Abstract
The patient is a 5-year-old male with Kawasaki disease, whose involution of giant aneurysms of the left coronary arteries was surprising after a prolonged period of treatment, which lasted 80 uninterrupted days and comprised anti-inflammatory drugs associated with anticoagulation agents. The distal diameters of the anterior interventricular, the diagonal, and the circumflex arteries normalized by the end of the treatment. A residual giant aneurysm localized at the beginning of the anterior interventricular artery did not cause ischemia. Continuation of the medication for a prolonged period was recommended.
CASE REPORT
Kawasaki disease. Involution of giant coronary aneurysms after prolonged anti-inflammatory treatment
Edmar Atik; Antonio Foronda; Luiz Narcio P. Bustamante
Instituto do Coração da Faculdade de Medicina da Universidade de São Paulo
Correspondence Correspondence to Edmar Atik InCor Av. Enéas C Aguiar,44 05403-000 - São Paulo,SP E-mail: conatik@incor.usp.br
The patient is a 5-year-old male with Kawasaki disease, whose involution of giant aneurysms of the left coronary arteries was surprising after a prolonged period of treatment, which lasted 80 uninterrupted days and comprised anti-inflammatory drugs associated with anticoagulation agents. The distal diameters of the anterior interventricular, the diagonal, and the circumflex arteries normalized by the end of the treatment. A residual giant aneurysm localized at the beginning of the anterior interventricular artery did not cause ischemia. Continuation of the medication for a prolonged period was recommended.
Kawasaki disease, known since 1976 1, has some evolutional characteristics that deserve mention 2-6, among which is the reduction in coronary aneurysms with adequate anti-inflammatory treatment, which causes radical change both in the size and extension of the aneurysm, except for the rare regression of giant aneurysms 2,3,6. This involution is possible and may even be significant in some cases. Therefore, in the acute phase of the disease, surgical indication, which is limited to the presence of significant dysfunction or myocardial ischemia, or both, should be very carefully considered 4,5.
We report a case of significant involution of giant coronary aneurysms with treatment.
Case Report
The patient is a 5-year-old male with findings suggestive of Kawasaki disease in the preceding 2 months, characterized by fever, enlargement of cervical lymph nodes, and tonsillitis, followed by generalized cutaneous erythema, pruritus, and edema of the limbs after a few days, and desquamation on the 10th day. The laboratory tests indicated an active inflammatory phase with an elevated sedimentation rate of 100 mm during the first minute, C-reactive protein of 50 U, leukocytosis of 12000/mm3, and, approximately 10 days later, an increased number of platelets (540000/mm3). Despite the treatment with acetylsalicylic acid (80mg/kg/day), gamma globulin (2g/kg) on the forth and seventh days, in addition to general measures, the patient developed giant aneurysms in the anterior interventricular, circumflex, and right coronary arteries. These aneurysms were detected in the initial third of the cited arteries on echocardiography (fig. 1) approximately 33 days after the beginning of the disease and were confirmed on coronary angiographic study on the 46th day of evolution, in which the right coronary artery was obstructed and filled retrogradely from the left coronary artery. The left arteries were significantly dilated halfway up their trajectories, and saccular aneurysms continued the anterior interventricular artery up to the left ventricular tip. The diagonal artery was slightly impaired (fig. 2).
Due to persistence of the elevated sedimentation rate and C-reactive protein, the treatment with high doses of acetylsalicylic acid was reinitiated on the 47th day after the beginning of the disease, interrupted on the 17th day due to gastric irritation. Laboratory tests became normal 20 days after the restart of medication, which, however, was purposely continued for 2 more months at high doses, aiming at increasing the possibility of regression of the coronary inflammatory phenomena. As the patient was asymptomatic, myocardial revascularization surgery and even cardiac transplantation, which were considered before the patient's referral to our service, were ruled out.
The patient underwent anti-inflammatory treatment associated with full anticoagulation for 80 uninterrupted days, because of his tolerance to the medication.
Myocardial perfusion with MIBI after exercise testing, during which a submaximal heart rate of 180 bpm was obtained, was adequate, and no myocardial perfusion alteration was observed. Normal ventricular function with an ejection fraction of 78% was assessed on radioisotopic ventriculography and also confirmed on echocardiography with fiber shortening fraction of 35%. The conventional electrocardiogram remained normal, as did chest radiography, which had shown no abnormalities in regard to heart size and pulmonary vasculature since the beginning of the disease.
The patient was hospitalized for more than 4 months, due to the potential risks of the coronary aneurysms.
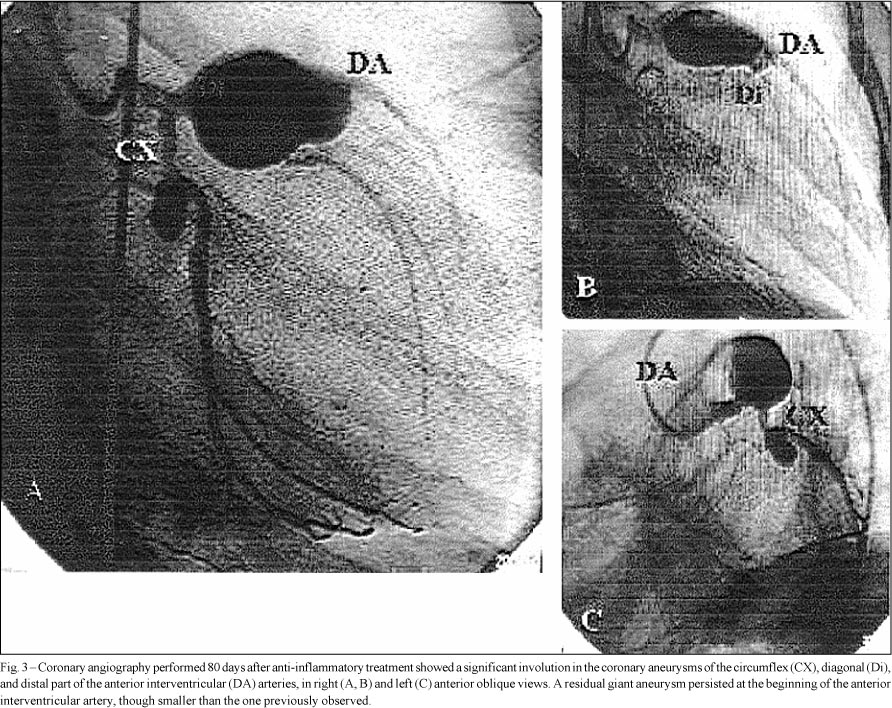
At the end of that period and of the prolonged anti-inflammatory treatment, cardiac catheterization was repeated and showed a surprising involution of the aneurysms of the circumflex artery and of the distal part of the anterior interventricular and diagonal arteries; however, a giant aneurysm remained at the beginning of the anterior interventricular artery before the emergence of the diagonal artery (fig. 3).
High doses of acetylsalicylic acid in association with anticoagulation therapy were maintained for a longer period due to the patient's evolution, in an attempt to achieve a greater regression of the aneurysm, which was then located in the anterior interventricular artery. A future surgical approach will be considered in the presence of an ischemic process or eventual worsening of the aneurysm, or both, which will be monitored through myocardial perfusion with MIBI and also another angiographic study.
Discussion
The involution of coronary aneurysms in Kawasaki disease is well known 2,3,6. According to Oki et al 6, in a study assessing 1,594 patients with that disease, coronary aneurysms were found in 162 (10.2%) patients in the acute phase, and, after a 12-month follow-up, the number of patients with aneurysms decreased to only 67 (4.2%). Still in that study 6, giant aneurysms were reported in 10 (6.1%) of the 162 patients in the acute phase, its mortality being 30%, which contrasted with the good evolution of the other patients with smaller aneurysms.
Due to the well-known involution of aneurysms 2,3, no precipitate management is recommended in the acute phase of the disease, even in the presence of giant aneurysms, unless the ventricular dysfunction requires urgent action. Another element guiding the approach in this phase is myocardial ischemia diagnosed through methods of myocardial perfusion with MIBI or thallium after physical activity or pharmacological testing with dipyridamole or adenosine. This monitoring determines the approach, which may be conservative in cases of good myocardial perfusion, or surgical, or even interventional cardiac catheterization, due to the presence of an ischemic process 4,5.
In the acute phase of Kawasaki disease, a greater surgical risk exists, because, in the presence of inflammation, the anastomosis with an inflamed coronary artery runs the risk of obstruction, in addition to exacerbation of the distal stenoses.
Due to the good clinical evolution of most patients with Kawasaki disease, caution is a very important general measure in the management of these patients 2,3,6.
On the other hand, the surgical approach is equally stimulating because of its adequate results, but it should be restricted to patients with giant aneurysms or ischemic processes after the acute phase of the disease 4,5.
Whether the anti-inflammatory medication administered for a prolonged period had an influence in the peculiar evolution of this patient is a matter of conjecture. This is due to the fact that the treatment was extended even beyond normalization of the blood markers for inflammation, based on the treatment duration of other autoimmune inflammatory processes, such as the diffuse diseases of the connective tissue, among which is rheumatic disease. Patients treated with high doses of anti-inflammatory medication are always under the potential risk of digestive hemorrhage, which, when present, requires interruption of the medication; this, however, did not happen to our patient.
The evident protection provided by gamma globulin in preventing coronary alterations is noteworthy, although its beneficial effect was not observed in the present case. The use of gamma globulin has become mandatory in the first 10 days of the disease, with a consequent reduction in the incidence of coronary aneurysms, which dropped from 16% to 4% of the cases reported in the literature 7,8, stressing the need for the early diagnosis of the disease.
In our experience, when we began to administer gamma globulin at the beginning of the disease, a reduction in the incidence of coronary aneurysms from 27% to 4% was observed in 291 children treated from 1980 onwards 9. In that sample, giant aneurysms were detected in 13 patients and they did not clear up. The evidence of involution of a giant aneurysm, like that observed in the case here reported, is very rare, occurring in approximately 1% of the cases, according to the literature 6,9.
Acknowledgments
We thank Drs. Luiz Kajita and José Carlos Brito for the angiographic studies, Drs. William Chalela and José Soares Jr. for the radioisotopic study, and Drs. Gláucia Tavares and Lúcia Duarte for the echocardiographic studies.
Recebido para publicação em 31/7/02
Aceito em 20/11/02
Received - 7/31/02
Accepted - 11/20/02
- 1. Kawasaki T. Discovery of Kawasaki disease (muco-cutaneous lymph node syndrome) and its research activities. Nippon Rinsho 1976;34:222-7.
- 2. Chang RK. Hospitalizations for Kawasaki disease among children in the United States, 1988-1997. Pediatrics 2002; 109: 87.
- 3. Chantepie A, Mauran P, Lusson JR, Vaillant MC, Bozio A. Cardiovascular complications of Kawasaki syndrome: results of a French multicenter study. Arch Pediatr 2001;8: 713-9.
- 4. Yoshikawa Y, Yagihara T, Kameda Y, et al. Result of surgical treatments in patients with coronary-arterial obstructive disease after Kawasaki disease. Eur J Cardiovasc Surg 2000;17:515-9.
- 5. Gotteiner N, Mavroudis C, Backer CL, et al. Coronary artery bypass grafting for Kawasaki disease. Pediatr Cardiol 2002;23:62-7.
- 6. Oki I, Tanihara S, Ojima T, Nakamura Y, Yanagawa H. A multicenter collaborative study on the risk factors of cardiac sequelae due to Kawasaki disease: a one-year follow-up study. Acta Pediatr 2000;89:1435-8.
- 7. Burns JC, Capparelli EV, Brown JA, Newburger JW, Glode MP. Intravenous gamma-globulin treatment and retreatment in Kawasaki disease. Pediatr Infect Dis J, 1998; 17:1144-8.
- 8. Tse SML, Silverman ED, McCrindle BW, Yeung RSM. Early treatment with intravenous immunoglobulin in patients with Kawasaki disease. J Pediatr 2002;140:450-5.
- 9. Foronda A, Sakane PT. Cardiac alterations in the Kawasaki disease. Cardiol Young, in press.
Publication Dates
-
Publication in this collection
09 Oct 2003 -
Date of issue
Sept 2003
History
-
Accepted
20 Nov 2002 -
Received
31 July 2002