Abstract
Purpose:
To evaluate whether the use of the physical surgical simulator may benefit the development of laparoscopic skills.
Methods:
Ten medical students were divided into two groups: the first one performed ten weekly training sessions with a physical surgical simulator - ETX A2 LAP and, afterwards, one laparoscopic cholecystectomy in a porcine model, while the second group performed only a laparoscopic cholecystectomy. Both groups were compared regarding bleeding, total surgical time, time to perform each surgical step and qualitative parameters, based on a previously validated tool.
Results:
There was no difference in any of the evaluated parameters.
Conclusion:
We did not find any evidence of benefit in the use of the physical simulator for surgical performance in medical students.
Key words:
Laparoscopy; Training; Education, Medical
Introduction
Learning surgery is a dynamic, extensive and multifaceted process. Besides the extensive range of theoretical learning, surgeons must possess an immense practical training experience in order to reach a satisfactory domain of surgical skills and be responsible for leading the operation room. To reach this ability level, surgeons relied on various training methods throughout history: corpse’s dissection, surgery in animals and by attending surgical procedures with experienced surgeons dedicated to teaching. However, with the tremendous development of medical technology in recent decades, especially in the field of laparoscopic surgery, the opportunity and the need for new teaching methods arises.
With the advent of laparoscopic surgery, introduced effectively by Kurt Semm in 1980 with the first laparoscopic appendectomy in humans, a true revolution happened11. Litynski GS. Kurt Semm and the fight against skepticism: endoscopic hemostasis, laparoscopic appendectomy, and Semm's impact on the "laparoscopic revolution". JSLS. 1998 Jul-Sep.;2(3):309-13. PMID: 9876762.. The improvement of laparoscopic surgical technique over the years has allowed this approach to present several advantages over conventional surgery, such as: lower rate of postoperative infection, better cosmetic results, shorter hospital stay and faster postoperative recovery22. Bruhat MA, Chapron C, Mage G, Pouly JL, Canis M, Wattiez A, Glowaczower E. The benefits and risks of laparoscopic surgery. Rev Fr Gynecol Obstet. 1993;88(2):84-8. PMID: 8469869.,33. Jonsson B, Zethraeus N. Costs and benefits of laparoscopic surgery--a review of the literature. Eur J Surg. 2000;Suppl(585):48-56. PMID: 10885558.. Thus, laparoscopy has evolved over the years and is currently the gold standard for some procedures, such as cholecystectomy, and discussed whether it should be considered the gold standard for others, like appendectomy44. Fingerhut A, Millat B, Borrie F. Laparoscopic versus open appendectomy: time to decide. World J Surg. 1999;23:835-845. PMID: 10415210.,55. Sasi, W. Dissection by ultrasonic energy versus monopolar electrosurgical energy in laparoscopic cholecystectomy. JSLS. 2010 Jan-Mar;14(1):23-34. PMID: 20412640.. However, the search for better methods of teaching laparoscopic surgery is still the subject of extensive research.
The traditional forms of learning surgery, such as the use of corpses and animals, provide good training opportunities, but present significant obstacles to large-scale use. The main ones are: ethical matters, material shortage, the impossibility to reproduce specific pathologic conditions and some technical details such as the absence of bleeding in corpses or anatomical differences in animals66. Hoffman H, Vu D. Virtual reality: teaching tool of the twenty-first century? Acad Med. 1997 Dec;72(12):1076-81. PMID: 9435714.,77. Hamilton EC, Scott DJ, Fleming JB, Rege RV, Laycock R, Bergen PC, Tesfay ST, Jones DB. Comparison of video trainer and virtual reality training systems on acquisition of laparoscopic skills. Surg Endosc. 2002 Mar;16(3):406-11. PMID: 11928017.. Subramoniam et al.88. Subramonian K, DeSylva S, Bishai P, Thompson P, Muir G. Acquiring surgical skills: a comparative study of open versus laparoscopic surgery. Eur Urol. 2004;45(3):346-51. PMID: 15036681., when comparing learning differences between conventional and laparoscopic surgeries, found that the difficulty is greater for laparoscopic surgery, even after training, and that the main difficulties were fine dissections and correct identification of plans. In this context, virtual reality surgical simulators (VRSS) and physical simulators have emerged.
The VRSS already have a considerable spread in the surgical teaching process and extensive approach in the literature. Some of its advantages include: unlimited possibility of repetition, tasks can be adjusted to your needs and decreased use of experimental animals99. Uranüs S, Yanik M, Bretthauer G., Virtual reality in laparoscopic surgery. Stud Health Technol Inform. 2004;104:151-5. PMID: 15747974.. Furthermore, the possibility of measuring several parameters and documentation of results are important gains that VRSS provide for self-learning1010. Wanzel KR, Ward M, Reznick RK. Teaching the surgical craft: from selection to certification. Curr Probl Surg. 2002 Jun;39(6):573-659. PMID: 12037512.. Hart et al.1111. Hart R, Karthigasu K. The benefits of virtual reality simulator training for laparoscopic surgery. Curr Opin Obstet Gynecol. 2007 Aug;19(4):297-302. PMID: 17625408. also highlights the possibility of anticipating deficiencies that surgeons may have, before they occur.
On the other hand, the literature also shows negative points about the VRSS. The high costs of purchase and upgrade are barriers to the widespread use1212. Lehmann KS, Gröne J, Lauscher JC, Ritz JP, Holmer C, Pohlen U, Buhr HJ. Simulation training in surgical education - application of virtual reality laparoscopic simulators in a surgical skills course. Zentralbl Chir. 2012 Apr;137(2):130-7. PMID: 22495487.. There is also difficulty in integrating their use in clinical practice and in the surgeon’s curriculum1313. Kneebone R. Simulation in surgical training: educational issues and practical implications. Med Educ. 2003;37(3):267-77. PMID: 12603766.. At last, tissue representation is artificial and still not entirely consistent with reality1414. Feldman LS, Sherman V, Fried GM. Using simulators to assess laparoscopic competence: ready for widespread use? Surgery. 2004;135(1):28-42. PMID: 14694298..
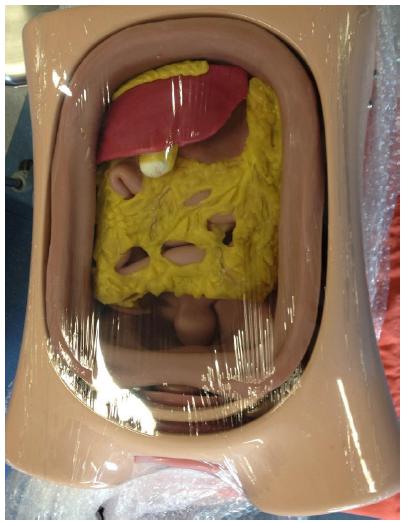
The physical simulator ETX A2 LAP (Prodelphus, Olinda-PE, Brazil) is a new tool for surgical training. It consists basically of a manikin with full representation of abdominal organs, including vessels and nerves. There is a mechanism for simulation of bleeding and organ injury. Although it is a very promising tool is has been little explored in the literature for surgical training. In other fields, such as anesthesiology, the use of manikins is well established and discussed1515. Tokarczyk AJ, Greenberg SB. Use of mannequin-based simulators in anesthesiology. Dis Mon. 2011 Nov;57(11):706-14. PMID: 22082556..
The purpose of this study is to evaluate whether the use of physical simulator ETX A2 LAP), as a method of training for laparoscopic surgery, results in surgical performance improvement in medical students.
Methods
Ten students enrolled in the School of Medicine of Universidade de São Paulo, between the 5th and 6th grade were evaluated. Students had prior mild experience in laparoscopy, since they had basic training in the disciplines of surgical technique given in the third and fifth years of graduation. They were randomly assigned into two groups (groups I and II), consisting of 5 students each. Group II was the control group. Participants’ demographics are described in Chart 1.
Members of group I underwent ten weekly sessions of simulator training ETX A2 LAP (Prodelphus, Olinda-PE, Brazil) in which they would perform a laparoscopic cholecystectomy in the physical model (Figures 1 to 4). Thereafter, each student performed a cholecystectomy in swine model. Students performed ten sessions because it is estimated that about the eighth session they would have achived the plateau of their learning curve1616. da Cruz JA, Sandy NS, Passerotti CC, Nguyen H, Antunes AA, Dos Reis ST, Dall'Oglio MF, Duarte RJ, Srougi M. Does training laparoscopic skills in a virtual reality simulator improve surgical performance? J Endourol. 2010 Nov;24(11):1845-9. PMID: 20958203.. The members of the group II (control) underwent only a cholecystectomy each, without prior training, under identical conditions to group I. A surgeon experienced in laparoscopy accompanied each procedure. All participants attended a lecture where the necessary instruments and surgical steps were presented, alongside with a video explaining the procedure.
All participants signed a consent form, but were not informed of the parameters that would be evaluated (blinded). All surgeries were recorded and the volume of aspirated blood was measured. A experienced surgeon evaluated the videos of each surgery performed. The evaluator was not informed to which group each video belonged (“blinded”).
Quantitative parameters analyzed during the cholecystectomies of each participant were: time spent for dissection of the gallbladder pedicle, time spent clipping the pedicle, time spent sectioning the pedicle, time taken to remove the gallbladder from the liver bed, total time of the procedure and aspirated blood loss (irrigation was subtracted).
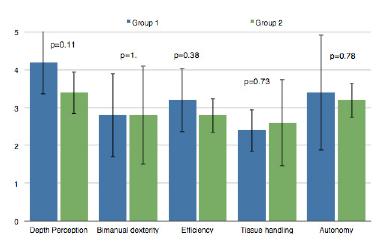
The qualitative aspects were evaluated based on criteria presented on a previously validated tool by Vassiliou et al called Global Operative Assessment of Laparoscopic Skills (GOALS)1717. Vassiliou MC, Feldman LS, Andrew CG, Bergman S, Leffondre K, Stanbridge D, Fried GM. A global assessment tool for evaluation of intraoperative laparoscopic skills. Am J Surg. 2005 Jul;190(1):107-13. PMID: 15972181., which consists in a rating scale of five aspects of minimally invasive procedures: depth perception, bimanual dexterity, efficiency, handling of tissues and autonomy. For each aspect, the individual is given a score varying from 1 to 5 (Table 1).
The animals were anesthetized with Telazol (4.4 to 6.6 mg/kg intramuscularly), xylazine (1.1 to 2.2 mg / kg im) and atropine (0.04 mg/kg intramuscularly) Anesthesia was maintained with isoflurane (1% to 4%) mixed with 1 to 2 liters of oxygen through an endotracheal tube. After the procedures, the animals were sacrificed by intravenous injection of a lethal dose of KCl.
The results from both groups (I and II) were subjected to statistical analysis with a significance level of 5%. The variables were first assessed for normality through Kolmogorov Smirnov test. Variables with normal distribution were compared through t-test, the remaining ones were compared with Mann-Whitney test. The software used was StatPlus® v. 2009 for Mac.
Results
The results for the laparoscopic cholecystectomy in the swine model for both groups, alongside with the corresponding p value, are demonstrated in Table 2.
The results show no statistically significant difference between the 2 groups for the different parameters on the first procedure. The results for each individual variable are also displayed on the graphs below (Figures 5 to 8):
Discussion
After a brief survey of the medical literature, it is noted that many studies are focused on the use of various simulation methods and the ability improvement resulting from them, not only in surgery, but in the entire medical field. Simulation is seen today as an important factor in medical education and it tends to be increasingly present in the teaching of students and residents, ensuring greater safety for patients1818. Gaba DM. The future vision of simulation in healthcare. Simul Healthc. 2007 Summer;2(2):126-35. PMID: 19088617..
There are many articles in the previously published literature that relate to the topic of simulation and training in laparoscopic surgery (416 in the last 5 years). However, only few studies assess the use of physical simulators and there is not a single paper similar to this that compares specifically the use of the LAP ETX A2 simulator for the benefit of learning. The vast majority of studies focused on the analysis and comparison between physical simulators and box trainers (black boxes)1919. Dehabadi M, Fernando B, Berlingieri P. The use of simulation in the acquisition of laparoscopic suturing skills. Int J Surg. 2014;12(4):258-68. PMID: 24503123.,2020. Khan MW, Lin D, Marlow N, Altree M, Babidge W, Field J, Hewett P, Maddern G Laparoscopic skills maintenance: a randomized trial of virtual reality and box trainer simulators. J Surg Educ. 2014 Jan-Feb;71(1):79-84. PMID: 24411428..
While performing the study, we were able to notice how the simulation exercise was beneficial for the students tested. The simulator proved to be an excellent method of learning, especially in regard to the anatomy and surgical steps of a laparoscopic cholecystectomy. Moreover, it was an excellent introduction to laparoscopic surgery instrumental and 2 dimensional vision that this method provides, which is undoubtedly one of the major obstacles to be surpassed by the young surgeons. During medical curriculum, medical students hardly have any real experiences and contact with laparoscopically and, when they do, they are mostly observers. Given that laparoscopy now occupies a prominent position in the surgical field, including being the preferred technique for many procedures2121. Pena Gonzalez JA, Pascual Queralt M, Salvador Bayarri JT, Rosales Bordes A, Palou Redorta J, Villavicencio Mavrich H. Evolution of open versus laparoscopic/robotic surgery: 10 years of changes in urology. Actas Urol Esp. 34(3):223-31. PMID: 20416238. medical students and surgical residents should be trained and introduced to this method as early and comprehensively as possible.
After statistical analysis, we observed that despite the best averages scores in virtually all analyzed parameters belonged to the test group, no statistically significant difference was found between the two groups performance. This result may be related to the small number of students tested in this study, which obviously decrease its statistical power. However, both the simulator and animal models are expensive, consequently limiting the number of participants.
As a downside of the simulator, we must emphasize that the hardened consistency of the synthetic tissue required higher drifts when performing maneuvers of dissection than the actual procedures requires. In addition, as the fabric is not easily separated with simple divulsion, the use of sharpened tweezers was required to advance trough tissues. On the other hand, the material proved to be excellent for training sutures.
Laparoscopy has been showing excellent results in the short and medium term throughout the years, being considered as the gold standard approach in several abdominal, urological and gynecological conditions2222. Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM; MRC CLASICC trial group. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718-26. PMID: 15894098.,2323. Lacy AM, Garcia-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359:2224-9. PMID: 12103285.. However, it is believed that the lack of appropriate programs and training methods is one of the major obstacles to the supremacy of this technique in some procedures, such as colectomy2424. Kemp JA, Finlayson SR. Nationwide trends in laparoscopic colectomy from 2000-2004. Surg Endosc. 2008;22:1181-7.PMID: 23598378..
As already stated, the use of animal models is increasingly costly both financially and morally for educational institutions. Although this model still plays a key role in training physicians and surgeons, being preferred by many residents by the similarity in texture of tissues, bleeding and ability to physically simulate the complications2525. Palter VN, Orzech N, Aggarwal R, Okrainec A, Grantcharov TP. Resident perceptions of advanced laparoscopic skills training. Surg Endosc. 2010;24:2830-4. PMID: 20428895.,2626. La Torre M, Caruso C. Resident training in laparoscopic colorectal surgery: role of the porcine model. World J Surg. 2012;36:2015-20. PMID: 22689021., the use of the physical simulator could significantly reduce the number of animals used, at least in regard to the gain of basic laparoscopic surgical skills. Therefore, the applicability of these simulators in the curriculum of the students and residents is certainly a topic that deserves attention.
Conclusion
We did not find any evidence of benefit in the use of the physical simulator for surgical performance in medical students.
References
-
1Litynski GS. Kurt Semm and the fight against skepticism: endoscopic hemostasis, laparoscopic appendectomy, and Semm's impact on the "laparoscopic revolution". JSLS. 1998 Jul-Sep.;2(3):309-13. PMID: 9876762.
-
2Bruhat MA, Chapron C, Mage G, Pouly JL, Canis M, Wattiez A, Glowaczower E. The benefits and risks of laparoscopic surgery. Rev Fr Gynecol Obstet. 1993;88(2):84-8. PMID: 8469869.
-
3Jonsson B, Zethraeus N. Costs and benefits of laparoscopic surgery--a review of the literature. Eur J Surg. 2000;Suppl(585):48-56. PMID: 10885558.
-
4Fingerhut A, Millat B, Borrie F. Laparoscopic versus open appendectomy: time to decide. World J Surg. 1999;23:835-845. PMID: 10415210.
-
5Sasi, W. Dissection by ultrasonic energy versus monopolar electrosurgical energy in laparoscopic cholecystectomy. JSLS. 2010 Jan-Mar;14(1):23-34. PMID: 20412640.
-
6Hoffman H, Vu D. Virtual reality: teaching tool of the twenty-first century? Acad Med. 1997 Dec;72(12):1076-81. PMID: 9435714.
-
7Hamilton EC, Scott DJ, Fleming JB, Rege RV, Laycock R, Bergen PC, Tesfay ST, Jones DB. Comparison of video trainer and virtual reality training systems on acquisition of laparoscopic skills. Surg Endosc. 2002 Mar;16(3):406-11. PMID: 11928017.
-
8Subramonian K, DeSylva S, Bishai P, Thompson P, Muir G. Acquiring surgical skills: a comparative study of open versus laparoscopic surgery. Eur Urol. 2004;45(3):346-51. PMID: 15036681.
-
9Uranüs S, Yanik M, Bretthauer G., Virtual reality in laparoscopic surgery. Stud Health Technol Inform. 2004;104:151-5. PMID: 15747974.
-
10Wanzel KR, Ward M, Reznick RK. Teaching the surgical craft: from selection to certification. Curr Probl Surg. 2002 Jun;39(6):573-659. PMID: 12037512.
-
11Hart R, Karthigasu K. The benefits of virtual reality simulator training for laparoscopic surgery. Curr Opin Obstet Gynecol. 2007 Aug;19(4):297-302. PMID: 17625408.
-
12Lehmann KS, Gröne J, Lauscher JC, Ritz JP, Holmer C, Pohlen U, Buhr HJ. Simulation training in surgical education - application of virtual reality laparoscopic simulators in a surgical skills course. Zentralbl Chir. 2012 Apr;137(2):130-7. PMID: 22495487.
-
13Kneebone R. Simulation in surgical training: educational issues and practical implications. Med Educ. 2003;37(3):267-77. PMID: 12603766.
-
14Feldman LS, Sherman V, Fried GM. Using simulators to assess laparoscopic competence: ready for widespread use? Surgery. 2004;135(1):28-42. PMID: 14694298.
-
15Tokarczyk AJ, Greenberg SB. Use of mannequin-based simulators in anesthesiology. Dis Mon. 2011 Nov;57(11):706-14. PMID: 22082556.
-
16da Cruz JA, Sandy NS, Passerotti CC, Nguyen H, Antunes AA, Dos Reis ST, Dall'Oglio MF, Duarte RJ, Srougi M. Does training laparoscopic skills in a virtual reality simulator improve surgical performance? J Endourol. 2010 Nov;24(11):1845-9. PMID: 20958203.
-
17Vassiliou MC, Feldman LS, Andrew CG, Bergman S, Leffondre K, Stanbridge D, Fried GM. A global assessment tool for evaluation of intraoperative laparoscopic skills. Am J Surg. 2005 Jul;190(1):107-13. PMID: 15972181.
-
18Gaba DM. The future vision of simulation in healthcare. Simul Healthc. 2007 Summer;2(2):126-35. PMID: 19088617.
-
19Dehabadi M, Fernando B, Berlingieri P. The use of simulation in the acquisition of laparoscopic suturing skills. Int J Surg. 2014;12(4):258-68. PMID: 24503123.
-
20Khan MW, Lin D, Marlow N, Altree M, Babidge W, Field J, Hewett P, Maddern G Laparoscopic skills maintenance: a randomized trial of virtual reality and box trainer simulators. J Surg Educ. 2014 Jan-Feb;71(1):79-84. PMID: 24411428.
-
21Pena Gonzalez JA, Pascual Queralt M, Salvador Bayarri JT, Rosales Bordes A, Palou Redorta J, Villavicencio Mavrich H. Evolution of open versus laparoscopic/robotic surgery: 10 years of changes in urology. Actas Urol Esp. 34(3):223-31. PMID: 20416238.
-
22Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM; MRC CLASICC trial group. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718-26. PMID: 15894098.
-
23Lacy AM, Garcia-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359:2224-9. PMID: 12103285.
-
24Kemp JA, Finlayson SR. Nationwide trends in laparoscopic colectomy from 2000-2004. Surg Endosc. 2008;22:1181-7.PMID: 23598378.
-
25Palter VN, Orzech N, Aggarwal R, Okrainec A, Grantcharov TP. Resident perceptions of advanced laparoscopic skills training. Surg Endosc. 2010;24:2830-4. PMID: 20428895.
-
26La Torre M, Caruso C. Resident training in laparoscopic colorectal surgery: role of the porcine model. World J Surg. 2012;36:2015-20. PMID: 22689021.
-
Financial source:
FAPESP
-
1
Research performed at Laboratory of Medical Research, Urology - LIM 55, Medical School, Universidade de São Paulo (USP), Brazil.
Publication Dates
-
Publication in this collection
Jan 2018
History
-
Received
08 Sept 2017 -
Reviewed
10 Nov 2017 -
Accepted
11 Dec 2017