time academics with clinical practice. Thirty-six (8.9%) of the study participants were certified by the American Board of Operative Dentistry. The mean duration of clinical practice for all participants was 22.14±14.1 years.
A total of 244 (60.7%) of the study participants would not prescribe antibiotics for irreversible pulpitis in a permanent tooth, with vital pulp confirmed by the standard tests, and without any evidence of soft-tissue swelling. The majority of these participants (56.3%) would prescribe analgesics and perform concurrent pulpectomy. A small minority (4.2%) would prescribe analgesics immediately and schedule a root canal treatment for a later time.
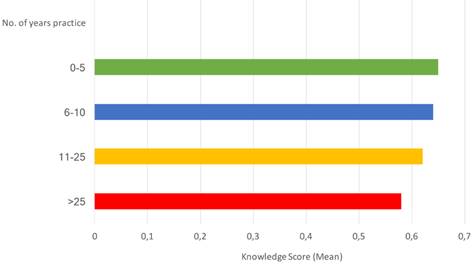
In the present study, 39.3% of the participants reported they would prescribe antibiotics for irreversible pulpitis affecting a permanent tooth without any signs of systemic infection. There was no significant difference in mean knowledge score based on number of years of clinical practice (p=0.66), although there was a trend towards reducing knowledge scores with increasing number of years in practice (Fig. 3). When participants were categorized on the basis of their level of dental training, those who had 1 or 2 years of advanced training (AEGD or GPR) had a significantly higher mean knowledge score compared to those with primary qualifications (BDS/DDS/DMD). (p=0.011). Participants with an academic element to their role (those in full-time academia with a clinical practice, full-time academics without a clinical practice or part-time academics with a private practice) had a significantly higher mean knowledge score than private practitioners (p=0.014).
Discussion
There is sufficient evidence to show that antibiotics are largely ineffective in controlling pain due to irreversible pulpitis 88 Agnihotry, A; Fedorowicz, Z; Van Zuuren, EJ; Farman, AG; Al-Langawi, JH. Antibiotic use for irreversible pulpitis. Cochrane Database Syst Rev 2016;2:CD004969.. However, over a third of dentists participating in our survey chose to prescribe antibiotics. Our findings concur with a report from Saudi Arabia, where 42% of dentists prescribed antibiotics 1212 Iqbal, A. The attitudes of dentists towards the prescription of antibiotics during endodontic treatment in north of Saudi Arabia. J Clin Diagn Res 2015;9:ZC82-ZC84. and the Spanish Endodontic Society which reported a figure of 40% in 2008 1313 Rodriguez-Núñez, A; Cisneros-Cabello, R; Velasco-Ortega, E; Llamas-Carreras, JM; Tórres-lagares, D; Segura-Egea, JJ. Antibiotic use by members of the Spanish Endodontic Society. J Endod 2009;35:1198-1203.. A survey in 2016 by the American Association of Endodontics found that 8.1% of its members would prescribe antibiotics for irreversible pulpitis 1414 Germack, M; Sedgley, CM; Sabbab, W; Whitten, B. Antibiotic use in 2016 by members of the American Association of Endodontics: report of a national survey. J Endod2017;43:1615-1622.. Similarly, a Welsh national audit of antibiotic prescribing published in 2016 found that 5% of all antibiotics prescribed by general dentists during the audit period were for irreversible pulpitis 1515 Cope, AL; Barnes, E; Howells, EP; Rockey, AP; Karki, AJ; Wilson, MJ; et al. Antimicrobial prescribing by dentists in Wales; UK: findings of the first cycle of a clinical audit. Br Dent J 2016;221:25-30. . These figures show a clear and unmistakable trend of over-prescription for irreversible pulpitis at the global level.
Education
The number of years of experience post-graduation showed little effect on the prescribing habits reported by dentists. In spite of the shift towards an evidence-based approach in dentistry and with the availability of clinical practice guidelines, this illustrates that irrespective of when dental clinicians graduated (and by inference what they were taught at dental school ) there appears to be little different in the approach to prescribing for irreversible pulpitis. Courses delivered as CE/CPD could provide the dentists with an understanding of the harmful effects of antibiotic over-prescription and educate them about the evidence-based guidelines on when to prescribe antibiotics. Given the high profile and patient safety risks associated with the over-prescription of antibiotics, it would be prudent for dental regulatory authorities to consider introducing a minimum requirement of CE/CPD credits in relation to antibiotic prescription in dentistry 1616 American Dental Association. Dentist continuing education state ce statutes and regulations. Available at: Available at: http://www.ada.org/~/media/ADA/Advocacy/Files/continuing_ed
. (Latest access May 2; 2019).
http://www.ada.org/~/media/ADA/Advocacy/...
.
General dental practitioners with advanced training (AEGD or GPR) prescribed antibiotics less frequently than general dental practitioners with just a primary dental degree (BDS/DDS/DMD). These dentists could provide advocacy and be role models of optimal antibiotic prescribing for less highly qualified colleagues working in practice. As trusted colleagues of other general dentists, they could also be ideally placed to deliver the CE/CPD courses identified above.
Academic Role
Another area with potential for future targeting in order to reduce overprescribing is the finding that dentists working in an academic environment (either part-time, or full time) were less likely to prescribe antibiotics for irreversible pulpitis than general dental practitioners working exclusively in a private practice setting. This suggests that spending time in an academic environment might help instill more optimal antibiotic prescription practices. Encouraging more general dentists to spend time working at least part-time in academia may be an effective way of improving knowledge about (and hence reducing overprescribing of) antibiotics. Whether a similar pattern could be seen in relation to other guidelines/issues would be an interesting area for further research.
Difficulty Achieving Anesthesia
One further interesting element of the survey which was raised by some of the responders in personal correspondence to the survey authors was failure to achieve anesthesia of a ‘hot tooth’. Around half of patients diagnosed with irreversible pulpitis have been reported as difficult to anesthetize 1717 Owatz, CB; Khan, AA; Schindler, WG; Schwartz, SA; Keiser, K; Hargreaves, KM. The incidence of mechanical allodynia in patients with irreversible pulpitis. J Endod 2007;33:552-556.,1818 Drum, M; Reader, A; Nusstein, J; Fowler, S. Successful pulpal anesthesia for symptomatic irreversible pulpitis. J Am Dent Assoc 2017;148:267-271.. This was referred to in the survey as ‘hot tooth’. A condition which arises as a result of inflammation, and with local changes occurring in the nerve tissue causing heightened response to stimuli such as for example hot or cold 1919 Lolignier, S; Eijkelkamp, N; Wood, JN. Mechanical allodynia. Pflugers Arch 2015;467:133-139.. In these cases, the traditional methods of local anesthesia may be less than effective. Many methods have been advocated to increase the chances of success of anesthesia for this condition, such as intra-bony anesthetic injections, nitrous oxide sedation, using high concentrations of long acting anesthesia, using corticosteroids; but reinjection improves success rates to level of 92%-96% 2020 Nusstein, J; Reader, A; Nist, R; Beck, M; Meyers, WJ. Anesthetic efficacy of the supplemental intraosseous injection of 2% lidocaine with 1:100;000 epinephrine in irreversible pulpitis. J Endod1998;24:487-491.,2121 Smith, GN; Walton, RE; Abbott, BJ. Clinical evaluation of periodontal ligament anesthesia using a pressure syringe. J Am Dent Assoc 1983;107:953-956.,2222 Walton, RE. The periodontal ligament injection as a primary technique. J Endod1990;16:62-66.,2323 Cohen, HP; Cha, BY; Spångberg, LS. Endodontic anesthesia in mandibular molars: a clinical study. J Endod 1993;19:370-373.,2424 Stanley, W; Drum, M; Nusstein, J; Reader, A; Beck, M. Effect of nitrous oxide on the efficacy of the inferior alveolar nerve block in patients with symptomatic irreversible pulpitis. J Endod2012;38:565-569.,2525 Aggarwal, V; Singla, M; Rizvi, A; Miglani, S. Comparative evaluation of local infiltration of articaine; articaine plus ketorolac; and dexamethasone on anesthetic efficacy of inferior alveolar nerve block with lidocaine in patients with irreversible pulpitis. J Endod 2011;37:445-449.,2626 Bane, K; Charpentier, E; Bronnec, F; Descroix, V; Gaye-N'diaye, F; Kane, AW; et al. Randomized clinical trial of intraosseous methylprednisolone injection for acute pulpitis pain. J Endod 2016;42:2-7.. In these ‘hot tooth’ clinical situations, some dentists appear to confuse inflammation with infection, and inappropriately prescribe antibiotics. Evidence-based guidance on the optimal analgesic routine for use by general dentists to treat teeth with irreversible pulpitis during urgent appointments could be a helpful way of reducing the over-prescription of antibiotics.
Dental Antibiotic Stewardship
Governments around the world are setting out their antibiotic stewardship plan to address the risk of drug-resistant infections by reducing the overprescribing of antibiotics, including in outpatient settings 2727 Joint Joint commission joins white house effort to reduce antibiotic overuse. Jt Comm Perspect2015;35:4;11.,2828 DentalDental antimicrobial stewardship: toolkit. Available at: Available at: http://www.gov.uk/guidance/dental-antimicrobial-stewardship-toolkit
(Latest access May 2; 2019).
http://www.gov.uk/guidance/dental-antimi...
. In response, national dental bodies, faculties and associations (such as the American Dental Association (ADA)) have pledged to improve the dental prescribing practices, including by providing evidence-based recommendations and systematic reviews 2828 DentalDental antimicrobial stewardship: toolkit. Available at: Available at: http://www.gov.uk/guidance/dental-antimicrobial-stewardship-toolkit
(Latest access May 2; 2019).
http://www.gov.uk/guidance/dental-antimi...
,2929 American Dental Association. ADA supports responsible antibiotic use- June 2015Available at: Available at: http://www.ada.org/en/publications/ada-news/2015-archive/june/ada-supports-responsible-antibiotic-use
(Latest access May 2; 2019).
http://www.ada.org/en/publications/ada-n...
,3030 Thompson, W; Sandoe, J. What does NICE have to say about antimicrobial stewardship to the dental community? BDJ2016Feb 26:220:193-195.. Our findings suggest that irreversible pulpitis is a condition which should be explicitly included in approaches to dental antibiotic stewardship.
Guidelines alone, however, are unlikely to be the answer to reducing overprescribing 3131 Wieringa, S; Greenhalgh, T. 10 years of mindlines: a systematic review and commentary. Implement Sci2015; 10: 45.. There is evidence that audit and feedback of an individual’s prescribing practice against guidelines can be effective at optimizing their prescribing. A good example of this is the Scottish ‘Reducing Antibiotic Prescribing in Dentistry’ (RAPiD) trial. The results of this trial illustrated that using routinely collected national data to provide feedback to primary care dentists resulted in a significant reduction in antibiotic prescribing rates, with the highest prescribers showing the greatest reduction in their prescribing rate 3232 Elouafkaoui, P; Young, L; Newlands, R; Duncan, EM; Elders, A; Clarkson, JE; et al. An audit and feedback intervention for reducing antibiotic prescribing in general dental practice: the rapid cluster randomised controlled trial. PLoS Med 13:e1002115 2015.. Similarly, in the US, the Centers for Medicare & Medicaid Services (CMS) Antibiotic Stewardship program has instituted the provision of added incentives for clinicians to optimize their prescribing through a quality based payment program: Merit-based Incentive Payment System (MIPS) 3333 Quality Quality Payment Program. MIPS Overview. Available at: Available at: https://qpp.cms.gov/mips/overview
(Latest access May 2; 2019).
https://qpp.cms.gov/mips/overview...
. CMS Antibiotic Stewardship to improve prescription behaviors for certain high-priority conditions is one of the elements of this program.
Limitation of the Study
A limitation of the study is the low response rate. This is fairly typical of surveys of health professionals and has been further reinforced by response rates showing a decrease over recent years 3434 Funkhouser, E; Vellala, K; Baltuck, C; Cacciato, R; Durand, E; McEdward, D; et al. Survey methods to optimize response rate in the national dental practice-based research network. Eval Health Prof 2017;40:332-358.. Although the response rate recorded for this survey was less than 2% of all the members of AGD, it is unclear how many of its members read the online newsletter which included details about participating in the survey. Thus, we cannot be precise about the percentage of people who read but chose not to respond to the survey. Exploration of how to use electronic media to best effect, including increasing reach as well as response rates from members of the dental team, is identified as an area ripe for future research.
Antibiotic Over Prescription Across Healthcare
Antibiotic over prescription all across healthcare has been a challenge. Amongst a group of inpatient physicians, it was found that over prescription was largely due to anxiety of missing an infection, whereas potential adverse effects of antibiotics had no strong influence over decision making. 3535 Livorsi, D; Comer, A; Matthias, MS; Perencevich, EN; Bair, MJ. Factors influencing antibiotic-prescribing decisions among inpatient physicians: A qualitative investigation. Infect Control Hosp Epidemiol2015;36:1065-1072.. It has been seen as an issue with urinary tract infections 3636 Blumberg, EA. Just say no: stemming the tide of antibiotic overprescription. Am J Transplant 2016;16:2779-2780. and respiratory tract infections 3737 Dekker, AR; Verheij, TJ; Van der Velden, AW. Inappropriate antibiotic prescription for respiratory tract indications: most prominent in adult patients. Fam Pract 2015;32:401-407. very commonly. Interestingly, antibiotic prescriptions for childhood infections in primary care often result from “just in case” prescribing while the physicians mentioned social pressure from the parents as a cause for prescribing, even though, they were concerned about adverse effects and resistance of the antibiotics. 3838 Lucas, PJ; Cabral, C; Hay, AD; Horwood, J. A systematic review of parent and clinician views and perceptions that influence prescribing decisions in relation to acute childhood infections in primary care. Scand J Prim Health Care 2015;33:11-20.. Some parallels can be drawn here with dental over prescription.
A significant proportion of general dentists overprescribe antibiotics for irreversible pulpitis. Whilst a dentist’s number of years of experience showed no statistically significant difference on his or her reported antibiotic prescription behavior, there was a trend towards increased over-prescribing with increasing years in practice. Those dentists who have an academic element to their role and/or those having undertaken advanced training post-graduation reported prescribing antibiotics less frequently. It is suggested that irreversible pulpitis should be included as a key condition to be addressed within dental antibiotic stewardship programs (including training, guideline development and other interventions).
Acknowledgements
The authors would like to thank Rohitashva Agrawal MBBS, MPH, PGDMLE, PGDIPRL for his guidance in preparing the discussion section.
References
-
1Dellit, TH, Owens, RC; McGowan, JE Jr; Gerding, DN; Weinstein, RA; Burke, JP; et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 2007;44:159-177.
-
2Centers Centers for Disease Control and Prevention. Antibiotic/Antimicrobial Resistance. Available at:Available at:https://www.cdc.gov/drugresistance/index.html (Latest access May 2, 2019).
» https://www.cdc.gov/drugresistance/index.html -
3TacklingTackling drug resistance globally: the review on antimicrobial resistance. Chaired by O’Neill May2016. Available at: Available at: https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf (Latest access May 2, 2019).
» https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf -
4Rôças, IN; Siqueira, JF. Detection of antibiotic resistance genes in samples from acute and chronic endodontic infections and after treatment. Arch Oral Biol2013;58:1123-1128.
-
5Centers Centers for Disease Control and Prevention. Outpatient antibiotic prescriptions - United States, 2014. Available at: Available at: http://www.cdc.gov/getsmart/community/pdfs/annual-reportsummary_2014.pdf (Latest access May 2, 2019).
» http://www.cdc.gov/getsmart/community/pdfs/annual-reportsummary_2014.pdf -
6American Association of Endodontics. Publications and Research. Available at Available at https://www.aae.org/uploadedfiles/publications_and_research/endodontics_colleagues_for_excellence_newsletter/summer06ecfe.pdf (Latest access May 2, 2019).
» https://www.aae.org/uploadedfiles/publications_and_research/endodontics_colleagues_for_excellence_newsletter/summer06ecfe.pdf -
7Segura-Egea, JJ; Gould, K; Sen ,BH; Jonasson, P; Cotti, E; Mazzoni, A; et al. European Society of Endodontology position statement: the use of antibiotics in endodontics. Int Endod J 2018;51:20-25.
-
8Agnihotry, A; Fedorowicz, Z; Van Zuuren, EJ; Farman, AG; Al-Langawi, JH. Antibiotic use for irreversible pulpitis. Cochrane Database Syst Rev 2016;2:CD004969.
-
9Agnihotry, A; Fedorowicz, Z; Al-Langawi, JH; Moghadam, S; Kochhar, R; Cohen, S. Improving the “Implications for Practice/Research” section of a Cochrane Review using a survey questionnaire. Cochrane Colloquium 2014; 09/2014. doi: 10.13140/2.1.4116.9925
» https://doi.org/10.13140/2.1.4116.9925 -
10Lipton, JA; Ship, JA; Larach-Robinson, D. Estimated prevalence and distribution of reported orofacial pain in the United States. J Am Dent Assoc 1993;124:115-121.
-
11Dar-Odeh, NS; Abu-Hammad, OA; Al-Omiri, MK; Khraisat, AS; Shehabi, AA. Antibiotic prescribing practices by dentists: a review. Ther Clin Risk Manag 2010;6:301-306.
-
12Iqbal, A. The attitudes of dentists towards the prescription of antibiotics during endodontic treatment in north of Saudi Arabia. J Clin Diagn Res 2015;9:ZC82-ZC84.
-
13Rodriguez-Núñez, A; Cisneros-Cabello, R; Velasco-Ortega, E; Llamas-Carreras, JM; Tórres-lagares, D; Segura-Egea, JJ. Antibiotic use by members of the Spanish Endodontic Society. J Endod 2009;35:1198-1203.
-
14Germack, M; Sedgley, CM; Sabbab, W; Whitten, B. Antibiotic use in 2016 by members of the American Association of Endodontics: report of a national survey. J Endod2017;43:1615-1622.
-
15Cope, AL; Barnes, E; Howells, EP; Rockey, AP; Karki, AJ; Wilson, MJ; et al. Antimicrobial prescribing by dentists in Wales; UK: findings of the first cycle of a clinical audit. Br Dent J 2016;221:25-30.
-
16American Dental Association. Dentist continuing education state ce statutes and regulations. Available at: Available at: http://www.ada.org/~/media/ADA/Advocacy/Files/continuing_ed (Latest access May 2; 2019).
» http://www.ada.org/~/media/ADA/Advocacy/Files/continuing_ed -
17Owatz, CB; Khan, AA; Schindler, WG; Schwartz, SA; Keiser, K; Hargreaves, KM. The incidence of mechanical allodynia in patients with irreversible pulpitis. J Endod 2007;33:552-556.
-
18Drum, M; Reader, A; Nusstein, J; Fowler, S. Successful pulpal anesthesia for symptomatic irreversible pulpitis. J Am Dent Assoc 2017;148:267-271.
-
19Lolignier, S; Eijkelkamp, N; Wood, JN. Mechanical allodynia. Pflugers Arch 2015;467:133-139.
-
20Nusstein, J; Reader, A; Nist, R; Beck, M; Meyers, WJ. Anesthetic efficacy of the supplemental intraosseous injection of 2% lidocaine with 1:100;000 epinephrine in irreversible pulpitis. J Endod1998;24:487-491.
-
21Smith, GN; Walton, RE; Abbott, BJ. Clinical evaluation of periodontal ligament anesthesia using a pressure syringe. J Am Dent Assoc 1983;107:953-956.
-
22Walton, RE. The periodontal ligament injection as a primary technique. J Endod1990;16:62-66.
-
23Cohen, HP; Cha, BY; Spångberg, LS. Endodontic anesthesia in mandibular molars: a clinical study. J Endod 1993;19:370-373.
-
24Stanley, W; Drum, M; Nusstein, J; Reader, A; Beck, M. Effect of nitrous oxide on the efficacy of the inferior alveolar nerve block in patients with symptomatic irreversible pulpitis. J Endod2012;38:565-569.
-
25Aggarwal, V; Singla, M; Rizvi, A; Miglani, S. Comparative evaluation of local infiltration of articaine; articaine plus ketorolac; and dexamethasone on anesthetic efficacy of inferior alveolar nerve block with lidocaine in patients with irreversible pulpitis. J Endod 2011;37:445-449.
-
26Bane, K; Charpentier, E; Bronnec, F; Descroix, V; Gaye-N'diaye, F; Kane, AW; et al. Randomized clinical trial of intraosseous methylprednisolone injection for acute pulpitis pain. J Endod 2016;42:2-7.
-
27Joint Joint commission joins white house effort to reduce antibiotic overuse. Jt Comm Perspect2015;35:4;11.
-
28DentalDental antimicrobial stewardship: toolkit. Available at: Available at: http://www.gov.uk/guidance/dental-antimicrobial-stewardship-toolkit (Latest access May 2; 2019).
» http://www.gov.uk/guidance/dental-antimicrobial-stewardship-toolkit -
29American Dental Association. ADA supports responsible antibiotic use- June 2015Available at: Available at: http://www.ada.org/en/publications/ada-news/2015-archive/june/ada-supports-responsible-antibiotic-use (Latest access May 2; 2019).
» http://www.ada.org/en/publications/ada-news/2015-archive/june/ada-supports-responsible-antibiotic-use -
30Thompson, W; Sandoe, J. What does NICE have to say about antimicrobial stewardship to the dental community? BDJ2016Feb 26:220:193-195.
-
31Wieringa, S; Greenhalgh, T. 10 years of mindlines: a systematic review and commentary. Implement Sci2015; 10: 45.
-
32Elouafkaoui, P; Young, L; Newlands, R; Duncan, EM; Elders, A; Clarkson, JE; et al. An audit and feedback intervention for reducing antibiotic prescribing in general dental practice: the rapid cluster randomised controlled trial. PLoS Med 13:e1002115 2015.
-
33Quality Quality Payment Program. MIPS Overview. Available at: Available at: https://qpp.cms.gov/mips/overview (Latest access May 2; 2019).
» https://qpp.cms.gov/mips/overview -
34Funkhouser, E; Vellala, K; Baltuck, C; Cacciato, R; Durand, E; McEdward, D; et al. Survey methods to optimize response rate in the national dental practice-based research network. Eval Health Prof 2017;40:332-358.
-
35Livorsi, D; Comer, A; Matthias, MS; Perencevich, EN; Bair, MJ. Factors influencing antibiotic-prescribing decisions among inpatient physicians: A qualitative investigation. Infect Control Hosp Epidemiol2015;36:1065-1072.
-
36Blumberg, EA. Just say no: stemming the tide of antibiotic overprescription. Am J Transplant 2016;16:2779-2780.
-
37Dekker, AR; Verheij, TJ; Van der Velden, AW. Inappropriate antibiotic prescription for respiratory tract indications: most prominent in adult patients. Fam Pract 2015;32:401-407.
-
38Lucas, PJ; Cabral, C; Hay, AD; Horwood, J. A systematic review of parent and clinician views and perceptions that influence prescribing decisions in relation to acute childhood infections in primary care. Scand J Prim Health Care 2015;33:11-20.
Publication Dates
-
Publication in this collection
22 July 2019 -
Date of issue
Jul-Aug 2019
History
-
Received
11 Apr 2019 -
Accepted
10 June 2019