ABSTRACT
BACKGROUND:
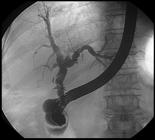
Hepatobiliary surgery and hepatic trauma are frequent causes of bile leaks and this feared complication can be safely managed by endoscopic retrograde cholangiopancreatography (ERCP). The approach consists of sphincterotomy alone, biliary stenting or a combination of the two but the optimal form remains unclear.
OBJECTIVE:
The aim of this study is to compare sphincterotomy alone versus sphincterotomy plus biliary stent placement in the treatment of post-surgical and traumatic bile leaks.
METHODS:
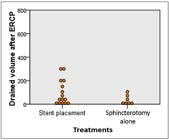
We retrospectively analyzed 31 patients with the final ERCP diagnosis of “bile leak”. Data collected included patient demographics, etiology of the leak and the procedure details. The treatment techniques were divided into two groups: sphincterotomy alone vs. sphincterotomy plus biliary stenting. We evaluated the volume of the abdominal surgical drain before and after each procedure and the number of days needed until cessation of drainage post ERCP.
RESULTS:
A total of 31 patients (18 men and 3 women; mean age, 51 years) with bile leaks were evaluated. Laparoscopic cholecystectomy was the etiology of the leak in 14 (45%) cases, followed by conventional cholecystectomy in 9 (29%) patients, hepatic trauma in 5 (16%) patients, and hepatectomy secondary to neoplasia in 3 (9.7%) patients. The most frequent location of the leaks was the cystic duct stump with 12 (38.6%) cases, followed by hepatic common duct in 10 (32%) cases, common bile duct in 7 (22%) cases and the liver bed in 2 (6.5%) cases. 71% of the patients were treated with sphincterotomy plus biliary stenting, and 29% with sphincterotomy alone. There was significant difference between the volume drained before and after both procedures (P<0.05). However, when comparing sphincterotomy alone and sphincterotomy plus biliary stenting, regarding the volume drained and the days needed to cessation of drainage, there was no statistical difference in both cases (P>0.005).
CONCLUSION:
ERCP remains the first line treatment for bile leaks with no difference between sphincterotomy alone vs sphincterotomy plus stent placement.
HEADINGS:
Fístula biliar; Sphincterotomy; Stents; Endoscopic retrograde cholangiopancreatography; Cholecystectomy

 Thumbnail
Thumbnail
 Thumbnail
Thumbnail
 Thumbnail
Thumbnail
 Thumbnail
Thumbnail
 Thumbnail
Thumbnail
 Thumbnail
Thumbnail





