ABSTRACT
Lack of stroke awareness and slow activation of emergency medical services (EMS) are frequently reported reasons for delayed arrival to the hospital. We evaluated these variables in our population.
Methods
Review of hospital records and structured telephone interviews of 100 consecutive stroke patients. Forward stepwise logistic regression was used for the statistical analysis.
Results
Seventy patients (75%) arrived at the hospital 4.5 hours after stroke symptoms onset. The use of EMS did not improve arrival times. Most patients who recognized their symptoms did not use EMS (p < 0.02). Nineteen patients (20%) were initially misdiagnosed. Eighteen of them were first assessed by non-neurologist physicians (p < 0.001).
Conclusions
Our population showed a low level of stroke awareness. The use of EMS did not improve arrival times at the hospital and the non-utilization of the EMS was associated with the recognition of stroke symptoms. There was a concerning rate of misdiagnosis, mostly by non-neurologist medical providers.
stroke; emergency medical system
RESUMO
La falta de reconocimiento de los síntomas del accidente cerebrovascular (ACV) y la lenta activación de los servicios de emergencias médicos (SEM) son causas frecuentes de demoras en el arribo hospitalario. Nuestro objetivo fue evaluar ambas variables en nuestra población.
Métodos
Revisión de registros hospitalarios y entrevista telefónica estructurada de 100 pacientes consecutivos internados por ACV. El análisis estadístico se realizó mediante un modelo de regresión logística multivariada por pasos.
Resultados
Setenta pacientes (75%) arribaron al hospital luego de 4.5 horas del comienzo de los síntomas. El uso de los SEM no mejoró los tiempos de arribo al hospital (p < 0.02). Inicialmente, 19 pacientes (20%) recibieron un diagnóstico erróneo. Dieciocho de ellos fueron evaluados por médicos no neurólogos. (p < 0.001).
Conclusiones
El reconocimiento de los síntomas de ACV en nuestra población fue bajo. El uso de los SEM no mejoró los tiempos de arribo hospitalario y la no utilización de los mismos se asoció con el correcto reconocimiento de los síntomas por parte de los pacientes. La proporción de diagnósticos erróneos fue preocupante, fundamentalmente entre médicos no neurólogos.
accidente cerebrovascular; servicios de emergencias médico
Stroke is the second leading cause of mortality and the third cause of disability worldwide11. Feigin VL, Forouzanfar MH, Krishnamurthi R, R, Mensah GA, Connor M, Bennett DA et al. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet . 2014;383(9913):245-54. doi:10.1016/S0140-6736(13)61953-4
https://doi.org/10.1016/S0140-6736(13)61...
,22. Murray CJL, Lopez AD. Measuring the global burden of disease. N Engl J Med. 2013;369(5):448-57. doi:10.1056/NEJMra1201534
https://doi.org/10.1056/NEJMra1201534...
. With the aging of populations, concern is growing about a potentially larger impact of the stroke burden on public health33. Cadilhac DA, Carter RC, Thrift AG, Dewey HM. Why invest in a national public health program for stroke? An example using Australian data to estimate the potential benefits and cost implications. Health Policy. 2007;83(2-3):287-94. doi:10.1016/j.healthpol.2007.02.001
https://doi.org/10.1016/j.healthpol.2007...
,44. Dewey HM, Thrift AG, Mihalopoulos C, Carter R, Macdonell RA, McNeil JJ et al. ‘Out of pocket’ costs to stroke patients during the first year after stroke – results from the North East Melbourne Stroke Incidence Study. J Clin Neurosci. 2004;11(2):134-7. doi:10.1016/S0967-5868(03)00148-6
https://doi.org/10.1016/S0967-5868(03)00...
. This impact can be diminished by early thrombolytic treatment as this reduces disability and improves outcomes after ischemic stroke55. Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384(9958):1929-35. doi:10.1016/S0140-6736(14)60584-5
https://doi.org/10.1016/S0140-6736(14)60...
.
The principal reason for non-use of IV rtPA is delayed arrival time at the hospital66. Rosamond WD, Gorton R, Hinn R, Hohenhaus SM, Morris DL. Rapid response to stroke symptoms: the Delay in Accessing Stroke Healthcare (DASH) study. Acad Emerg Med. 1998;5(1):45-51. doi:10.1111/j.1553-2712.1998.tb02574.x
https://doi.org/10.1111/j.1553-2712.1998...
. Causes for this delay may be specific to particular characteristics of each population, however lack of recognition of stroke symptoms and slow activation and response of emergency medical services (EMS) are frequently reported reasons77. Feldmann E, Gordon N, Brooks JM, Brass LM, Fayad PB, Sawaya KL et al. Factors associated with early presentation of acute stroke. Stroke. 1993;24(12):1805-10. doi:10.1161/01.STR.24.12.1805
https://doi.org/10.1161/01.STR.24.12.180...
,88. Williams LS, Bruno A, Rouch D, Marriott DJ, Mas DJ. Stroke patients’ knowledge of stroke : influence on time to presentation. Stroke. 1997;28(5):912-5. doi:10.1161/01.STR.28.5.912
https://doi.org/10.1161/01.STR.28.5.912...
,99. Wester P, Rådberg J, Lundgren B, Peltonen M. Factors associated with delayed admission to hospital and in-hospital delays in acute stroke and TIA: a prospective, multicenter study. Seek- Medical-Attention-in-Time Study Group. Stroke. 1999;30(1):40-8. doi:10.1161/01.STR.30.1.40
https://doi.org/10.1161/01.STR.30.1.40...
,1010. Clark JM, Renier, Sa. A community stroke study: factors influencing stroke awareness and hospital arrival time. J Stroke Cerebrovasc Dis. 2001;10(6):274-8. doi:10.1053/jscd.2001.123774
https://doi.org/10.1053/jscd.2001.123774...
,1111. Schroeder EB, Rosamond WD, Morris DL, Evenson KR, Hinn AR. Determinants of use of emergency medical services in a population with stroke symptoms : The Second Delay in Accessing Stroke Healthcare (DASH II) Study. Stroke. 2000;31(11):2591-6. doi:10.1161/01.STR.31.11.2591
https://doi.org/10.1161/01.STR.31.11.259...
.
Information about the recognition of stroke symptoms, the role of EMS for stroke patients’ transportation and their impact on arrival times in Latin America is scant. Data from Brazil show an alarming lack of knowledge of stroke symptoms and activation of EMS in the general population1212. Pontes-Neto OM, Silva GS, Feitosa MR, Figueiredo NL, Fiorot Jr JA, Rocha TN et al. Stroke awareness in Brazil: alarming results in a community-based study. Stroke. 2008;39(2):292-6. doi:10.1161/STROKEAHA.107.493908
https://doi.org/10.1161/STROKEAHA.107.49...
,1313. Nóvak EM, Zétola VHF, Muzzio JA, Puppi M, Carraro Júnior H, Werneck LC. [Lay knowledge about stroke]. Arq Neuropsiquiatr. 2003;61(3B):772-6. Portuguese. doi:10.1590/S0004-282X2003000500013
https://doi.org/10.1590/S0004-282X200300...
. However, there are no studies exploring this topic in patients with prior stroke1414. Hawkes MA, Ameriso SF, Willey JZ. Stroke knowledge in Spanish-speaking populations. Neuroepidemiology. 2015;44(3):121-9. doi:10.1159/000381100
https://doi.org/10.1159/000381100...
.
In Argentina, where thrombolytic therapy is not widely utilized, we hypothesize that low stroke awareness in the general population and in non-neurologist medical providers, as well as the lack of a rapid referral system for stroke care may negatively impact arrival times at hospital, negatively affecting the use of thrombolytic therapy.
Our aim was to evaluate the pattern of recognition of stroke symptoms, utilization of EMS and their impact on arrival times at the hospital in our population.
METHODS
This was a retrospective review of hospital records and prospective structured telephone interviews of 100 consecutive patients admitted to the stroke unit of our institution with a diagnosis of acute ischemic stroke from November 2012 to July 2013. As several studies suggest that the population awareness and response to transient symptoms are different1515. Sprigg N, Machili C, Otter ME, Wilson A, Robinson TG. A systematic review of delays in seeking medical attention after transient ischaemic attack. J Neurol Neurosurg Psychiatry. 2009;80(8):871-5. doi:10.1136/jnnp.2008.167924
https://doi.org/10.1136/jnnp.2008.167924...
, transient ischemic attacks (TIAs) were excluded from this study. Patients or caregivers were contacted by a neurologist and questioned about their interpretation of their symptoms, and subsequent response, using a predesigned standardized questionnaire (Figure 1). Time between admission and phone contact was from one to seven months.
Population
Patients were selected from hospital records of tertiary neurological hospital of the city of Buenos Aires. Its stroke unit admits approximately 180 patients with ischemic stroke per year.
According to a 2010 national census, the city of Buenos Aires has 2.9 million habitants. The educational level, socioeconomic status and private healthcare coverage in this population is higher than the average in Argentina1616. Programa de las Naciones Unidas para el Desarrollo – PNUD. El sistema de salud argentino y su trayectoria de largo plazo: logros alcanzados y desafíos futuros. Buenos Aires: Programa de las Naciones Unidas para el Desarrollo ; 2011. (Aportes para el desarrollo humano en Argentina 2011, vol 6).. Besides being a regional referral center, approximately 260,000 people, mostly those with private health insurance, are within the influence area and have access to acute stroke care in our hospital.
Health care system
The health care system in Argentina is segmented and heterogeneous because of the lack of integration between the public system, social security and private sector. It is based on the public provision of health for every habitant. Additionally, people can be covered by the social security system comprising workers’ organizations “health care insurance” (52%), government-funded social insurance for the retired population “PAMI” (8.3%), or by private health insurances (9%)1616. Programa de las Naciones Unidas para el Desarrollo – PNUD. El sistema de salud argentino y su trayectoria de largo plazo: logros alcanzados y desafíos futuros. Buenos Aires: Programa de las Naciones Unidas para el Desarrollo ; 2011. (Aportes para el desarrollo humano en Argentina 2011, vol 6).. The latter, in turn, subcontract to emergency medical companies.
Definitions
Stroke was defined as an acute focal neurological deficit lasting more than 24 hours. The word used to refer to stroke in the Spanish version of the questionnaire was ACV, the acronym of “accidente cerebrovascular” (cerebrovascular accident). A TIA was considered to be an acute neurological deficit lasting < 24 hours with a normal physical examination beyond that time. Patients who were referred with transient symptoms but had abnormal findings on the neurological examination were considered stroke patients.
As IV rtPA efficacy decreases in a time-dependent fashion up to 4.5 hours after symptom onset and endovascular treatments can be used in selected patients within six hours, arrival time was segmented into 3, 4.5 and 6 hours between stroke onset and presentation at the emergency room, for the purpose of data analysis. To investigate the causes for which patients could not even be considered for IV rtPA treatment, patients who arrived to hospital after 4.5 hours from stroke onset were considered to have pre-hospital delay (PHD) and those who arrived to the hospital before 4.5 hours but had completed initial work-up beyond that time, were considered to have hospital diagnosis delay (HDD).
Arrival time was defined as the last time the patient was asymptomatic until arrival at hospital. If the patients were transferred from another institution, arrival time was considered to be from the onset of stroke symptoms until arrival at the first center. The term “non-specialized hospital” was used to describe centers not meeting criteria for a primary stroke center1717. Alberts MJ, Latchaw RE, Jagoda A, Wechsler LR, Crocco T, George MG et al. Revised and updated recommendations for the establishment of primary stroke centers: a summary statement from the brain attack coalition. Stroke. 2011;42(9):2651-65. doi:10.1161/STROKEAHA.111.615336
https://doi.org/10.1161/STROKEAHA.111.61...
.
We defined “educational level” as the highest level of schooling that a person has reached. It was stratified as completed elementary school, completed secondary school or university education. Patients who had an incomplete level were allocated to the immediate lower group.
Statistical analysis
Regression analysis was performed with EMS utilization and emergency consultation as outcomes. Other variables included and/or considered potential confounders were age, gender, educational level, neighborhood, previous knowledge about stroke, history of neurological symptoms, family history of stroke, previous inpatient admission, heart disease, presence of motor or sensory symptoms, facial weakness and National Institutes of Health Stroke Scale (NIHSS) score at admission. Forward stepwise logistic regression analysis was used to determine which factors correlated with the odds of calling EMS or going to the emergency by their own means. Univariate analysis was performed for each variable and tests with p values < 0.25 were ranked and kept for the next step. Age, gender, and educational level were added regardless of their p value. We then added, as a first variable, the one having the highest correlation with the dependent variable and, if it was significant, we continued with the next variable until no more were available. Partial F tests were conducted at every step, and non-significant variables were removed. Fisher’s exact test was used to estimate statistical significance of the categorical data. The local ethics committee approved the study.
RESULTS
Five patients were lost to follow up and one had died. Thus, 84 patients and 10 caregivers completed the telephone survey and were included in the final analysis.
Demographic characteristics
Mean age was 67 ± 20 years old. Sixty-four percent of patients were male. All patients had at least completed elementary school and 55% had completed college education. Thirty percent had had a stroke before the index event and 24% had relatives with stroke (Table 1). Initial symptoms and NIHSS scores on admission are presented in Table 2.
Arrival times, pre-hospital delay and hospital diagnostic delay
Seventy patients (75%) arrived at the hospital more than 4.5 hours after onset of the stroke. Those patients were considered to have PHD. The principal causes were lack of recognition of symptoms as indicators of acute stroke and mild or transient symptoms (Table 2).
Twenty-four patients (25%) arrived at the emergency room within 4.5 hours from stroke onset, half of them (n = 12) within 3 hours. Four of those patients had their initial work-up completed more than 4.5 hours after stroke symptoms and did not receive rtPA. They were considered to have HDD. Causes of initial HDD were misdiagnosis in three patients and unavailability of brain imaging in one. All HDD patients were referred to our center after their first evaluation in non-specialized hospitals. The referral time was less than 24 hours in all cases. Nineteen patients (20%) were initially misdiagnosed. Eighteen of them were first assessed by a non-neurologist physician (p < 0.001).
Pattern of utilization of EMS
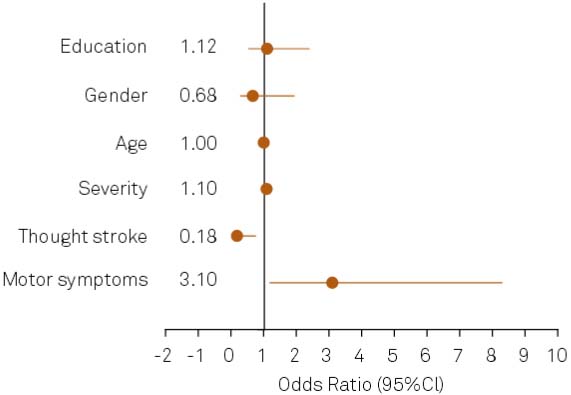
The EMS were used by 37% of patients without a significant impact on arrival time. Most patients who recognized their symptoms did not use EMS for transportation to the hospital (p < 0.02) (Figure 2). Patients with motor symptoms were more likely to use EMS (p < 0.02) (Figure 2). Also stroke severity, measured by the NIHSS, was associated with the use of the EMS. For each point of the NIHSS score, the chance of calling the EMS increased by 10%. Fifty-five percent of patients referred that they had received information about stroke before their event; however this did not make them more prone to call the EMS.
IV rtPA treatment and transportation to the hospital
Ten patients (10.6%) received IV rtPA treatment. Most of them (n = 7) arrived within three hours from stroke symptom onset. Seven out of ten treated subjects did not use the EMS and came to our emergency in their own transportation or hired vehicles.
Interpretation of stroke symptoms
Only 21% of the patients interpreted their initial symptoms as consistent with stroke. This group was more likely to arrive within six hours (adjusted OR 2.96 95%CI 1–8.7 p < 0.05). Also a trend in the odds of consultation in the first three, and four-and-a-half hours was found among them, but this did not reach statistical significance. Motor symptoms and speech disturbances were the most frequently-recognized symptoms. There was no relationship between past history of stroke or higher educational level and the correct interpretation of symptoms.
Patients with visual symptoms tended to consult at ophthalmological medical institutions first (adjusted OR 0.11, 95%CI 0, 02–0.55, p < 0.01) and those with prior stroke came directly to our institution (adjusted OR 5.8, 95%CI 1.81–18.6, p < 0.01)
DISCUSSION
Compared with prior studies1414. Hawkes MA, Ameriso SF, Willey JZ. Stroke knowledge in Spanish-speaking populations. Neuroepidemiology. 2015;44(3):121-9. doi:10.1159/000381100
https://doi.org/10.1159/000381100...
, our population showed a higher educational level. All individuals had at least completed elementary school and 55% had a college degree. In this population, economic and educational levels may be higher than the average in Argentina1616. Programa de las Naciones Unidas para el Desarrollo – PNUD. El sistema de salud argentino y su trayectoria de largo plazo: logros alcanzados y desafíos futuros. Buenos Aires: Programa de las Naciones Unidas para el Desarrollo ; 2011. (Aportes para el desarrollo humano en Argentina 2011, vol 6). and in other Latin American populations. However, we did not find an association between educational level and correct stroke symptom interpretation or proper use of EMS.
Only 21% of patients recognized their initial symptoms as consistent with stroke. This percentage is lower than previous reports in Spanish speakers1414. Hawkes MA, Ameriso SF, Willey JZ. Stroke knowledge in Spanish-speaking populations. Neuroepidemiology. 2015;44(3):121-9. doi:10.1159/000381100
https://doi.org/10.1159/000381100...
. Recognition of stroke symptoms tripled the chances of consultation in the first six hours from symptom onset. A trend in the odds of consultation in first three and 4.5 hours was also found among those who recognized their symptoms as stroke, but without reaching statistical significance. Similar findings have been previously published in Spain1414. Hawkes MA, Ameriso SF, Willey JZ. Stroke knowledge in Spanish-speaking populations. Neuroepidemiology. 2015;44(3):121-9. doi:10.1159/000381100
https://doi.org/10.1159/000381100...
. It is remarkable that, despite most people seem not to acknowledge that they were having a stroke, they did know something was wrong enough to go to the hospital.
About 37% of subjects used the EMS, suggesting poor knowledge of its availability, lack of confidence in this system, and/or prior poor experience with its utilization. The association between motor symptoms and stroke severity and use of EMS suggests that, in this population, the reasons to call the ambulance were mainly physical difficulties in using their own transportation.
Counterintuitively, the use of the EMS was not associated with shorter arrival times. Moreover, most patients who acknowledged they were having a stroke and who were later treated with IV rtPA did not use EMS for transportation. Although this finding neither demonstrates a negative impact on EMS, nor points towards a recommendation for not using them, it does raise several areas for future analysis.
In Argentina, possibly less than 1% of patients with acute stroke receive IV thrombolysis, and this is mainly in private centers1818. Atallah AM, Fustinoni O, Zurru M, Beigelman R, Cirio J, Ameriso S et al. Identifying barriers in acute stroke therapy in Argentina. ARENAS Registry. Neurology. 2014;82(10 Suppl):P2.014.,1919. Sposato LA, Esnaola MM, Zamora R, Zurrú MC, Fustinoni O, Saposnik G. Quality of ischemic stroke care in emerging countries: the Argentinian National Stroke Registry (ReNACer). Stroke. 2008;39(11):3036-41. doi:10.1161/STROKEAHA.108.521062
https://doi.org/10.1161/STROKEAHA.108.52...
. Emergency services not being focused on diagnosis, triage and rapid transportation of possible candidates for IV rtPA treatment can, at least in part, be responsible for this. Buenos Aires does not have an organized system of stroke care and predefined protocols for rapid referral of patients to stroke centers. Further studies are needed to establish if EMS are playing a detrimental role in the rates of thrombolysis compared to patients who did not use them.
In contrast to the average thrombolysis rate reported in Argentina, this group had a high rate of thrombolysis (10%). This reflects the advantage of access to specialized stroke care in this region, as well as the potential selection bias of a group of patients from a single private hospital.
Prior stroke or TIA has been associated with recognition of stroke symptoms in several studies2020. Díez-Ascaso O, Martinez-Sánchez P, Fuentes B, Díez-Tejedor E. Sociocultural study on the self-perception of stroke and an analysis of doctor-patient communication. Neurologia. 2011;26(2):81-91. doi:10.1016/j.nrl.2010.09.017
https://doi.org/10.1016/j.nrl.2010.09.01...
,2121. Palomeras Soler E, Fossas Felip P, Quintana Luque M, Monteis Cahis R, Sebastián Salvatierra M, Fábregas Casarramona C et al. [Knowledge about stroke symptoms and attitude towards them in the population]. Neurologia. 2007;22(7):434-40. Spanish.,2222. Geffner D, Soriano C, Pérez T, Vilar C, Rodríguez D. Delay in seeking treatment by patients with stroke: who decides, where they go, and how long it takes. Clin Neurol Neurosurg. 2012;114(1):21-5. doi:10.1016/j.clineuro.2011.08.014
https://doi.org/10.1016/j.clineuro.2011....
. Differing from them, we did not find this association. Our finding may reflect a lack of education about stroke as part of secondary prevention programs.
Frequent misdiagnosis of stroke has been described among non-neurologist medical providers2323. Harbison J, Hossain O, Jenkinson D, Davis J, Louw SJ, Ford GA. Diagnostic accuracy of stroke referrals from primary care, emergency room physicians, and ambulance staff using the face arm speech test. Stroke. 2002;34(1):71-6. doi:10.1161/01.STR.0000044170.46643.5E
https://doi.org/10.1161/01.STR.000004417...
. The presence of a neurologist in the emergency room has been proposed as a solution to improve this situation2424. Moulin T, Sablot D, Vidry E, Belahsen F, Berger E, Lemounaud P et al. Impact of emergency room neurologists on patient management and outcome. Eur Neurol. 2003;50(4):207-14. doi:10.1159/000073861
https://doi.org/10.1159/000073861...
. Overall, 20% of patients in our study were initially misdiagnosed in non-specialized hospitals or EMS, this being the principal cause of HDD and a cause of PHD. Additionally, nine subjects arrived at the emergency department in under 4.5 hours from symptoms onset despite having been initially misdiagnosed. Misdiagnosis was evident almost exclusively among non-neurologists physicians. This point is particularly concerning given that only 8.4% of patients with stroke are initially evaluated by a neurologist in Argentina1818. Atallah AM, Fustinoni O, Zurru M, Beigelman R, Cirio J, Ameriso S et al. Identifying barriers in acute stroke therapy in Argentina. ARENAS Registry. Neurology. 2014;82(10 Suppl):P2.014..
Our study has some limitations. Patients were contacted one to seven months after the index stroke. This may have introduced a recall bias. However, the recognition of stroke symptoms was poor even assuming that a recall bias could falsely increase the percentage of patients claiming correct stroke awareness. Additionally, excluding the questionnaire, data used for the analysis was taken from hospital records and it was not affected by this bias. Also, we did not obtain firsthand information for 16 subjects, five were lost to follow up, one died and 10 subjects were unable to answer. In the last group, caregivers were contacted to help with the responses.
In conclusion, even in subjects with high economic and educational level, these results suggest low stroke awareness in our population. Educational programs about stroke warning symptoms as part of secondary prevention strategies for stroke patients are needed to improve early recognition in this high-risk population, given that prior stroke does not improve the recognition of new events.
The role and procedures of EMS in Argentina should be revised as their use did not improve arrival times at the hospital. Also, stroke symptom recognition was associated with the non-utilization of EMS.
Lastly, misdiagnosis by non-neurologist medical providers is concerning. Programs to address stroke knowledge among them are needed to plan future educational interventions.
References
-
1Feigin VL, Forouzanfar MH, Krishnamurthi R, R, Mensah GA, Connor M, Bennett DA et al. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet . 2014;383(9913):245-54. doi:10.1016/S0140-6736(13)61953-4
» https://doi.org/10.1016/S0140-6736(13)61953-4 -
2Murray CJL, Lopez AD. Measuring the global burden of disease. N Engl J Med. 2013;369(5):448-57. doi:10.1056/NEJMra1201534
» https://doi.org/10.1056/NEJMra1201534 -
3Cadilhac DA, Carter RC, Thrift AG, Dewey HM. Why invest in a national public health program for stroke? An example using Australian data to estimate the potential benefits and cost implications. Health Policy. 2007;83(2-3):287-94. doi:10.1016/j.healthpol.2007.02.001
» https://doi.org/10.1016/j.healthpol.2007.02.001 -
4Dewey HM, Thrift AG, Mihalopoulos C, Carter R, Macdonell RA, McNeil JJ et al. ‘Out of pocket’ costs to stroke patients during the first year after stroke – results from the North East Melbourne Stroke Incidence Study. J Clin Neurosci. 2004;11(2):134-7. doi:10.1016/S0967-5868(03)00148-6
» https://doi.org/10.1016/S0967-5868(03)00148-6 -
5Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384(9958):1929-35. doi:10.1016/S0140-6736(14)60584-5
» https://doi.org/10.1016/S0140-6736(14)60584-5 -
6Rosamond WD, Gorton R, Hinn R, Hohenhaus SM, Morris DL. Rapid response to stroke symptoms: the Delay in Accessing Stroke Healthcare (DASH) study. Acad Emerg Med. 1998;5(1):45-51. doi:10.1111/j.1553-2712.1998.tb02574.x
» https://doi.org/10.1111/j.1553-2712.1998.tb02574.x -
7Feldmann E, Gordon N, Brooks JM, Brass LM, Fayad PB, Sawaya KL et al. Factors associated with early presentation of acute stroke. Stroke. 1993;24(12):1805-10. doi:10.1161/01.STR.24.12.1805
» https://doi.org/10.1161/01.STR.24.12.1805 -
8Williams LS, Bruno A, Rouch D, Marriott DJ, Mas DJ. Stroke patients’ knowledge of stroke : influence on time to presentation. Stroke. 1997;28(5):912-5. doi:10.1161/01.STR.28.5.912
» https://doi.org/10.1161/01.STR.28.5.912 -
9Wester P, Rådberg J, Lundgren B, Peltonen M. Factors associated with delayed admission to hospital and in-hospital delays in acute stroke and TIA: a prospective, multicenter study. Seek- Medical-Attention-in-Time Study Group. Stroke. 1999;30(1):40-8. doi:10.1161/01.STR.30.1.40
» https://doi.org/10.1161/01.STR.30.1.40 -
10Clark JM, Renier, Sa. A community stroke study: factors influencing stroke awareness and hospital arrival time. J Stroke Cerebrovasc Dis. 2001;10(6):274-8. doi:10.1053/jscd.2001.123774
» https://doi.org/10.1053/jscd.2001.123774 -
11Schroeder EB, Rosamond WD, Morris DL, Evenson KR, Hinn AR. Determinants of use of emergency medical services in a population with stroke symptoms : The Second Delay in Accessing Stroke Healthcare (DASH II) Study. Stroke. 2000;31(11):2591-6. doi:10.1161/01.STR.31.11.2591
» https://doi.org/10.1161/01.STR.31.11.2591 -
12Pontes-Neto OM, Silva GS, Feitosa MR, Figueiredo NL, Fiorot Jr JA, Rocha TN et al. Stroke awareness in Brazil: alarming results in a community-based study. Stroke. 2008;39(2):292-6. doi:10.1161/STROKEAHA.107.493908
» https://doi.org/10.1161/STROKEAHA.107.493908 -
13Nóvak EM, Zétola VHF, Muzzio JA, Puppi M, Carraro Júnior H, Werneck LC. [Lay knowledge about stroke]. Arq Neuropsiquiatr. 2003;61(3B):772-6. Portuguese. doi:10.1590/S0004-282X2003000500013
» https://doi.org/10.1590/S0004-282X2003000500013 -
14Hawkes MA, Ameriso SF, Willey JZ. Stroke knowledge in Spanish-speaking populations. Neuroepidemiology. 2015;44(3):121-9. doi:10.1159/000381100
» https://doi.org/10.1159/000381100 -
15Sprigg N, Machili C, Otter ME, Wilson A, Robinson TG. A systematic review of delays in seeking medical attention after transient ischaemic attack. J Neurol Neurosurg Psychiatry. 2009;80(8):871-5. doi:10.1136/jnnp.2008.167924
» https://doi.org/10.1136/jnnp.2008.167924 -
16Programa de las Naciones Unidas para el Desarrollo – PNUD. El sistema de salud argentino y su trayectoria de largo plazo: logros alcanzados y desafíos futuros. Buenos Aires: Programa de las Naciones Unidas para el Desarrollo ; 2011. (Aportes para el desarrollo humano en Argentina 2011, vol 6).
-
17Alberts MJ, Latchaw RE, Jagoda A, Wechsler LR, Crocco T, George MG et al. Revised and updated recommendations for the establishment of primary stroke centers: a summary statement from the brain attack coalition. Stroke. 2011;42(9):2651-65. doi:10.1161/STROKEAHA.111.615336
» https://doi.org/10.1161/STROKEAHA.111.615336 -
18Atallah AM, Fustinoni O, Zurru M, Beigelman R, Cirio J, Ameriso S et al. Identifying barriers in acute stroke therapy in Argentina. ARENAS Registry. Neurology. 2014;82(10 Suppl):P2.014.
-
19Sposato LA, Esnaola MM, Zamora R, Zurrú MC, Fustinoni O, Saposnik G. Quality of ischemic stroke care in emerging countries: the Argentinian National Stroke Registry (ReNACer). Stroke. 2008;39(11):3036-41. doi:10.1161/STROKEAHA.108.521062
» https://doi.org/10.1161/STROKEAHA.108.521062 -
20Díez-Ascaso O, Martinez-Sánchez P, Fuentes B, Díez-Tejedor E. Sociocultural study on the self-perception of stroke and an analysis of doctor-patient communication. Neurologia. 2011;26(2):81-91. doi:10.1016/j.nrl.2010.09.017
» https://doi.org/10.1016/j.nrl.2010.09.017 -
21Palomeras Soler E, Fossas Felip P, Quintana Luque M, Monteis Cahis R, Sebastián Salvatierra M, Fábregas Casarramona C et al. [Knowledge about stroke symptoms and attitude towards them in the population]. Neurologia. 2007;22(7):434-40. Spanish.
-
22Geffner D, Soriano C, Pérez T, Vilar C, Rodríguez D. Delay in seeking treatment by patients with stroke: who decides, where they go, and how long it takes. Clin Neurol Neurosurg. 2012;114(1):21-5. doi:10.1016/j.clineuro.2011.08.014
» https://doi.org/10.1016/j.clineuro.2011.08.014 -
23Harbison J, Hossain O, Jenkinson D, Davis J, Louw SJ, Ford GA. Diagnostic accuracy of stroke referrals from primary care, emergency room physicians, and ambulance staff using the face arm speech test. Stroke. 2002;34(1):71-6. doi:10.1161/01.STR.0000044170.46643.5E
» https://doi.org/10.1161/01.STR.0000044170.46643.5E -
24Moulin T, Sablot D, Vidry E, Belahsen F, Berger E, Lemounaud P et al. Impact of emergency room neurologists on patient management and outcome. Eur Neurol. 2003;50(4):207-14. doi:10.1159/000073861
» https://doi.org/10.1159/000073861
Publication Dates
-
Publication in this collection
Nov 2016
History
-
Received
15 Mar 2016 -
Received
05 June 2016 -
Accepted
12 July 2016