Abstracts
Objective:
to present the development of a toolkit for education quality improvement in universal health and primary health care, targeting schools of nursing and midwifery in Latin American and Caribbean countries.
Methods:
an expert work group conducted a systematic literature review, selected key content and completed toolkit drafting, using an iterative consensus approach. International partners reviewed the toolkit. Cognitive debriefing data were analyzed, revisions and new tools were integrated, and the final version was approved.
Results:
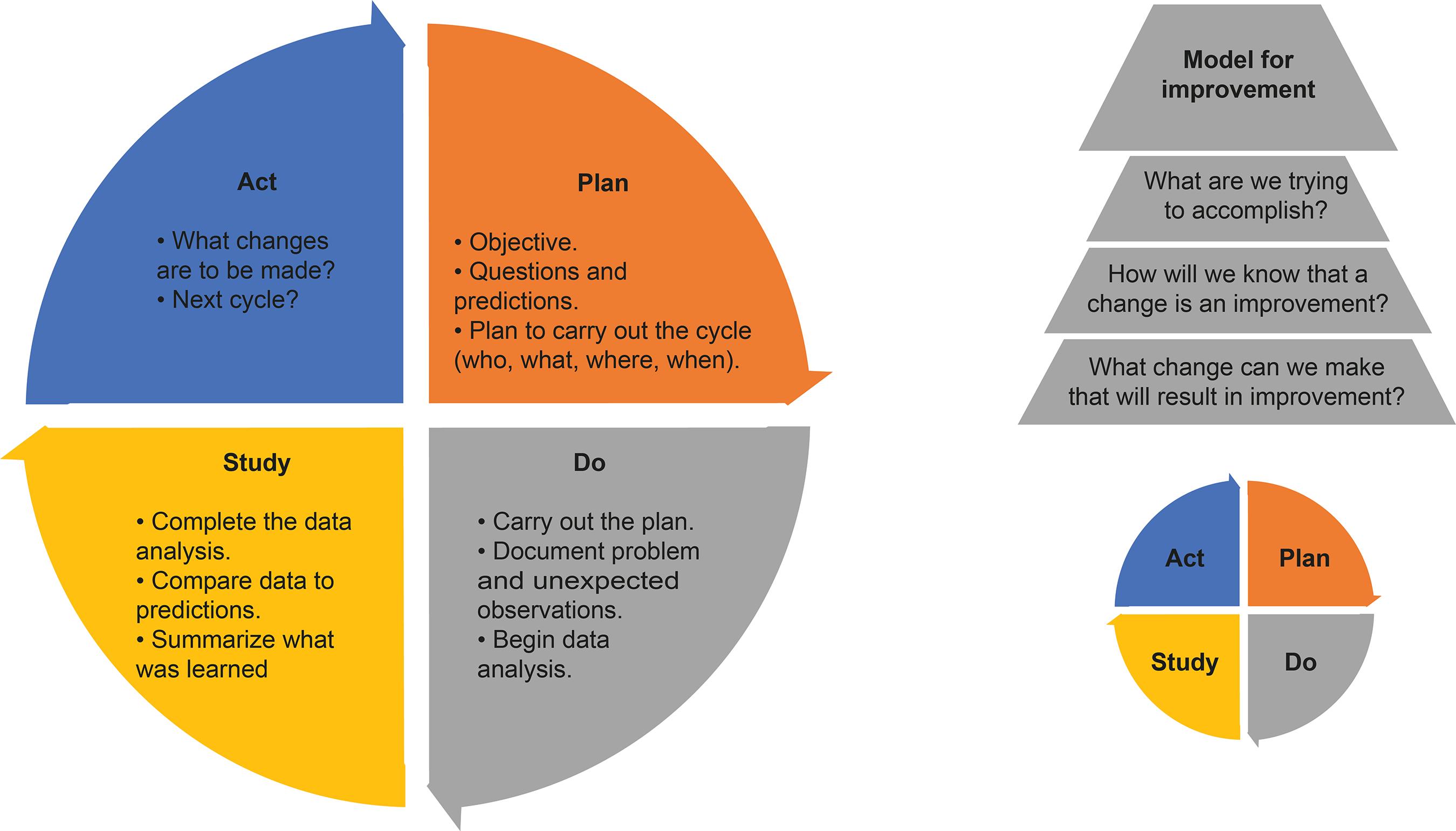
twenty-two articles were identified and mapped as resources. The Model for Improvement, a data-driven approach to performance analysis, was selected for its widespread use and simplicity in carrying out the following steps: 1) organize a team, 2) assess improvement need regarding universal health and primary health care education, 3) set an aim/goal and identify priorities using a matrix, 4) establish metrics, 5) identify change, 6) carry out a series of Plan-Do-Study-Act learning cycles, and 7) sustain change.
Conclusions:
the Education Quality Improvement Toolkit, developed through stakeholder consensus, provides a systematic, and potentially culturally adaptable approach to improve student, faculty, and program areas associated with universal health coverage and access.
Descriptors:
Primary Health Care; Quality Improvement; Universal Health Insurance; Nursing Education; Nurse Midwives; Midwifery
Objetivo:
apresentar o desenvolvimento de um kit de ferramentas para melhoria da qualidade da educação em saúde universal e na atenção primária à saúde em escolas de enfermagem e obstetrícia na América Latina e no Caribe.
Métodos:
um grupo de especialistas realizou uma revisão sistemática da literatura, selecionou conteúdos-chave e desenvolveu uma versão preliminar do kit, através de uma abordagem iterativa de consenso. Posteriormente, esta versão foi submetida a revisão por parceiros internacionais. Foram efetuadas análise dos dados obtidos em entrevista cognitiva, seguida da integração de revisões e de novas ferramentas até a se alcançar a aprovação da versão final.
Resultados:
vinte e dois estudos foram identificados e mapeados como recursos. O Modelo de Melhoria - uma abordagem baseada em dados para a análise de desempenho - foi selecionado devido a sua ampla difusão e simplicidade na execução das seguintes fases: 1) formação de uma equipe, 2) avaliação das melhorias necessárias na educação em saúde universal e atenção primária à saúde, 3) determinação de objetivos/metas e definição de prioridades com base numa matriz, 4) estabelecimento de métricas, 5) identificação de mudanças, 6) realização de uma série de ciclos de aprendizagem Planeje-Faça-Estude-Atue, e 7) manutenção das mudanças.
Conclusões:
o Kit de Ferramentas para Melhoria da Qualidade da Educação, desenvolvido a partir do consenso entre as partes envolvidas, representa uma abordagem sistemática, potencialmente adaptável às diversas culturas, para aprimorar aspectos do corpo discente, do corpo docente e de programas de educação relacionados com a cobertura e o acesso à saúde universal.
Descritores:
Atenção Primária à Saúde; Melhoria de Qualidade; Cobertura Universal do Seguro de Saúde; Educação em Enfermagem; Enfermeiras Obstétricas; Tocologia
Objetivo:
presentar el desarrollo de un kit de herramientas para la mejora de la calidad de la educación en salud universal y atención primaria de salud, dirigido a las escuelas de enfermería y obstetricia en los países de América Latina y el Caribe.
Métodos:
un grupo de trabajo de expertos realizó una revisión sistemática de la literatura, seleccionó el contenido clave y redactó las herramientas, utilizando un consenso iterativo. Socios internacionales revisaron el kit de herramientas. Se analizaron los datos de la entrevista cognitiva, se integraron las revisiones y las nuevas herramientas, y se aprobó la versión final.
Resultados:
veintidós artículos fueron identificados y registrados como recursos. Se seleccionó el Modelo para Mejoramiento, un enfoque basado en datos para el análisis del desempeño, por su uso generalizado y sencillez para realizar los siguientes pasos: 1) organizar un equipo, 2) evaluar la necesidad de mejora con respecto a la educación universal en salud y atención primaria de salud, 3) establecer el objetivo e identificar las prioridades utilizando una matriz, 4) establecer métricas, 5) identificar el cambio, 6) llevar a cabo una serie de ciclos de aprendizaje Planear-Hacer-Estudiar-Actuar, y 7) mantener el cambio.
Conclusiones:
el Kit de Herramientas para la Mejora de la Calidad de la Educación, desarrollado mediante el consenso de las partes interesadas, proporciona un enfoque sistemático y culturalmente adaptable en potencia para mejorar las áreas de los estudiantes, profesores y programas que se encuentran asociados con el acceso y cobertura universal de salud.
Descriptores:
Atención Primaria de Salud; Mejoramiento de la Calidad; Cobertura Universal del Seguro de Salud; Educación en Enfermería; Enfermeras Matronas; Partería
Introduction
In 2016, the Pan American Health Organization (PAHO), in collaboration with three World Health Organization Collaborating Centers (WHOCCs) in Nursing and Midwifery, and the Latin American Association of Nursing Schools and Faculty (ALADEFE), conducted an “Analysis of Nursing Education in the Region of the Americas towards Primary Health Care and Universal Health.” Latin American and Caribbean (LAC) nursing and midwifery programs were surveyed regarding their preparation of graduates to promote Universal Health (UH), their orientation towards Primary Health Care (PHC), and focus on social determinants of health. Although various program strengths were identified, this collaborative work identified a need for ongoing monitoring, evaluation, reporting and development of quality improvement (QI) plans, to ensure graduate preparedness in PHC and UH. Recommendations included: 1) strengthening knowledge of integrating information technologies (IT) into healthcare, environmental and global health, emergency and disaster preparedness, complex and systemic thinking, problem solving and evidence-based care; 2) expanding use of clinical simulation and training experiences in PHC settings; and 3) adopting the principles of interprofessional education (IPE) using practical team-based experiences that reflect country specific healthcare contexts and priorities around PHC and UH(11 Cassiani SHDB, Wilson LL, Mikael SSE, Morán-Peña L, Zarate-Grajales R, McCreary LL, et al. The situation of nursing education in Latin America and the Caribbean towards universal health. Rev. Latino-Am. Enfermagem. 2017;25:e2913. doi: 10.1590/1518-8345.2232.2913
https://doi.org/10.1590/1518-8345.2232.2...
).
In the footsteps of this study, the PAHO/WHOCC in International Nursing at the University of Alabama at Birmingham (UAB) was tasked to develop “Universal Health and Primary Health Care: a Plan for Nursing and Midwifery Education Quality Improvement.” This plan included an education quality improvement (EQI) Toolkit to assist nursing and midwifery programs in evaluating and improving structure, process, and outcomes within the framework of transformative education and competency-based interprofessional collaborative practice (IPCP). The overarching goal for this international multi-centric partnership study was to improve UH and PHC in LAC countries. In this paper, we will describe the development, evaluation by partners, and revision of the EQI Toolkit aimed to guide QI activities in nursing and midwifery education.
Transformative Education
In the era of a global economy, sweeping technological advances, growing disparities and increased focus on sustainability, higher education for health professionals is rapidly evolving. Pathways for transforming higher education to strengthen health systems in an interdependent and interprofessional world have been the focus of two simultaneous landmark reports(22 Frenk J, Chen L, Bhutta AZ, Cohen J, Crisp N, Evans T, et al. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet. 2010 [cited Dec 17, 2016];376(9756):1923-58. doi: 10.1016/S0140-6736(10)61854-5
https://doi.org/10.1016/S0140-6736(10)61...
-33 World Health Organization. Framework for action on interprofessional education & collaborative practice. [WHO/HRH/HPN/10.3]. [Internet]. Geneva; 2010 [cited Dec 14, 2016]. Available from: http://whqlibdoc.who.int/hq/2010/WHO_HRH_HPN_10.3_eng.pdf
http://whqlibdoc.who.int/hq/2010/WHO_HRH...
). Transformative education encompasses principles of critical thinking, team work, creative adaptation, integration of education into health systems, resource sharing, networking and partnerships(22 Frenk J, Chen L, Bhutta AZ, Cohen J, Crisp N, Evans T, et al. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet. 2010 [cited Dec 17, 2016];376(9756):1923-58. doi: 10.1016/S0140-6736(10)61854-5
https://doi.org/10.1016/S0140-6736(10)61...
-33 World Health Organization. Framework for action on interprofessional education & collaborative practice. [WHO/HRH/HPN/10.3]. [Internet]. Geneva; 2010 [cited Dec 14, 2016]. Available from: http://whqlibdoc.who.int/hq/2010/WHO_HRH_HPN_10.3_eng.pdf
http://whqlibdoc.who.int/hq/2010/WHO_HRH...
). Interprofessional education, where students learn from each other outside traditional disciplinary silos, is a pre-requisite to transformative education(33 World Health Organization. Framework for action on interprofessional education & collaborative practice. [WHO/HRH/HPN/10.3]. [Internet]. Geneva; 2010 [cited Dec 14, 2016]. Available from: http://whqlibdoc.who.int/hq/2010/WHO_HRH_HPN_10.3_eng.pdf
http://whqlibdoc.who.int/hq/2010/WHO_HRH...
). Preparing the future healthcare workforce for IPCP, different disciplines working effectively together in teams with patients, families, caregivers, and communities, is a prerequisite to delivering the highest quality care(33 World Health Organization. Framework for action on interprofessional education & collaborative practice. [WHO/HRH/HPN/10.3]. [Internet]. Geneva; 2010 [cited Dec 14, 2016]. Available from: http://whqlibdoc.who.int/hq/2010/WHO_HRH_HPN_10.3_eng.pdf
http://whqlibdoc.who.int/hq/2010/WHO_HRH...
). The High-Level Commission on Health Employment and Economic Growth, established by the United Nations (UN), WHO, and other agencies, recommends scaling up transformative and lifelong learning for the healthcare workforce(44 World Health Organization, High-Level Commission on Health Employment and Economic Growth. Working for health and growth: Investing in the health workforce. Geneva: World Health Organization. [Internet]. 2016 [cited Jan 22, 2017]. Available from: http://www.who.int/hrh/com-heeg/reports/en/
http://www.who.int/hrh/com-heeg/reports/...
). To move forward the UN 2030 Sustainable Development Goals (SDGs) agenda, nurses and midwives must be prepared to practice and thrive in an ever-changing environment, assessing evidence and working collaboratively with other healthcare professionals to meet the needs of diverse populations.
Universal health (UH) access and coverage are two of the main indicators for ensuring healthy lives and promoting well-being for all (SDG #3). Defined as “the absence of geographical, economic, sociocultural, organizational, or gender barriers” universal access to health is achieved through “the progressive elimination of barriers that prevent all people from having equitable use of comprehensive health services determined at the national level”(55 Pan American Health Organization. Strategy for universal access to health and universal health coverage. [CD53.R14]. Washington, D.C.: PAHO. [Internet]. 2014 [cited Feb 11, 2017]. Available from: http://www.paho.org/uhexchange/index.php/en/uhexchange-documents/technical-information/26-strategy-for-universal-access-to-health-and-universal-health-coverage/file
http://www.paho.org/uhexchange/index.php...
). Universal health coverage (UHC) is a financial protection arrangement for health for all. It is often achieved through some form of national health insurance program to serve the needs of the population(66 World Health Organization. The world health report 2008: Primary health care (now more than ever). Geneva: World Health Organization. [Internet]. 2008 [cited Jun 30, 2018]. Available from: https://www.who.int/whr/2008/en/
https://www.who.int/whr/2008/en/...
). Closely tied to both concepts, PHC aims to achieve better health for all through reform in universal coverage, service delivery, public policy, and leadership(77 World Health Organization. Operations manual for staff at primary health care centres. Geneva: World Health Organization. [Internet]. 2008 [cited May 17, 2018]; p. 282. Available from: http://www.who.int/hiv/pub/imai/om.pdf
http://www.who.int/hiv/pub/imai/om.pdf...
). Organizing health services around peoples’ needs and expectations, and increasing stakeholder participation are two key PHC mandates. Recently, the potential contribution of nurses and midwives towards achieving UH has been a focus of the Nursing Now Campaign(88 Nursing Now Campaign. [Internet]. 2018 [cited May 1, 2018]. Available from: http://www.nursingnow.org/our-aims/; http://www.nursingnow.org/programmes/
http://www.nursingnow.org/our-aims/...
). Based on the premise that investment in nursing will enable nurses to achieve their full potential, nursing and midwifery education programs are urged to prepare graduates in promoting UH and PHC.
In order to prepare competent and skillful entry-level nurses and midwives in providing PHC and UH, educators must meet a minimum of core competencies. The “Midwifery Educator Core Competencies”
(99 World Health Organization. Midwifery Educator Core Competencies. Geneva: World Health Organization. [Internet]. 2014 [cited June 30, 2018]. Available from: https://www.who.int/hrh/nursing_midwifery/educator_competencies/en/
https://www.who.int/hrh/nursing_midwifer...
) and the “Nurse Educator Core Competencies”
(1010 World Health Organization. Nurse Educator Competencies. Geneva: WHO. [Internet]. 2016 [cited Aug 1, 2018]. Available from: http://www.who.int/hrh/nursing_midwifery/nurse_educator050416.pdf
http://www.who.int/hrh/nursing_midwifery...
) were developed in response to the World Health Assembly resolutions upon consultation with key partners. Both documents aim to support and guide educational institutions, worldwide, in modifying their competencies-based curricula within each country’s parameters, including diversity and availability of resources. Monitoring, assessment and evaluation of students and programs are listed as educator competencies for both nurses and midwives(99 World Health Organization. Midwifery Educator Core Competencies. Geneva: World Health Organization. [Internet]. 2014 [cited June 30, 2018]. Available from: https://www.who.int/hrh/nursing_midwifery/educator_competencies/en/
https://www.who.int/hrh/nursing_midwifer...
-1010 World Health Organization. Nurse Educator Competencies. Geneva: WHO. [Internet]. 2016 [cited Aug 1, 2018]. Available from: http://www.who.int/hrh/nursing_midwifery/nurse_educator050416.pdf
http://www.who.int/hrh/nursing_midwifery...
) linking core competencies to the ongoing debate about improving educational outcomes in nursing and midwifery schools.
Background - Nursing and Midwifery Education in Latin America and the Caribbean
Entry-level nursing and midwifery education in LAC countries reflects regional disparities in terms of geography, politics, economy, and culture(1111 World Health Organization. Global Standards for the initial education of professional nurses and midwives [WHO/HRH/HPN/08.6]. Geneva: WHO. [Internet]. 2009 [cited Dec 18, 2016]. Available from: http://www.who.int/hrh/nursing_midwifery/hrh_global_standards_education.pdf
http://www.who.int/hrh/nursing_midwifery...
). Variation in levels of educational preparation affect workforce capacity, in both numbers and skill mix, which ultimately influences care quality. For example, some Eastern Caribbean countries have more than 40 professional nurses per 10,000 population, whereas most of the Spanish-speaking countries in the region have less than 10 per 10,000(1212 Carpio C, Bench NS. The Health Workforce in Latin America and the Caribbean: An analysis of Colombia, Costa Rica, Jamaica, Panama, Peru and Uruguay. World Bank Group. [Internet]. 2015 [cited Jun 30, 2018]. Available from: http://dx.doi.org/10.1596/978-1-4648-0594-3
http://dx.doi.org/10.1596/978-1-4648-059...
).
Similarly, teaching and practicing midwifery varies greatly, with an ongoing debate over education and care models(1313 Luyben A, Barger M, Avery M, Bharj KK, O’connel R, Fleming V, et al. Exploring global recognition of quality midwifery education: Vision or fiction? Women and Birth. 2017 Jun; 30(3):184-92. doi: 10.1016/j.wombi.2017.03.001
https://doi.org/10.1016/j.wombi.2017.03....
). Midwifery can be practiced by obstetric nurses, nurse-midwives, professional midwives, and in some countries, by traditional midwives, with education ranging from lay midwifery to undergraduate and/or post-graduate preparation(1414 Pan American Health Organization. Toolkit for strengthening professional midwifery in the Americas. Washington, D.C.: PAHO. [Internet]. 2014 [cited Sep 7, 2018]. Available from: https://www.paho.org/clap/index.php?option=com_docman&view=download&category_slug=salud-de-mujer-reproductiva-materna-y-perinatal&alias=427-toolkit-for-strengthening-professional-midwifery-in-the-americas-3-ed-1&Itemid=219&lang=es
https://www.paho.org/clap/index.php?opti...
). For countries with low numbers of skilled birth attendants and high maternal mortality rates, it has been recommended that Ministries of Health consider professional midwifery as a key to improving maternal and perinatal health(1414 Pan American Health Organization. Toolkit for strengthening professional midwifery in the Americas. Washington, D.C.: PAHO. [Internet]. 2014 [cited Sep 7, 2018]. Available from: https://www.paho.org/clap/index.php?option=com_docman&view=download&category_slug=salud-de-mujer-reproductiva-materna-y-perinatal&alias=427-toolkit-for-strengthening-professional-midwifery-in-the-americas-3-ed-1&Itemid=219&lang=es
https://www.paho.org/clap/index.php?opti...
). Therefore, strategies to strengthen the quality of nursing and midwifery education are vital for establishing a competent workforce and must be set in the context of each country.
Quality Improvement in Healthcare and Health Professional Education
Quality improvement, as we currently know it in healthcare and education, originated in 1939 with control charts to track variation in manufacturing defects and the “learning and improvement cycle” known in healthcare as the Plan-Do-Study-Act (PDSA) cycle(1515 Shewhart WA. Statistical Method from the Viewpoint of Quality Control. Department of Agriculture. [Internet]. 1986 [cited June 30, 2018]; p. 45. Available from: https://archive.org/details/CAT10502416
https://archive.org/details/CAT10502416...
). Studying what is occurring and its variation patterns was viewed as a first step before intervening to improve quality. The impact of specific QI approaches varies, depending on the context in which they are implemented(1616 Devers KJ. The state of quality improvement science in health: What do we know about how to provide better care? Robert Wood Johnson Foundation & Urban Institute. [Internet]. 2011 Nov [cited June 30, 2018]. Available from: https://www.rwjf.org/en/library/research/2011/11/the-state-of-quality-improvement-science-in-health.html
https://www.rwjf.org/en/library/research...
). In general, success of a QI program is determined by an organization’s commitment to monitor, assess, improve, and embed continuous improvement into the organization’s culture for seeking higher levels of performance. Understanding systems and how they interact is critical, since improvement in one area of operations may induce unintended consequences, and even harm, in another area(1717 U. S. Department of Health and Human Services - Health Resources and Services Administration. Quality Improvement. Washington, D.C. [Internet]. 2011 [cited Aug 1, 2018]. Available from: https://www.hrsa.gov/sites/default/files/quality/toolbox/508pdfs/qualityimprovement.pdf
https://www.hrsa.gov/sites/default/files...
). Focusing improvement efforts on customers who benefit from the system is fundamental, whether they be patients, students, providers, or teachers. A team approach, involving more than one discipline, builds creativity, enthusiasm, and commitment to the work. Focus on collecting and using data, constant monitoring, and tracking the same elements throughout the iterative PDSA cycles is paramount to successful QI endeavors. The WHO has defined QI as “An approach to improvement of service systems and processes through the routine use of health and programme data to meet patient and programme needs.”(77 World Health Organization. Operations manual for staff at primary health care centres. Geneva: World Health Organization. [Internet]. 2008 [cited May 17, 2018]; p. 282. Available from: http://www.who.int/hiv/pub/imai/om.pdf
http://www.who.int/hiv/pub/imai/om.pdf...
) This versatile definition can be applied to both healthcare delivery and educational programs. Improving quality in healthcare requires an appreciation and understanding of system complexity, critical components, and most importantly, the cultural context and population served(1818 Institute of Medicine. Crossing the quality chasm: A new health system for the 21st Century Committee on Quality of Health Care in America, ed. N.A. Press; Washington, DC. IOM. [Internet]. 2001 [cited Aug 1, 2018]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25057539
https://www.ncbi.nlm.nih.gov/pubmed/2505...
). Educational program quality can be defined as the degree to which didactic and clinical education increases the likelihood of desirable outcomes, consistent with current knowledge. These educational outcomes should reflect competencies of nurses and midwives as they relate to providing patient care.
In light of the above priorities and needs for highly competent nursing and midwifery professionals who are well-equipped to promote UH and PHC, this article aims to present the development of an EQI Toolkit for schools of nursing and midwifery in LAC countries.
Method
Following the Standards for Quality Improvement Reporting Excellence (SQUIRE), this multi-centric study is outlined in sequential phases (Figure 1).
Phase 1 - QI expert work group
A group of 10 faculty with expertise in the areas of QI, improvement science, program evaluation, competency-based education, IPE, IPCP, midwifery, primary health care, rural care, and global health were assembled. This expert group was tasked with reviewing previous work on educational resources in the LAC region, as well as the broader literature, to develop a plan for self-directed QI among nursing and midwifery schools/programs. As a starting point, an extensive survey carried out across LAC nursing school programs regarding preparation of graduates to promote UH and PHC was reviewed for baseline data and recommendations(11 Cassiani SHDB, Wilson LL, Mikael SSE, Morán-Peña L, Zarate-Grajales R, McCreary LL, et al. The situation of nursing education in Latin America and the Caribbean towards universal health. Rev. Latino-Am. Enfermagem. 2017;25:e2913. doi: 10.1590/1518-8345.2232.2913
https://doi.org/10.1590/1518-8345.2232.2...
). For consistency with this previous PAHO commissioned work, the term UH was used as encompassing both universal access to health and universal health coverage. Donabedian’s model(1919 Donabedian A. Evaluating the quality of medical care. Milbank Mem Fund Q. 1966;44 (Suppl):166-206. doi: 10.2307/3348969
https://doi.org/10.2307/3348969...
) provided the framework for toolkit design and was operationalized through the QI process; a data-driven, formal approach to performance analysis in nursing and midwifery educational programs and the systematic efforts to improve it(1616 Devers KJ. The state of quality improvement science in health: What do we know about how to provide better care? Robert Wood Johnson Foundation & Urban Institute. [Internet]. 2011 Nov [cited June 30, 2018]. Available from: https://www.rwjf.org/en/library/research/2011/11/the-state-of-quality-improvement-science-in-health.html
https://www.rwjf.org/en/library/research...
).
Phase 2 - Literature review
A systematic literature search on the topic of QI, as it relates to nursing and midwifery education or nursing and midwifery education programs, was carried out in five databases; PubMed, Scopus, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), the Latin American & Caribbean Health Sciences Literature (LILACS), and Google/PAHO. Search terms included: “education, nursing, midwifery, baccalaureate, program accreditation, quality improvement, standards, Latin America, Caribbean”. A total of 313 peer-reviewed full-text articles, published within the last 10 years (from 2010 to 2018) in English language were retrieved. Search strategy results are presented in the PRISMA flow chart (Figure 2).
Two investigators from the phase 1 expert group conducted independent title/abstract/full text reviews, discussed disagreements and a consensus was met. A total of 50 articles were screened for the following inclusion criteria: 1) focus on an educational program or school of nursing or midwifery; 2) focus on monitoring or evaluation or assessment of quality or implementation of a QI project; and 3) focus on a model or conceptual framework in relation to accreditation, competency-based education, IPE, IPCP or transformational education. Exclusion criteria were: 1) focus on a healthcare setting; 2) clinical practice focus; and 3) no full-text available online.
Phase 3 - EQI Toolkit development
With surveyed areas for improvement in mind, the same 10-member expert group: 1) identified existing QI resources for nursing and midwifery educational programs, and 2) prepared the model for a QI plan that could be tailored by LAC schools to address specific weaknesses in UH and PHC. Development of this model evolved into the EQI Toolkit with a target population of all nursing and midwifery schools offering undergraduate programs in the LAC region. Because of substantial educational differences among programs, it was clear that the toolkit would need to be adaptable to country/language/culture/setting, plus be user friendly and simple to use. For clarity, a glossary of terms with appropriate references was developed as an appendix to the EQI Toolkit.
The first toolkit version was developed using brainstorming and modified affinity grouping techniques. This process allowed the expert work group to generate, categorize, and choose among ideas by posting common themes on a flip chart(2020 Dartmouth College - Sheffield Microsystem Coaching Academy. Brainstorming, Affinity Grouping and Multivoting ‘A one page book’. [Internet]. 2014 [cited Aug 1, 2018]. Available from: http://www.sheffieldmca.org.uk/UserFiles/File/Brainstorming_one_page_book_V2.pdf
http://www.sheffieldmca.org.uk/UserFiles...
). For this project, ideas were recorded using a laptop and were immediately projected onto a screen for everyone to see and compare notes. Each work group member took responsibility for drafting content and tools for inclusion. An iterative process was used to select and connect the key elements to form a coherent resource for the next phase of review.
Phase 4 - EQI Toolkit user evaluation and revision
To obtain user evaluation, the qualitative method of iterative processing cognitive debriefing was applied. Four international stakeholders were invited as reviewers through three partnering PAHO/WHOCCs. Individuals represented Brazil, Chile, and Mexico and were chosen for their diverse perspectives and technical expertise. They were asked to review the first version and to provide detailed comments, suggestions, and track-changes in the actual file. Further, reviewers were asked to complete the Cognitive Debriefing Form (Figure 3) during a live virtual meeting.
Two investigators asked questions and recorded responses. For two of the Spanish speaking respondents, questions and answers were translated back and forth by the Spanish speaking investigator. Respondent behaviors, such as asking for clarifications, being ambivalent or skipping items were recorded. Any difficulties experienced by subjects were used to modify the first toolkit version, thus making data collection an iterative process. Qualitative content analysis of cognitive debriefing data from the international reviewers was applied. In addition, the reviewers’ electronic track changes and added comments were also considered as part of the review process. Last, reaching consensus was used when reconciling reviewers’ input and data in order to agree on a final version of the EQI Toolkit.
Ethics
The UAB Institutional Review Board (IRB) designated this project as Not Human Subjects Research (IRB-300002006). The international review process was overseen by the leading investigator who safeguarded ethical standards of conduct and that all review comments were carefully considered.
Results
Literature review
A total of 22 articles met all inclusion criteria and are listed in Figure 4 as existing resources for this project, along with key relevant points. Type of study and level of evidence was appraised based on the hierarchical classification by Melnyk and Fineout-Overholt(2121 Melnyk BM, Fineout-Overhold E. Evidence-based practice in nursing and healthcare: a guide to best practice. 2ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams and Wilkins; 2011.).
Literature review articles according to type of study, level of evidence, implications and resource theme
Content analysis of selected articles revealed the following themes: 1) assessment - evaluation; 2) continuous quality improvement (CQI) - accreditation; 3) curriculum plan development; and 4) implementation - case study. Key points relevant to QI efforts in schools of nursing and midwifery, with a focus on UH and PHC, are presented below, grouped according to above themes.
Assessment and evaluation are essential to the QI process, reflected in select articles(11 Cassiani SHDB, Wilson LL, Mikael SSE, Morán-Peña L, Zarate-Grajales R, McCreary LL, et al. The situation of nursing education in Latin America and the Caribbean towards universal health. Rev. Latino-Am. Enfermagem. 2017;25:e2913. doi: 10.1590/1518-8345.2232.2913
https://doi.org/10.1590/1518-8345.2232.2...
,2727 Escallier LA, Fullerton JT. An innovation in design of a school of nursing evaluation protocol. Nurse Educator. 2012;37(5):187-91. doi: 10.1097/NNE.0b013e318262eb15
https://doi.org/10.1097/NNE.0b013e318262...
28 Fater KH. Gap analysis: A method to assess core competency development in the curriculum. Nurs Educn Perspect. 2013; 34(2):101-5. doi: 10.5480/1536-5026-34.2.101
https://doi.org/10.5480/1536-5026-34.2.1...
-2929 González-Chordá VM, Maciá-Soler ML. Evaluation of the quality of the teaching-learning process in undergraduate courses in Nursing. Rev. Latino-Am. Enfermagem. 2015; 23(4):700-7. doi: 10.1590/0104-1169.0393.2606
https://doi.org/10.1590/0104-1169.0393.2...
). Despite the labor intensive nature of data mining, it is argued that gap analysis and feedback, as a method to assess core competency in the curriculum, could decrease content saturation and promote active learning(2828 Fater KH. Gap analysis: A method to assess core competency development in the curriculum. Nurs Educn Perspect. 2013; 34(2):101-5. doi: 10.5480/1536-5026-34.2.101
https://doi.org/10.5480/1536-5026-34.2.1...
). Program evaluation is achieved through course reviews, student surveys, pre-and-post-program assessment of students’ knowledge/skills, and faculty interviews about their experiences with new teaching methods(2727 Escallier LA, Fullerton JT. An innovation in design of a school of nursing evaluation protocol. Nurse Educator. 2012;37(5):187-91. doi: 10.1097/NNE.0b013e318262eb15
https://doi.org/10.1097/NNE.0b013e318262...
,2929 González-Chordá VM, Maciá-Soler ML. Evaluation of the quality of the teaching-learning process in undergraduate courses in Nursing. Rev. Latino-Am. Enfermagem. 2015; 23(4):700-7. doi: 10.1590/0104-1169.0393.2606
https://doi.org/10.1590/0104-1169.0393.2...
). It is recommended that evaluation protocols include linkages to external criteria for evaluating the plan itself, while the teaching-learning process should be subject to ongoing QI(2727 Escallier LA, Fullerton JT. An innovation in design of a school of nursing evaluation protocol. Nurse Educator. 2012;37(5):187-91. doi: 10.1097/NNE.0b013e318262eb15
https://doi.org/10.1097/NNE.0b013e318262...
). This is consistent with findings from an extensive survey of nursing schools in LAC countries showing nursing program evaluation, student evaluation, and outcomes as the top priorities for QI initiatives(11 Cassiani SHDB, Wilson LL, Mikael SSE, Morán-Peña L, Zarate-Grajales R, McCreary LL, et al. The situation of nursing education in Latin America and the Caribbean towards universal health. Rev. Latino-Am. Enfermagem. 2017;25:e2913. doi: 10.1590/1518-8345.2232.2913
https://doi.org/10.1590/1518-8345.2232.2...
). Using an original self-assessment tool, the same survey revealed the heterogeneity of education, with a clear need to strengthen training in UH, PHC, and transformational education. Schools seeking accreditation are highly encouraged to develop periodic evaluations of curricula and programs with participation from their students, as well as to share the results with educational authorities and professional organizations(11 Cassiani SHDB, Wilson LL, Mikael SSE, Morán-Peña L, Zarate-Grajales R, McCreary LL, et al. The situation of nursing education in Latin America and the Caribbean towards universal health. Rev. Latino-Am. Enfermagem. 2017;25:e2913. doi: 10.1590/1518-8345.2232.2913
https://doi.org/10.1590/1518-8345.2232.2...
).
The CQI-accreditation approach is described in select articles(2424 Brown JF, Marshall BL. Continuous quality improvement: An effective strategy for improvement of program outcomes in a higher education setting. Nurs Educ Perspect. [Internet]. 2008 [cited June 30, 2018];29(4):205-11. Available from: https://www.ncbi.nlm.nih.gov/pubmed/18770948
https://www.ncbi.nlm.nih.gov/pubmed/1877...
,2626 Ellis P, Halstead J. Understanding the commission on collegiate nursing education accreditation process and the role of the continuous improvement progress report. J Prof Nurs. 2012; 28(1):18-26. doi: 10.1016/j.profnurs.2011.10.004
https://doi.org/10.1016/j.profnurs.2011....
,3030 Halstead JA. The value of nursing program accreditation. Teach Learn Nurs. [Internet]. 2017; 12(3):181-2. doi: 10.1016/j.teln.2017.03.005
https://doi.org/10.1016/j.teln.2017.03.0...
-3131 Hooper JI, Ayars VD. How Texas nursing education programs increased NCLEX pass rates and improved programming. J Nurs Regulation. [Internet]. 2017; 8(3):53-8. doi: 10.1016/S2155-8256(17)30160-6
https://doi.org/10.1016/S2155-8256(17)30...
,3636 Nugent E, LaRocco S. Comprehensive review of an accelerated nursing program: A quality improvement project. Dimens Crit Care Nurs. 2014; 33(4):226-33. doi: 10.1097/DCC.0000000000000054
https://doi.org/10.1097/DCC.000000000000...
,3838 Santos M. The role of nursing education in the transformation of the U.S. health system. Online Braz J Nurs. 2012; 11(2):257-60. doi: 10.5935/1676-4285.20120024
https://doi.org/10.5935/1676-4285.201200...
,4040 Sherrod RA, Morrison RS. Leadership experiences for baccalaureate nursing students: Improving quality in a nurse-managed rural health clinic. Nurs Educ Perspectives. [Internet]. 2008 [cited Sept 29, 2018];29(4):212-216. Available from: https://wwww.unboundmedicine.com/medline/citation/18770949/Leadership_experiences_for_baccalaureate_nursing_students:_improving_quality_in_a_nurse_managed_rural_health_clinic_
https://wwww.unboundmedicine.com/medline...
,4242 Wolf ZR, Czekanski KE. Analyzing student complaints against nursing programs: taxonomies of complaints and outcomes. J Prof Nurs. 2011 Sep-Oct; 27(5):283-91. doi: 10.1016/j.profnurs.2011.06.00443.
https://doi.org/10.1016/j.profnurs.2011....
). It provides metrics and information to administrators and faculty regarding the rigor of programs and the potential of graduates. CQI as a hallmark of the accreditation process, identifies areas for improvement and allows for planning(3030 Halstead JA. The value of nursing program accreditation. Teach Learn Nurs. [Internet]. 2017; 12(3):181-2. doi: 10.1016/j.teln.2017.03.005
https://doi.org/10.1016/j.teln.2017.03.0...
). Thus, the Standards for Accreditation of Baccalaureate and Graduate Degree Nursing Programs in USA, required by the Commission on Collegiate Nursing Education (CCNE), are also examined as an ongoing CQI process(2626 Ellis P, Halstead J. Understanding the commission on collegiate nursing education accreditation process and the role of the continuous improvement progress report. J Prof Nurs. 2012; 28(1):18-26. doi: 10.1016/j.profnurs.2011.10.004
https://doi.org/10.1016/j.profnurs.2011....
,4242 Wolf ZR, Czekanski KE. Analyzing student complaints against nursing programs: taxonomies of complaints and outcomes. J Prof Nurs. 2011 Sep-Oct; 27(5):283-91. doi: 10.1016/j.profnurs.2011.06.00443.
https://doi.org/10.1016/j.profnurs.2011....
). Brown and Marshall(2424 Brown JF, Marshall BL. Continuous quality improvement: An effective strategy for improvement of program outcomes in a higher education setting. Nurs Educ Perspect. [Internet]. 2008 [cited June 30, 2018];29(4):205-11. Available from: https://www.ncbi.nlm.nih.gov/pubmed/18770948
https://www.ncbi.nlm.nih.gov/pubmed/1877...
) use a quality enhancement plan (QEP) to assess key factors affecting program outcomes. They demonstrate CQI effectiveness in increasing NCLEX-RN pass rates, improving student advisement, and raising student satisfaction. Other effective interventions across programs include: early identification of students at risk, timely remediation, and program policy enforcement(3131 Hooper JI, Ayars VD. How Texas nursing education programs increased NCLEX pass rates and improved programming. J Nurs Regulation. [Internet]. 2017; 8(3):53-8. doi: 10.1016/S2155-8256(17)30160-6
https://doi.org/10.1016/S2155-8256(17)30...
). Of equal importance is surveying past graduates of their opinion and feedback about strengths and weaknesses of the school/program(3636 Nugent E, LaRocco S. Comprehensive review of an accelerated nursing program: A quality improvement project. Dimens Crit Care Nurs. 2014; 33(4):226-33. doi: 10.1097/DCC.0000000000000054
https://doi.org/10.1097/DCC.000000000000...
).
For curriculum plan development, faculty collaborations and partnerships were instrumental in augmenting evaluation tools and processes for clinical learning, expanding clinical capacity, and improving clinical experiences(2222 Andresen K, Levin P. Enhancing quantity and quality of clinical experiences in a baccalaureate nursing program. Int J Nurs Educ Scholarsh. 2014;11(1):1-8. doi: 10.1515/ijnes-2013-0053
https://doi.org/10.1515/ijnes-2013-0053...
). Armstrong et al.(2323 Armstrong GE, Spencer TS, Lenburg CB. Using quality and safety education for nurses to enhance competency outcome performance assessment: A synergistic approach that promotes patient safety and quality outcomes. J Nurs Educ. 2009;48(12):686-93. doi: 10.3928/01484834-20091113-02
https://doi.org/10.3928/01484834-2009111...
) use the Quality and Safety Education for Nurses (QSEN) competencies to enhance a competency outcome performance assessment (COPA)-based curriculum. Reflective components of practice-based learning activities based on QSEN competencies engage students in evaluating: 1) level of comfort with being a change agent, 2) unit climate for change, and 3) delegation and communication skills(3939 Seibert SA. Safety consciousness: Assignments that expand focus beyond the bedside. Nurse Educ Today. 2014;34(2):233-6. doi: 10.1016/j.nedt.2013.08.002
https://doi.org/10.1016/j.nedt.2013.08.0...
).
Implementation case studies have shown that students’ readiness to learn and ability to embrace concepts, processes, and outcomes measurement is enhanced by early teaching of systems and QI thinking within an undergraduate curriculum(3434 Karagory PM, McComb S. Measuring the vital signs of the health care system with the first clinical experience: Sophomore nursing students rise to the challenge. J Nurs Educ. 2014; 53:S97-S100. doi: 10.3928/01484834-20140806-01
https://doi.org/10.3928/01484834-2014080...
-3535 McComb SA, Kirkpatrick JM. Infusing systems and quality improvement throughout an undergraduate nursing curriculum. J Nurs Educ. 2017;56(12):752-7. doi: 10.3928/01484834-20171120-10
https://doi.org/10.3928/01484834-2017112...
). Exposing students to real world experiences that underline the significance of these skills helps bridge the education-practice gap(3535 McComb SA, Kirkpatrick JM. Infusing systems and quality improvement throughout an undergraduate nursing curriculum. J Nurs Educ. 2017;56(12):752-7. doi: 10.3928/01484834-20171120-10
https://doi.org/10.3928/01484834-2017112...
). A study with United Kingdom student nurses showed that they can successfully overcome their fears and meet the QI practicum challenge, if adequate support mechanisms are in place(3232 James B, Beattie M, Shepherd A, Armstrong L, Wilkinson J. Time, fear and transformation: Student nurses’ experiences of doing a practicum (quality improvement project) in practice. Nurse Educ Practice. 2016; 19:70-8. doi: 10.1016/j.nepr.2016.05.004
https://doi.org/10.1016/j.nepr.2016.05.0...
). Doing a practicum as a compulsory assignment in a large-scale cohort is achievable, if there is balance between motivation to learn and fear(3232 James B, Beattie M, Shepherd A, Armstrong L, Wilkinson J. Time, fear and transformation: Student nurses’ experiences of doing a practicum (quality improvement project) in practice. Nurse Educ Practice. 2016; 19:70-8. doi: 10.1016/j.nepr.2016.05.004
https://doi.org/10.1016/j.nepr.2016.05.0...
). Students develop teamwork and leadership skills, while clinical partners are motivated by the students(3434 Karagory PM, McComb S. Measuring the vital signs of the health care system with the first clinical experience: Sophomore nursing students rise to the challenge. J Nurs Educ. 2014; 53:S97-S100. doi: 10.3928/01484834-20140806-01
https://doi.org/10.3928/01484834-2014080...
). Adopting a blended learning approach, where face-to-face classroom and online teaching is combined with clinical experiences, along with incorporating IT through the use of electronic portfolios to demonstrate student accomplishments and document program and course outcomes, have shown promising results(3737 Posey L, Pintz C. Transitioning a bachelor of science in nursing program to blended learning: Successes, challenges & outcomes. Nurse Educ Practice. 2017; 26:126-33. doi: 10.1016/j.nepr.2016.10.006
https://doi.org/10.1016/j.nepr.2016.10.0...
,4141 Wassef ME, Riza L, Maciag T, Worden C, Delaney A. Implementing a competency-based electronic portfolio in a graduate nursing program. Comput Inform Nurs. 2012; 30(5):242-8. doi: 10.1097/NXN.0b013e31824af6d4.
https://doi.org/10.1097/NXN.0b013e31824a...
). Furthermore, use of patient simulators and the concierge model of simulation can be an effective strategy for deliberate practice of skills and standardized exposure to limited scenarios(2525 Coffman S, Doolen J, Llasus L. Program development and evaluation of the concierge model of simulation. Online J Nurs Informatics. [Internet]. 2015 [cited Aug 1, 2018];19(2):8-8. Available from: https://www.himss.org/program-development-and-evaluation-concierge-model-simulation
https://www.himss.org/program-developmen...
,3333 Kaplan BG, Holmes L, Mott M, Atallah H. Design and implementation of an interdisciplinary pediatric mock code for undergraduate and graduate nursing students. Comput Inform Nurs. [Internet]. 2011; 29(9):531-8. doi: 10.1097/NCN.0b013e31821a166e
https://doi.org/10.1097/NCN.0b013e31821a...
). Clinical simulation and debriefing are effective methods to incorporate the competencies as set forth by the Institute of Medicine (IOM) and the American Association of Colleges of Nursing (AACN); patient-centered care, interprofessional teams, evidence-based practice, clinical reasoning, patient safety, and practice across the life span(3333 Kaplan BG, Holmes L, Mott M, Atallah H. Design and implementation of an interdisciplinary pediatric mock code for undergraduate and graduate nursing students. Comput Inform Nurs. [Internet]. 2011; 29(9):531-8. doi: 10.1097/NCN.0b013e31821a166e
https://doi.org/10.1097/NCN.0b013e31821a...
) . Subsequently, the EQI Toolkit has attempted to incorporate all of the above competencies.
User assessment and regional variation
As part of the evaluation process, all four international reviewers answered questions using the Cognitive Debriefing Form (Figure 3) addressing strengths/weaknesses, clarity, ease of understanding, and relevance of the toolkit to their specific school/program. The overall impression was that the toolkit was easy to understand, user-friendly and relevant. Identified strengths were: use of a defined model for QI, the inclusion of structure, process and outcome as evaluation criteria, clearly stated definitions, and material that was relevant and up-to-date. Reviewers recommended expanding description of the PDSA cycle and strengthening linkages between the QI model and midwifery education. All reviewers suggested making the toolkit more culturally specific to their region, and tailoring or refinement of case studies. Minor modifications to wording and additional examples were offered to reduce ambiguity.
Components of final EQI Toolkit
The toolkit includes an introduction to and definitions of UH, PHC, and IPCP concepts based upon WHO(66 World Health Organization. The world health report 2008: Primary health care (now more than ever). Geneva: World Health Organization. [Internet]. 2008 [cited Jun 30, 2018]. Available from: https://www.who.int/whr/2008/en/
https://www.who.int/whr/2008/en/...
) and PAHO(55 Pan American Health Organization. Strategy for universal access to health and universal health coverage. [CD53.R14]. Washington, D.C.: PAHO. [Internet]. 2014 [cited Feb 11, 2017]. Available from: http://www.paho.org/uhexchange/index.php/en/uhexchange-documents/technical-information/26-strategy-for-universal-access-to-health-and-universal-health-coverage/file
http://www.paho.org/uhexchange/index.php...
) documents. An overview of nursing and midwifery education presents the core competencies for educators(99 World Health Organization. Midwifery Educator Core Competencies. Geneva: World Health Organization. [Internet]. 2014 [cited June 30, 2018]. Available from: https://www.who.int/hrh/nursing_midwifery/educator_competencies/en/
https://www.who.int/hrh/nursing_midwifer...
-1010 World Health Organization. Nurse Educator Competencies. Geneva: WHO. [Internet]. 2016 [cited Aug 1, 2018]. Available from: http://www.who.int/hrh/nursing_midwifery/nurse_educator050416.pdf
http://www.who.int/hrh/nursing_midwifery...
), followed by an introduction of QI in nursing and midwifery education. The expert group adopted the Model for Improvement (MFI) as the operational model for educational QI due to its widespread use and relative simplicity for end users. The MFI is described as a systematic method to effectively identify weaknesses or gaps in educational structures, processes, and outcomes. Starting with organizing a team to tackle the improvements and assess the current state, the MFI progresses to a series of questions that lead to an aim statement of what is to be accomplished. Measures are presented along with a strategy to determine whether an improvement has been made, identification of changes that may be tested to accomplish improvements, and iterative PDSA cycles to evaluate changes. The last step is how to sustain the change(s) and perhaps scale it to other programs or schools. Both the MFI and the PDSA cycles are depicted in Figure 5.
Model for Improvement and PDSA Cycle with steps
Used with permission from Moen R, and Norman CL. Source: Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2.ed. San Francisco: Jossey-Bass Publishers; 2009. p. 24.
To accomplish the MFI and PDSA steps, six tools were incorporated as appendices to the toolkit. First, an instrument was developed for schools of nursing and midwifery to assess program components representing areas of excellence, as well as opportunities for improvement, specific to UH and PHC. The “Universal Health and Primary Health Care in Nursing & Midwifery Education: A Self-Assessment QI Tool” is envisioned for use in conjunction with other available tools to assess the current state. Using ‘yes’ or ‘no’ responses to statements, Part one of the tool assesses items related to the school’s structure, including mission, objectives and philosophy, as well as resources, infrastructure, external relationships and policies. Part two covers 14 items evaluating students’ and graduates’ professional competencies addressed in the curriculum, followed by 8 items related to curriculum model, teaching and learning strategies. Part three includes 6 items to evaluate the school, program and faculty outcomes, followed by guidance for tallying total scores.
Second, a “Prioritization Matrix” along with a completed example were included. Together, these items assist the improvement team to prioritize up to three items/areas requiring improvement, stemming from the results of the previously described self-assessment tool. The matrix guides the team in using weighed criteria to score improvement project options and use criteria-based evidence when choosing those to begin first. Priority criteria can be tailored for each school/program; cost, expertise, space, location, and organizational culture are some of the most frequently encountered.
Third, a “PDSA Cycle Worksheet” consisting of four sections along with a completed example was provided. The first section, “Plan”, asks the improvement team to detail the plan for a test of change; the improvement to be implemented, who will be involved, what are the components of the change, when will the change begin and end, where the project will occur, and predictions regarding the change. The team is asked to define all measures (process, outcome, balancing and system measures), name their data source and frequency of measure, and assign responsibilities. The second section, “Do”, reminds the team to determine the number of participants, carry out the change or test and collect planned data, while documenting problems and unexpected observations. In the third section, “Study”, improvement team members are guided to analyze data and summarize lessons learned, then compare data to a priori predictions and reflect on what was learned. Last, in the “Act” section, the team is prompted to refine the change based on what was learned, and consider whether to adapt, adopt, or abandon the change.
The fourth appendix includes two improvement exemplars for teaching UH and PHC competencies. The first one is a completed MFI/PDSA project illustrating an interprofessional team-based immersive simulation. It exemplifies language for problem statement, aim, measures, test of change (delivery of an interprofessional team), detailed project plan, and report of findings from the PDSA cycles. The second example offers an improvement project ready to be adapted and tested. Learning objectives, scenarios, questions to stimulate discussion, and prompts helping end users adapt the project to their courses are included.
The last two appendices of the EQI Toolkit represent the group’s collective knowledge, experience, and multicultural awareness. An extensive list of freely available web-based QI resources for nursing and midwifery educators and administrators was compiled. Special emphasis was given to resources from the LAC region by searching through the LILACS database, a comprehensive index of scientific and technical literature from Latin America and the Caribbean. Also, a glossary of terms with definitions of main concepts covered in the EQI Toolkit and relevant references was included to enhance understanding and clarity.
International reviewers were positive about using the QI process to evaluate their nursing programs, particularly if they didn’t currently use a standardized data collection and evaluation method. All reviewers suggested changes to make the toolkit more specific to the educational structure and culture of their region. Content was added to address the variation in nursing, nurse midwifery, and midwifery programs across LAC countries. Wording was changed to reflect cultural nuances and a PHC relevant case study was translated, culturally adapted, and applied to the PDSA model, addressing IPCP and nursing/midwifery competencies. During the last phase, a reconciliation list of QI resources was developed for final review and input with effort on including LAC specific resources in Spanish and/or Portuguese. Overall, feedback strengthened the usability of the toolkit.
Discussion
The final EQI Toolkit is freely available through the UAB School of Nursing website(4343 University of Alabama at Birmingham School of Nursing & Pan American Health Organization. A plan for nursing & midwifery education quality improvement in universal health and primary health care. [Internet] [cited Sep 30 2019]; 2019. Available from: https://www.uab.edu/nursing/home/images/OCGP/PAHO-WHO/QI-Toolkit-Joint-Publication.pdf
https://www.uab.edu/nursing/home/images/...
). Ultimately, the toolkit’s endorsement will be a measure of its comprehensiveness, relevance, and adaptability to different settings, institutions, and countries. Extension of its use to other types of programs, such as graduate, post-graduate, and interdisciplinary could signal greater adaptability and inclusiveness. Its potential for better educational outcomes and systematic QI is highly anticipated. Given that currently there is no mandatory accreditation for most nursing and midwifery programs in LAC countries, the EQI Toolkit could serve as a guide for institutions towards developing standards and procedures for ongoing, systematic internal quality control and improvement. Key higher education stakeholders can play an important role by providing strong incentives and building capacity at multiple levels (e.g., among individual faculty, interprofessional teams, across schools and institutions). Examples include QI education and training, technical assistance, ongoing mentoring or coaching, and financial support towards QI infrastructure development and staff. Improvement science coursework could also be introduced to undergraduate students.
Learning the science and application of improvement is becoming more pertinent to nurses and midwives around the globe. The Nursing Now(88 Nursing Now Campaign. [Internet]. 2018 [cited May 1, 2018]. Available from: http://www.nursingnow.org/our-aims/; http://www.nursingnow.org/programmes/
http://www.nursingnow.org/our-aims/...
) global campaign has recently teamed up with the Institute for Healthcare Improvement (IHI) Open School to offer several free online modules on QI, program management, and culture change(4343 University of Alabama at Birmingham School of Nursing & Pan American Health Organization. A plan for nursing & midwifery education quality improvement in universal health and primary health care. [Internet] [cited Sep 30 2019]; 2019. Available from: https://www.uab.edu/nursing/home/images/OCGP/PAHO-WHO/QI-Toolkit-Joint-Publication.pdf
https://www.uab.edu/nursing/home/images/...
-4444 Institute for Healthcare Improvement (IHI). Open School. Supporting nurses and midwives across the globe to develop knowledge and skills in leading change. [Internet]. 2018 [cited May 17, 2018]. Available from: http://www.ihi.org/education/IHIOpenSchool/Courses/Pages/Nursing-Now.aspx
http://www.ihi.org/education/IHIOpenScho...
). Although mostly targeting the healthcare environment, introductory and intermediate modules aim to build fundamental QI knowledge and skills in becoming a change agent. According to campaign leaders, nurses and midwives are well positioned to make innovative changes that not only improve their work practice environment, but also shift the universal health paradigm. After piloting and further refinement, LAC schools of nursing and midwifery could use this toolkit to improve capacity for preparing future professionals, according to their country and national health system needs. Long-term, the toolkit could perhaps, guide strategic planning initiatives and future directives for undergraduate programs and schools.
The EQI Toolkit was developed using a systematic and iterative process. Upon identifying relevant evidence-based literature from the LAC region, online resources stemming from professional associations, organizations and institutes were compiled into an accompanying appendix. Completeness and accuracy of data were assessed through: 1) reaching consensus after several iterations, 2) choosing expert group members and reviewers based on diverse perspectives and technical expertise, and 3) indirectly asking reviewers to endorse the content and providing them the final draft before its release. Cognitive debriefing revealed some strong positive comments in support of the developed plan for QI. Nevertheless, certain limitations exist. Systematic literature review was limited to English language articles with full-text availability, published within the last 10 years. All included articles were appraised at a low level of evidence indicating a deficit in available rigorous evidence. Pilot testing of the EQI Toolkit was not within this project’s scope and is planned for the future. Translation and linguistic adaptation into Spanish and Portuguese would be required to broaden the toolkit’s reach, once the original English version has been sufficiently pilot tested and refined. Further cultural and organizational adaptation to each country and/or setting is needed to tailor and refine the toolkit.
Conclusions
Strengthening UH and PHC through transformative education has been at the core of a PAHO/WHO “call for action” for preparing a competent global nursing and midwifery workforce. Building capacity in LAC countries, many with low ratios of nurses and midwives to population and great variation of professional entry-level education, is paramount. Based on a systematic review of available literature, and recognizing that substantial educational differences occur among programs, the EQI toolkit is poised to be adaptable to individual characteristics or circumstances within any nursing or midwifery undergraduate school program. The toolkit offers a dynamic model for a QI plan that could be adopted by educational programs in LAC countries to address weaknesses in UH and PHC within the framework of transformative education and IPCP. Inherent in this work is the acknowledgement that nurses and midwives have important leadership roles to play in health promotion, disease prevention, and reducing morbidity and mortality. A strength of this toolkit stems from its development in partnership with international stakeholders. Future activities will focus on how this educational intervention can be disseminated, evaluated and further improved for broader application.
Aknowledgements
We would like to thank the following individuals, associated with the PAHO/WHO Collaborating Center for Development of Professional Nursing; School of Nursing and Midwifery of the Autonomous University of Mexico, who contributed a case study for the toolkit: Angélica Ramírez Elías, Professor; Angelina Rivera Montiel, Professor; Leticia Hernández Rodríguez, Professor, Academy of Obstetrics; Micaela López Maldonado, Perinatal Nurse Specialist and Professor, Academy of Obstetrics.
Also, Ms. Rebecca Billings, Assistant Professor, Reference Department / UAB Libraries for her assistance with the literature search to identify and map existing QI resources. Last, Ms. Silvia Gisiger Camata, Program Director, Office of Research and Scholarship at the UAB School of Nursing for reviewing and editing the Portuguese version of this article.
References
-
1Cassiani SHDB, Wilson LL, Mikael SSE, Morán-Peña L, Zarate-Grajales R, McCreary LL, et al. The situation of nursing education in Latin America and the Caribbean towards universal health. Rev. Latino-Am. Enfermagem. 2017;25:e2913. doi: 10.1590/1518-8345.2232.2913
» https://doi.org/10.1590/1518-8345.2232.2913 -
2Frenk J, Chen L, Bhutta AZ, Cohen J, Crisp N, Evans T, et al. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet. 2010 [cited Dec 17, 2016];376(9756):1923-58. doi: 10.1016/S0140-6736(10)61854-5
» https://doi.org/10.1016/S0140-6736(10)61854-5 -
3World Health Organization. Framework for action on interprofessional education & collaborative practice. [WHO/HRH/HPN/10.3]. [Internet]. Geneva; 2010 [cited Dec 14, 2016]. Available from: http://whqlibdoc.who.int/hq/2010/WHO_HRH_HPN_10.3_eng.pdf
» http://whqlibdoc.who.int/hq/2010/WHO_HRH_HPN_10.3_eng.pdf -
4World Health Organization, High-Level Commission on Health Employment and Economic Growth. Working for health and growth: Investing in the health workforce. Geneva: World Health Organization. [Internet]. 2016 [cited Jan 22, 2017]. Available from: http://www.who.int/hrh/com-heeg/reports/en/
» http://www.who.int/hrh/com-heeg/reports/en/ -
5Pan American Health Organization. Strategy for universal access to health and universal health coverage. [CD53.R14]. Washington, D.C.: PAHO. [Internet]. 2014 [cited Feb 11, 2017]. Available from: http://www.paho.org/uhexchange/index.php/en/uhexchange-documents/technical-information/26-strategy-for-universal-access-to-health-and-universal-health-coverage/file
» http://www.paho.org/uhexchange/index.php/en/uhexchange-documents/technical-information/26-strategy-for-universal-access-to-health-and-universal-health-coverage/file -
6World Health Organization. The world health report 2008: Primary health care (now more than ever). Geneva: World Health Organization. [Internet]. 2008 [cited Jun 30, 2018]. Available from: https://www.who.int/whr/2008/en/
» https://www.who.int/whr/2008/en/ -
7World Health Organization. Operations manual for staff at primary health care centres. Geneva: World Health Organization. [Internet]. 2008 [cited May 17, 2018]; p. 282. Available from: http://www.who.int/hiv/pub/imai/om.pdf
» http://www.who.int/hiv/pub/imai/om.pdf -
8Nursing Now Campaign. [Internet]. 2018 [cited May 1, 2018]. Available from: http://www.nursingnow.org/our-aims/; http://www.nursingnow.org/programmes/
» http://www.nursingnow.org/our-aims/» http://www.nursingnow.org/programmes/ -
9World Health Organization. Midwifery Educator Core Competencies. Geneva: World Health Organization. [Internet]. 2014 [cited June 30, 2018]. Available from: https://www.who.int/hrh/nursing_midwifery/educator_competencies/en/
» https://www.who.int/hrh/nursing_midwifery/educator_competencies/en/ -
10World Health Organization. Nurse Educator Competencies. Geneva: WHO. [Internet]. 2016 [cited Aug 1, 2018]. Available from: http://www.who.int/hrh/nursing_midwifery/nurse_educator050416.pdf
» http://www.who.int/hrh/nursing_midwifery/nurse_educator050416.pdf -
11World Health Organization. Global Standards for the initial education of professional nurses and midwives [WHO/HRH/HPN/08.6]. Geneva: WHO. [Internet]. 2009 [cited Dec 18, 2016]. Available from: http://www.who.int/hrh/nursing_midwifery/hrh_global_standards_education.pdf
» http://www.who.int/hrh/nursing_midwifery/hrh_global_standards_education.pdf -
12Carpio C, Bench NS. The Health Workforce in Latin America and the Caribbean: An analysis of Colombia, Costa Rica, Jamaica, Panama, Peru and Uruguay. World Bank Group. [Internet]. 2015 [cited Jun 30, 2018]. Available from: http://dx.doi.org/10.1596/978-1-4648-0594-3
» http://dx.doi.org/10.1596/978-1-4648-0594-3 -
13Luyben A, Barger M, Avery M, Bharj KK, O’connel R, Fleming V, et al. Exploring global recognition of quality midwifery education: Vision or fiction? Women and Birth. 2017 Jun; 30(3):184-92. doi: 10.1016/j.wombi.2017.03.001
» https://doi.org/10.1016/j.wombi.2017.03.001 -
14Pan American Health Organization. Toolkit for strengthening professional midwifery in the Americas. Washington, D.C.: PAHO. [Internet]. 2014 [cited Sep 7, 2018]. Available from: https://www.paho.org/clap/index.php?option=com_docman&view=download&category_slug=salud-de-mujer-reproductiva-materna-y-perinatal&alias=427-toolkit-for-strengthening-professional-midwifery-in-the-americas-3-ed-1&Itemid=219&lang=es
» https://www.paho.org/clap/index.php?option=com_docman&view=download&category_slug=salud-de-mujer-reproductiva-materna-y-perinatal&alias=427-toolkit-for-strengthening-professional-midwifery-in-the-americas-3-ed-1&Itemid=219&lang=es -
15Shewhart WA. Statistical Method from the Viewpoint of Quality Control. Department of Agriculture. [Internet]. 1986 [cited June 30, 2018]; p. 45. Available from: https://archive.org/details/CAT10502416
» https://archive.org/details/CAT10502416 -
16Devers KJ. The state of quality improvement science in health: What do we know about how to provide better care? Robert Wood Johnson Foundation & Urban Institute. [Internet]. 2011 Nov [cited June 30, 2018]. Available from: https://www.rwjf.org/en/library/research/2011/11/the-state-of-quality-improvement-science-in-health.html
» https://www.rwjf.org/en/library/research/2011/11/the-state-of-quality-improvement-science-in-health.html -
17U. S. Department of Health and Human Services - Health Resources and Services Administration. Quality Improvement. Washington, D.C. [Internet]. 2011 [cited Aug 1, 2018]. Available from: https://www.hrsa.gov/sites/default/files/quality/toolbox/508pdfs/qualityimprovement.pdf
» https://www.hrsa.gov/sites/default/files/quality/toolbox/508pdfs/qualityimprovement.pdf -
18Institute of Medicine. Crossing the quality chasm: A new health system for the 21st Century Committee on Quality of Health Care in America, ed. N.A. Press; Washington, DC. IOM. [Internet]. 2001 [cited Aug 1, 2018]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25057539
» https://www.ncbi.nlm.nih.gov/pubmed/25057539 -
19Donabedian A. Evaluating the quality of medical care. Milbank Mem Fund Q. 1966;44 (Suppl):166-206. doi: 10.2307/3348969
» https://doi.org/10.2307/3348969 -
20Dartmouth College - Sheffield Microsystem Coaching Academy. Brainstorming, Affinity Grouping and Multivoting ‘A one page book’. [Internet]. 2014 [cited Aug 1, 2018]. Available from: http://www.sheffieldmca.org.uk/UserFiles/File/Brainstorming_one_page_book_V2.pdf
» http://www.sheffieldmca.org.uk/UserFiles/File/Brainstorming_one_page_book_V2.pdf -
21Melnyk BM, Fineout-Overhold E. Evidence-based practice in nursing and healthcare: a guide to best practice. 2ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams and Wilkins; 2011.
-
22Andresen K, Levin P. Enhancing quantity and quality of clinical experiences in a baccalaureate nursing program. Int J Nurs Educ Scholarsh. 2014;11(1):1-8. doi: 10.1515/ijnes-2013-0053
» https://doi.org/10.1515/ijnes-2013-0053 -
23Armstrong GE, Spencer TS, Lenburg CB. Using quality and safety education for nurses to enhance competency outcome performance assessment: A synergistic approach that promotes patient safety and quality outcomes. J Nurs Educ. 2009;48(12):686-93. doi: 10.3928/01484834-20091113-02
» https://doi.org/10.3928/01484834-20091113-02 -
24Brown JF, Marshall BL. Continuous quality improvement: An effective strategy for improvement of program outcomes in a higher education setting. Nurs Educ Perspect. [Internet]. 2008 [cited June 30, 2018];29(4):205-11. Available from: https://www.ncbi.nlm.nih.gov/pubmed/18770948
» https://www.ncbi.nlm.nih.gov/pubmed/18770948 -
25Coffman S, Doolen J, Llasus L. Program development and evaluation of the concierge model of simulation. Online J Nurs Informatics. [Internet]. 2015 [cited Aug 1, 2018];19(2):8-8. Available from: https://www.himss.org/program-development-and-evaluation-concierge-model-simulation
» https://www.himss.org/program-development-and-evaluation-concierge-model-simulation -
26Ellis P, Halstead J. Understanding the commission on collegiate nursing education accreditation process and the role of the continuous improvement progress report. J Prof Nurs. 2012; 28(1):18-26. doi: 10.1016/j.profnurs.2011.10.004
» https://doi.org/10.1016/j.profnurs.2011.10.004 -
27Escallier LA, Fullerton JT. An innovation in design of a school of nursing evaluation protocol. Nurse Educator. 2012;37(5):187-91. doi: 10.1097/NNE.0b013e318262eb15
» https://doi.org/10.1097/NNE.0b013e318262eb15 -
28Fater KH. Gap analysis: A method to assess core competency development in the curriculum. Nurs Educn Perspect. 2013; 34(2):101-5. doi: 10.5480/1536-5026-34.2.101
» https://doi.org/10.5480/1536-5026-34.2.101 -
29González-Chordá VM, Maciá-Soler ML. Evaluation of the quality of the teaching-learning process in undergraduate courses in Nursing. Rev. Latino-Am. Enfermagem. 2015; 23(4):700-7. doi: 10.1590/0104-1169.0393.2606
» https://doi.org/10.1590/0104-1169.0393.2606 -
30Halstead JA. The value of nursing program accreditation. Teach Learn Nurs. [Internet]. 2017; 12(3):181-2. doi: 10.1016/j.teln.2017.03.005
» https://doi.org/10.1016/j.teln.2017.03.005 -
31Hooper JI, Ayars VD. How Texas nursing education programs increased NCLEX pass rates and improved programming. J Nurs Regulation. [Internet]. 2017; 8(3):53-8. doi: 10.1016/S2155-8256(17)30160-6
» https://doi.org/10.1016/S2155-8256(17)30160-6 -
32James B, Beattie M, Shepherd A, Armstrong L, Wilkinson J. Time, fear and transformation: Student nurses’ experiences of doing a practicum (quality improvement project) in practice. Nurse Educ Practice. 2016; 19:70-8. doi: 10.1016/j.nepr.2016.05.004
» https://doi.org/10.1016/j.nepr.2016.05.004 -
33Kaplan BG, Holmes L, Mott M, Atallah H. Design and implementation of an interdisciplinary pediatric mock code for undergraduate and graduate nursing students. Comput Inform Nurs. [Internet]. 2011; 29(9):531-8. doi: 10.1097/NCN.0b013e31821a166e
» https://doi.org/10.1097/NCN.0b013e31821a166e -
34Karagory PM, McComb S. Measuring the vital signs of the health care system with the first clinical experience: Sophomore nursing students rise to the challenge. J Nurs Educ. 2014; 53:S97-S100. doi: 10.3928/01484834-20140806-01
» https://doi.org/10.3928/01484834-20140806-01 -
35McComb SA, Kirkpatrick JM. Infusing systems and quality improvement throughout an undergraduate nursing curriculum. J Nurs Educ. 2017;56(12):752-7. doi: 10.3928/01484834-20171120-10
» https://doi.org/10.3928/01484834-20171120-10 -
36Nugent E, LaRocco S. Comprehensive review of an accelerated nursing program: A quality improvement project. Dimens Crit Care Nurs. 2014; 33(4):226-33. doi: 10.1097/DCC.0000000000000054
» https://doi.org/10.1097/DCC.0000000000000054 -
37Posey L, Pintz C. Transitioning a bachelor of science in nursing program to blended learning: Successes, challenges & outcomes. Nurse Educ Practice. 2017; 26:126-33. doi: 10.1016/j.nepr.2016.10.006
» https://doi.org/10.1016/j.nepr.2016.10.006 -
38Santos M. The role of nursing education in the transformation of the U.S. health system. Online Braz J Nurs. 2012; 11(2):257-60. doi: 10.5935/1676-4285.20120024
» https://doi.org/10.5935/1676-4285.20120024 -
39Seibert SA. Safety consciousness: Assignments that expand focus beyond the bedside. Nurse Educ Today. 2014;34(2):233-6. doi: 10.1016/j.nedt.2013.08.002
» https://doi.org/10.1016/j.nedt.2013.08.002 -
40Sherrod RA, Morrison RS. Leadership experiences for baccalaureate nursing students: Improving quality in a nurse-managed rural health clinic. Nurs Educ Perspectives. [Internet]. 2008 [cited Sept 29, 2018];29(4):212-216. Available from: https://wwww.unboundmedicine.com/medline/citation/18770949/Leadership_experiences_for_baccalaureate_nursing_students:_improving_quality_in_a_nurse_managed_rural_health_clinic_
» https://wwww.unboundmedicine.com/medline/citation/18770949/Leadership_experiences_for_baccalaureate_nursing_students:_improving_quality_in_a_nurse_managed_rural_health_clinic_ -
41Wassef ME, Riza L, Maciag T, Worden C, Delaney A. Implementing a competency-based electronic portfolio in a graduate nursing program. Comput Inform Nurs. 2012; 30(5):242-8. doi: 10.1097/NXN.0b013e31824af6d4.
» https://doi.org/10.1097/NXN.0b013e31824af6d4 -
42Wolf ZR, Czekanski KE. Analyzing student complaints against nursing programs: taxonomies of complaints and outcomes. J Prof Nurs. 2011 Sep-Oct; 27(5):283-91. doi: 10.1016/j.profnurs.2011.06.00443.
» https://doi.org/10.1016/j.profnurs.2011.06.00443 -
43University of Alabama at Birmingham School of Nursing & Pan American Health Organization. A plan for nursing & midwifery education quality improvement in universal health and primary health care. [Internet] [cited Sep 30 2019]; 2019. Available from: https://www.uab.edu/nursing/home/images/OCGP/PAHO-WHO/QI-Toolkit-Joint-Publication.pdf
» https://www.uab.edu/nursing/home/images/OCGP/PAHO-WHO/QI-Toolkit-Joint-Publication.pdf -
44Institute for Healthcare Improvement (IHI). Open School. Supporting nurses and midwives across the globe to develop knowledge and skills in leading change. [Internet]. 2018 [cited May 17, 2018]. Available from: http://www.ihi.org/education/IHIOpenSchool/Courses/Pages/Nursing-Now.aspx
» http://www.ihi.org/education/IHIOpenSchool/Courses/Pages/Nursing-Now.aspx
Publication Dates
-
Publication in this collection
05 Dec 2019 -
Date of issue
2019
History
-
Received
20 Jan 2019 -
Accepted
04 June 2019